Genetics and Prenatal Development
This text was last updated as of January 16, 2023 and is no longer being maintained by the author. The current version Psychology Through the Lifespan is available for use.
Why learn about prenatal development and genetics?
People endure quite an incredible journey before they are born. Think about it—when the timing and conditions are just right, a tiny egg releases from ovulation and a single sperm out of hundreds of millions unite to begin the process of fertilization. Genetic material from the mother and father join together to form a completely new organism. This new organism has to continue to travel and implant in the uterine wall in order to continue to grow and thrive. It is not an easy feat. It still must grow and develop for approximately 268 days before it begins life outside of the womb.
Today we have more knowledge and technology than ever before that has an impact on this process. We are privy to tests that can give us a wealth of information even before we conceive. We have the ability to know the genetic make-up of an embryo before it is implanted in the womb. If you could choose all of the features of your future baby, would you? What would be the pros and cons of this? New parents also have the choice of the prenatal care that they receive and how they want to prepare for labor and delivery. As you can see, the choices that are made along the way and the unforeseen surprises make for a unique pregnancy and birth story.
This module explores this journey and the development process from the moment of conception to delivery.
What you’ll learn to do: explain the role of genetics in prenatal development
In this section, we will look at some of the ways in which heredity helps to shape the way we are. Heredity involves more than genetic information from our parents. According to evolutionary psychology, our genetic inheritance comes from the most adaptive genes of our ancestors. We will look at what happens genetically during conception and take a brief look at some genetic abnormalities. Before going into these topics, however, it is important to emphasize the interplay between heredity and the environment. Why are you the way you are? As you consider some of your features (height, weight, personality, health, etc.), ask yourself whether these features are a result of heredity, or environmental factors, or both. Chances are, you can see the ways in which both heredity and environmental factors (such as lifestyle, diet, and so on) have contributed to these features.
Learning outcomes
- Explain the evolutionary psychology perspective of lifespan development
- Describe genetic components of conception
- Describe genes and their importance in genetic inheritance
- Describe chromosomal abnormalities
- Explain the value of prenatal testing
- Describe the interaction between genetics and the environment
- Compare monozygotic and dizygotic twins
Evolutionary Psychology
Evolutionary Psychology

Evolutionary psychology focuses on how universal patterns of behavior and cognitive processes have evolved over time. Variations in cognition and behavior would make individuals more or less successful in reproducing and passing those genes to their offspring. Evolutionary psychologists study a variety of psychological phenomena that may have evolved as adaptations, including the fear response, food preferences, mate selection, and cooperative behaviors (Confer et al., 2010).
Many think of evolution as the development of traits and behaviors that allow us to survive this “dog-eat-dog” world, like strong leg muscles to run fast, or fists to punch and defend ourselves. However, physical survival is only important if it eventually contributes to successful reproduction. That is, even if you live to be 100 years old if you fail to mate and produce children, your genes will die with your body. Thus, reproductive success, not survival success, is the engine of evolution by natural selection.
Charles Darwin describes this process in the theory of evolution by natural selection. In simple terms, the theory states that organisms that are better suited for their environment will survive and reproduce, while those that are poorly suited for their environment will die off. There is a growing interest in applying the principles of evolutionary psychology to better understand lifespan development in humans.
The Evolutionary Perspective: Genetic Inheritance from our Ancestors
The fundamentals of the evolutionary perspective

Evolutionary psychology has its historical roots in Charles Darwin’s theory of natural selection. In The Origin of Species, Darwin predicted that psychology would develop an evolutionary basis and that a process of natural selection creates traits in a species that is adaptive to its environment.
Using Darwin’s arguments, evolutionary approaches claim that one’s genetic inheritance not only determine such physical traits as skin and eye color, but also certain personality traits and social behaviors. For example, some evolutionary developmental psychologists suggest that behavior such as shyness and jealousy may be produced in part by genetic causes, presumably because they helped increase the survival rates of human’s ancient relatives.
Lifespan Development and Evolutionary Psychology
As we consider development from conception through the lifespan, there will be many opportunities to understand how evolutionary psychology enhances our understanding of development. For instance, women and men do differ in their preferences for a few key qualities in long-term mating, because of somewhat distinct adaptive concerns. Modern women have inherited the evolutionary trait to desire mates who possess resources, have qualities linked with acquiring resources (e.g., ambition, wealth, industriousness), and are willing to share those resources with them. On the other hand, men more strongly desire youth and health in women, as both are cues to fertility. These male and female differences have historically been universal in humans.
Just because a psychological adaptation was advantageous in our history, does not mean it’s still useful today. For example, even though women may have preferred men with resources in previous generations, our modern society has advanced such that these preferences are no longer necessary. Nonetheless, it’s important to consider how our evolutionary history has shaped our automatic or “instinctual” desires and reflexes of today so that we can better shape them for the future ahead.
As we follow the journey of life, from conception to death, think about how the theory of natural selection and the concepts of evolutionary psychology can enlighten our understanding of why some automatic reflexes or instinctual desires are more common than others. Remember that the end product of the theory of evolution by natural selection is successful survival and reproduction. Can you think of some ways that the ultimate goal of reproductive success affects our selection of a mate, how we parent young children, why we are motivated to achieve certain goals, or what differentiates families with traditionally longer lifespans? In order to achieve reproductive success, the theory of evolution by natural selection states that organisms should be suited to their environment. Think about how different environments or cultures require different traits for successful survival and reproduction. Can you think of some ways that we may be changing to be better suited to our changing culture?
Link to Learning
David Buss is one of the leading researchers in evolutionary psychology. In David Buss’s Ted Talk, he explains several theories related to the selection of sexual partners, mating preferences, and infidelity.
Heredity and Chromosomes
Gametes
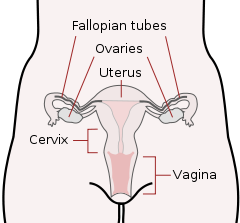
There are two types of sex cells or gametes involved in reproduction: the male gametes, or sperm, and female gametes, or ova. The male gametes are produced in the testes through a process called spermatogenesis, which begins at about 12 years of age. The female gametes, which are stored in the ovaries, are present at birth but are immature. Each ovary contains about 250,000 ova but only about 400 of these will become mature eggs (Mackon & Fauser, 2000; Rome, 1998). Beginning at puberty, one ovum ripens and is released about every 28 days, a process called oogenesis.
After the ovum or egg ripens and is released from the ovary, it is drawn into the fallopian tube and in 3 to 4 days, reaches the uterus. It is typically fertilized in the fallopian tube and continues its journey to the uterus. At ejaculation, millions of sperm are released into the vagina, but only a few reach the egg and typically, only one fertilizes the egg. Once a single sperm has entered the wall of the egg, the wall becomes hard and prevents other sperm from entering. After the sperm has entered the egg, the tail of the sperm breaks off and the head of the sperm, containing the genetic information from the father, unites with the nucleus of the egg. As a result, a new cell is formed. This cell, containing the combined genetic information from both parents, is referred to as a zygote.
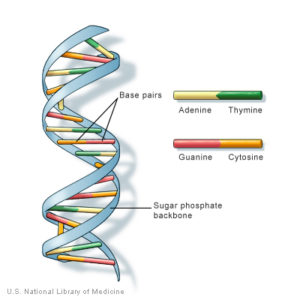
Chromosomes
While other normal human cells have 46 chromosomes (or 23 pairs), gametes contain 23 chromosomes. Chromosomes are long threadlike structures found in a cell nucleus that contains genetic material known as deoxyribonucleic acid (DNA). DNA is a helix-shaped molecule made up of nucleotide base pairs [adenine (A), guanine (G), cytosine (C), and thymine (T)]. In each chromosome, sequences of DNA make up genes that control or partially control a number of visible characteristics, known as traits, such as eye color, hair color, and so on. A single gene may have multiple possible variations or alleles. An allele is a specific version of a gene. So, a given gene may code for the trait of hair color, and the different alleles of that gene affect which hair color an individual has.
In a process called meiosis, segments of the chromosomes from each parent form pairs, and genetic segments are exchanged as determined by chance. Because of the unpredictability of this exchange, the likelihood of having offspring that are genetically identical (and not twins) is one in trillions (Gould & Keeton, 1997). Genetic variation is important because it allows a species to adapt so that those who are better suited to the environment will survive and reproduce, which is an important factor in natural selection.
Genotypes and Phenotypes
When a sperm and egg fuse, their 23 chromosomes pair up and create a zygote with 23 pairs of chromosomes. Therefore, each parent contributes half the genetic information carried by the offspring; the resulting physical characteristics of the offspring (called the phenotype) are determined by the interaction of genetic material supplied by the parents (called the genotype). A person’s genotype is the genetic makeup of that individual. Phenotype, on the other hand, refers to the individual’s inherited physical characteristics.
Look in the mirror. What do you see, your genotype or your phenotype? What determines whether or not genes are expressed? Actually, this is quite complicated. Some features follow the additive pattern which means that many different genes contribute to a final outcome. Height and skin tone are examples. In other cases, a gene might either be turned on or off depending on several factors, including the gene with which it is paired or the inherited epigenetic tags.
Link To learning
Visit the webpage “What are DNA and Genes?” from the University of Utah to better understand DNA and genes, then watch the video “What is Inheritance?” to learn how the genes from parents pass on genetic information to their children.
Determining the Sex of the Child
Twenty-two of those chromosomes from each parent are similar in length to a corresponding chromosome from the other parent. However, the remaining chromosome looks like an X or a Y. Half of the male’s sperm contains a Y chromosome and half contain an X. All of the ova contain X chromosomes. If the child receives the combination of XY, the child will be genetically male. If it receives the XX combination, the child will be genetically female.
Many potential parents have a clear preference for having a boy or a girl and would like to determine the sex of the child. Through the years, a number of tips have been offered for potential parents to maximize their chances of having either a son or daughter as they prefer. However, there is not much scientific evidence to back these claims. Today, however, there is new technology available called sperm sorting that makes it possible to isolate sperm containing either an X or a Y, depending on the preference, and use that sperm to fertilize a mother’s egg. Preimplantation genetic diagnosis (PGD) could also be used to select only embryos of the desired sex to be implanted during in-vitro fertilization (IVF). However, these methods are controversial and both fertility centers and medical organizations discourage it if there is no real medical reason to select gender.
Genetic Variation and Inheritance
Genetic variation, the genetic difference between individuals, is what contributes to a species’ adaptation to its environment. In humans, genetic variation begins with an egg, several million sperm, and fertilization. The egg and the sperm each contain 23 chromosomes, which make up our genes. A single gene may have multiple possible variations or alleles (a specific version of a gene), resulting in a variety of combinations of inherited traits.
Genetic inheritance of traits for humans is based upon Gregor Mendel’s model of inheritance. For genes on an autosome (any chromosome other than a sex chromosome), the alleles and their associated traits are autosomal dominant or autosomal recessive. In this model, some genes are considered dominant because they will be expressed. Others, termed recessive, are only expressed in the absence of a dominant gene. Some characteristics which were once thought of as dominant-recessive, such as eye color, are now believed to be a result of the interaction between several genes (McKusick, 1998). Dominant traits include curly hair, facial dimples, normal vision, and dark hair. Recessive characteristics include red hair, pattern baldness, and nearsightedness.
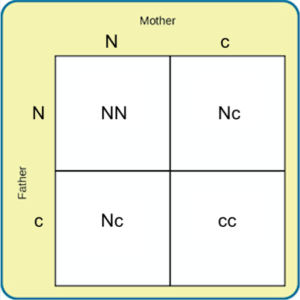
Sickle cell anemia is an autosomal recessive disease; Huntington’s disease is an autosomal dominant disease. Other traits are a result of partial dominance or co-dominance in which both genes are influential. For example, if a person inherits both recessive genes for cystic fibrosis, the disease will occur. But if a person has only one recessive gene for the disease, the person would be a carrier of the disease.
In this example, we will call the normal gene “N,” and the gene for cystic fibrosis “c.” The normal gene is dominant, which means that having the dominant allele either from one parent (Nc) or both parents (NN) will always result in the phenotype associated with the dominant allele. When someone has two copies of the same allele, they are said to be homozygous for that allele. When someone has a combination of alleles for a given gene, they are said to be heterozygous. For example, cystic fibrosis is a recessive disease which means that an individual will only have the disease if they are homozygous for that recessive allele (cc).
Imagine that a woman who is a carrier of the cystic fibrosis gene has a child with a man who also is a carrier of the same disease. What are the odds that their child would inherit the disease? Both the woman and the man are heterozygous for this gene (Nc). We can expect the offspring to have a 25% chance of having cystic fibrosis (cc), a 50% chance of being a carrier of the disease (Nc), and a 25% chance of receiving two normal copies of the gene (NN).
Where do harmful genes that contribute to diseases like cystic fibrosis come from? Gene mutations provide one source of harmful genes. A mutation is a sudden, permanent change in a gene. While many mutations can be harmful or lethal, once in a while a mutation benefits an individual by giving that person an advantage over those who do not have the mutation. Recall that the theory of evolution asserts that individuals best adapted to their particular environments are more likely to reproduce and pass on their genes to future generations. In order for this process to occur, there must be competition—more technically, there must be variability in genes (and resultant traits) that allow for variation in adaptability to the environment. If a population consisted of identical individuals, then any dramatic changes in the environment would affect everyone in the same way, and there would be no variation in selection. In contrast, diversity in genes and associated traits allow some individuals to perform slightly better than others when faced with environmental change. This creates a distinct advantage for individuals best suited for their environments in terms of successful reproduction and genetic transmission.
Link to Learning
Visit the Cystic Fibrosis Foundation to learn more about cystic fibrosis and learn how a mutation in DNA leads to the disease.
Chromosomal Abnormalities and Genetic Testing
Chromosomal Abnormalities
A chromosomal abnormality occurs when a child inherits too many or too few chromosomes. The most common cause of chromosomal abnormalities is the age of the mother. A 20-year-old woman has a 1 in 800 chance of having a child with a common chromosomal abnormality. A woman of 44, however, has a one in 16 chance. It is believed that the problem occurs when the ovum is ripening prior to ovulation each month. As the mother ages, the ovum is more likely to suffer abnormalities at this time.
Another common cause of chromosomal abnormalities occurs because the gametes do not divide evenly when they are forming. Therefore, some cells have more than 46 chromosomes. In fact, it is believed that close to half of all zygotes have an odd number of chromosomes. Most of these zygotes fail to develop and are spontaneously aborted by the body. If the abnormal number occurs on pair # 21 or # 23, however, the individual may have certain physical or other abnormalities.
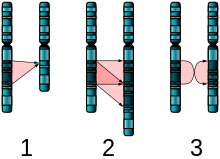
An altered chromosome structure may take several different forms, and result in various disorders or malignancies:
-
Deletions: A portion of the chromosome is missing or deleted. Known disorders in humans include Wolf-Hirschhorn syndrome, which is caused by partial deletion of the short arm of chromosome 4; and Jacobsen syndrome also called the terminal 11q deletion disorder.
- Duplications: A portion of the chromosome is duplicated, resulting in extra genetic material. Known human disorders include Charcot-Marie-Tooth disease type 1A, which may be caused by duplication of the gene encoding peripheral myelin protein 22 (PMP22) on chromosome 17.

Figure 6. The two major two-chromosome mutations: insertion (1) and Translocation (2). - Translocations: A portion of one chromosome is transferred to another chromosome. There are two main types of translocations:
- Reciprocal translocation: Segments from two different chromosomes have been exchanged.
- Robertsonian translocation: An entire chromosome has attached to another at the centromere – in humans, these only occur with chromosomes 13, 14, 15, 21, and 22.
- Inversions: A portion of the chromosome has broken off, turned upside down, and reattached, therefore the genetic material is inverted.
- Insertions: A portion of one chromosome has been deleted from its normal place and inserted into another chromosome.
- Rings: A portion of a chromosome has broken off and formed a circle or ring. This can happen with or without loss of genetic material.
- Isochromosome: Formed by the mirror image copy of a chromosome segment including the centromere.
One of the most common chromosomal abnormalities is on pair # 21. Trisomy 21 occurs when there are three rather than two chromosomes on #21. A person with Down syndrome has distinct facial features, intellectual disability, and oftentimes heart and gastrointestinal disorders. Symptoms vary from person to person and can range from mild to severe. With early intervention, the life expectancy of persons with Down syndrome has increased in recent years. Keep in mind that there is as much variation in people with Down Syndrome as in most populations and those differences need to be recognized and appreciated.
When the chromosomal abnormality is on pair #23, the result is a sex-linked chromosomal abnormality. A person might have XXY, XYY, XXX, XO, or 45 or 47 chromosomes as a result. Two of the more common sex-linked chromosomal disorders are Turner syndrome and Klinefelter syndrome. Turner’s syndrome occurs in 1 of every 2,500 live female births when an ovum that lacks a chromosome is fertilized by a sperm with an X chromosome (Carroll, 2007). The resulting zygote has an XO composition. Fertilization by a Y sperm is not viable. Turner syndrome affects cognitive functioning and sexual maturation. The external genitalia appear normal, but breasts and ovaries do not develop fully and the woman does not menstruate. Turner’s syndrome also results in short stature and other physical characteristics. Klinefelter syndrome (XXY) occurs in 1 out of 700 live male births and results when an ovum containing an extra X chromosome is fertilized by a Y sperm. The Y chromosome stimulates the growth of male genitalia, but the additional X chromosome inhibits this development. An individual with Klinefelter syndrome has some breast development, infertility (this is the most common cause of infertility in males), and has low levels of testosterone.
Prenatal Testing
Prenatal testing consists of prenatal screening and prenatal diagnosis, which are aspects of prenatal care that focus on detecting problems with the pregnancy as early as possible. These may be anatomic and physiologic problems with the health of the zygote, embryo, or fetus, either before gestation even starts or as early in gestation as practical. Prenatal screening focuses on finding problems among a large population with affordable and noninvasive methods. The most common screening procedures are routine ultrasounds, blood tests, and blood pressure measurement. Prenatal diagnosis focuses on pursuing additional detailed information once a particular problem has been found, and can sometimes be more invasive.
Screening can detect problems such as neural tube defects, anatomical defects, chromosome abnormalities, and gene mutations that would lead to genetic disorders and birth defects, such as spina bifida, cleft palate, Downs Syndrome, Tay–Sachs disease, sickle cell anemia, thalassemia, cystic fibrosis, muscular dystrophy, and fragile X syndrome. Some tests are designed to discover problems that primarily affect the health of the mother, such as PAPP-A to detect pre-eclampsia or glucose tolerance tests to diagnose gestational diabetes. Screening can also detect anatomical defects such as hydrocephalus, anencephaly, heart defects, and amniotic band syndrome.
Common prenatal diagnosis procedures include amniocentesis and chorionic villus sampling. Because of the miscarriage and fetal damage risks associated with amniocentesis and CVS procedures, many women prefer to first undergo screening so they can find out if the fetus’ risk of birth defects is high enough to justify the risks of invasive testing. Screening tests yield a risk score which represents the chance that the baby has the birth defect; the most common threshold for high-risk is 1:270. A risk score of 1:300 would, therefore, be considered low-risk by many physicians. However, the trade-off between the risk of birth defects and risk of complications from invasive testing is relative and subjective; some parents may decide that even a 1:1000 risk of birth defects warrant an invasive test while others wouldn’t opt for an invasive test even if they had a 1:10 risk score.
There are three main purposes of prenatal diagnosis: (1) to enable timely medical or surgical treatment of a condition before or after birth, (2) to give the parents the chance to abort a fetus with the diagnosed condition, and (3) to give parents the chance to prepare psychologically, socially, financially, and medically for a baby with a health problem or disability, or for the likelihood of stillbirth. Having this information in advance of birth means that healthcare staff, as well as parents, can better prepare themselves for the delivery of a child with a health problem. For example, Down Syndrome is associated with cardiac defects that may need intervention immediately upon birth.
The American College of Obstetricians and Gynecologists (ACOG) guidelines currently recommend that all pregnant women, regardless of age, be offered invasive testing to obtain a definitive diagnosis of certain birth defects. Therefore, most physicians offer diagnostic testing to all their patients, with or without prior screening, and let the patient decide.
Behavioral Genetics
Behavioral geneticists study how individual differences arise, in the present, through the interaction of genes and the environment. When studying human behavior, behavioral geneticists often employ twin and adoption studies to research questions of interest. Twin studies compare the rates that a given behavioral trait is shared among identical and fraternal twins; adoption studies compare those rates among biologically related relatives and adopted relatives. Both approaches provide some insight into the relative importance of genes and environment for the expression of a given trait.
The evolutionary perspective encompasses one of the fastest-growing areas within the field of lifespan development: behavioral genetics. Behavioral genetics is a field of scientific research that uses genetic methods to investigate the nature and origins of individual differences in behavior and studies the effects of heredity on behavior. Behavioral geneticists strive to understand how we might inherit certain behavioral traits and how the environment influences whether we actually displayed those traits. It also considers how genetic factors may influence psychological disorders such as schizophrenia, depression, and substance abuse.
Nature or Nurture?
For decades, scholars have carried on the “nature/nurture” debate. For any particular feature, those on the “nature” side would argue that heredity plays the most important role in bringing about that feature. Those on the “nurture” side would argue that one’s environment is most significant in shaping the way we are. This debate continues in questions about what makes us masculine or feminine (Lippa, 2002), concerns about vision (Mutti, Kadnik, & Adams, 1996), and many other developmental issues.
Most scholars agree that there is a constant interplay between the two forces. It is difficult to isolate the root of any single behavior as a result solely of nature or nurture, and most scholars believe that even determining the extent to which nature or nurture impacts a human feature is difficult to answer. In fact, almost all human features are polygenic (a result of many genes) and multifactorial (a result of many factors, both genetic and environmental). It is as if one’s genetic make-up sets up a range of possibilities, which may or may not be realized depending upon one’s environmental experiences. For instance, a person might be genetically predisposed to develop diabetes, but the person’s lifestyle may help bring about the disease.
When you think about your own family history, it is easy to see that there are certain personality traits, behavioral characteristics, and medical conditions that are more common than others. This is the reason that doctors ask you about your family medical history. While genetic predisposition is important to consider, there are some family members who, for a variety of reasons, seemed to defy the odds of developing these conditions. These differences can be explained in part by the effect of epigenetic (above the genome) changes.
The Epigenetic Framework
The term “epigenetic” has been used in developmental psychology to describe psychological development as the result of an ongoing, bi-directional interchange between heredity and the environment. Gottlieb (1998; 2000; 2002) suggests an analytic framework for the nature/nurture debate that recognizes the interplay between the environment, behavior, and genetic expression. This bidirectional interplay suggests that the environment can affect the expression of genes just as genetic predispositions can impact a person’s potentials. Likewise, environmental circumstances can trigger symptoms of a genetic disorder. For example, a person predisposed genetically for type 2 diabetes may trigger the disease through poor diet and little exercise.
The developmental psychologist Erik Erikson wrote of an epigenetic principle in his book Identity: Youth and Crisis (1968), encompassing the notion that we develop through an unfolding of our personality in predetermined stages, and that our environment and surrounding culture influence how we progress through these stages. This biological unfolding in relation to our socio-cultural settings is done in stages of psychosocial development, where “progress through each stage is in part determined by our success, or lack of success, in all the previous stages.”
In typical human families, children’s biological parents raise them, so it is very difficult to know whether children act like their parents due to genetic (nature) or environmental (nurture) reasons. Nevertheless, despite our restrictions on setting up human-based experiments, we do see real-world examples of nature-nurture at work in the human sphere—though they only provide partial answers to our many questions. The science of how genes and environments work together to influence behavior is called behavioral genetics. The easiest opportunity we have to observe this is the adoption study. When children are put up for adoption, the parents who give birth to them are no longer the parents who raise them. Children aren’t assigned to random adoptive parents in order to suit the particular interests of a scientist but adoption still tells us some interesting things, or at least confirms some basic expectations. For instance, if the biological child of tall parents were adopted into a family of short people, do you suppose the child’s growth would be affected? What about the biological child of a Spanish-speaking family adopted at birth into an English-speaking family? What language would you expect the child to speak? And what might these outcomes tell you about the difference between height and language in terms of nature-nurture?
Monozygotic and Dizygotic Twins
Another option for observing nature-nurture in humans involves twin studies. To analyze nature-nurture using twins, we compare the similarity of monozygotic and dizygotic pairs. Monozygotic twins occur when a single zygote or fertilized egg splits apart in the first two weeks of development. The result is the creation of two separate but genetically identical offspring. About one-third of twins are monozygotic twins. Monozygotic twins occur in birthing at a rate of about 3 in every 1000 deliveries worldwide (about 0.3% of the world population). Monozygotic twins are genetically nearly identical and they are always the same sex unless there has been a mutation during development. The children of monozygotic twins test genetically as half-siblings (or full siblings, if a pair of monozygotic twins reproduces with another pair of identical twins or with the same person), rather than first cousins.
Sometimes two eggs or ova are released and fertilized by two separate sperm. The result is dizygotic or fraternal twins. About two-thirds of twins are dizygotic. These two individuals share the same amount of genetic material as would any two children from the same mother and father. Older mothers are more likely to have dizygotic twins than are younger mothers and couples who use fertility drugs are also more likely to give birth to dizygotic twins. Consequently, there has been an increase in the number of fraternal twins in recent years (Bortolus et al., 1999). In vitro fertilization (IVF) techniques are more likely to create dizygotic twins. For IVF deliveries, there are nearly 21 pairs of twins for every 1,000.
In the uterus, a majority of monozygotic twins (60–70%) share the same placenta but have separate amniotic sacs. The placenta is a temporary organ that connects the developing fetus via the umbilical cord to the uterine wall to allow nutrient uptake, thermo-regulation, waste elimination, and gas exchange via the mother’s blood supply. The amniotic sac (also called the bag of waters or the membranes), is a thin but tough transparent pair of membranes that hold a developing embryo (and later fetus) until shortly before birth. In 18–30% of monozygotic twins each fetus has a separate placenta and a separate amniotic sac. A small number (1–2%) of monozygotic twins share the same placenta and amniotic sac. Fraternal twins each have their own placenta and own amniotic sac.

Monozygotic (one egg/identical) twins can be categorized into four types depending on the timing of the separation and duplication of cells. Various types of chorionicity and amniosity (how the baby’s sac looks) in monozygotic twins are a result of when the fertilized egg divides. This is known as placentation.
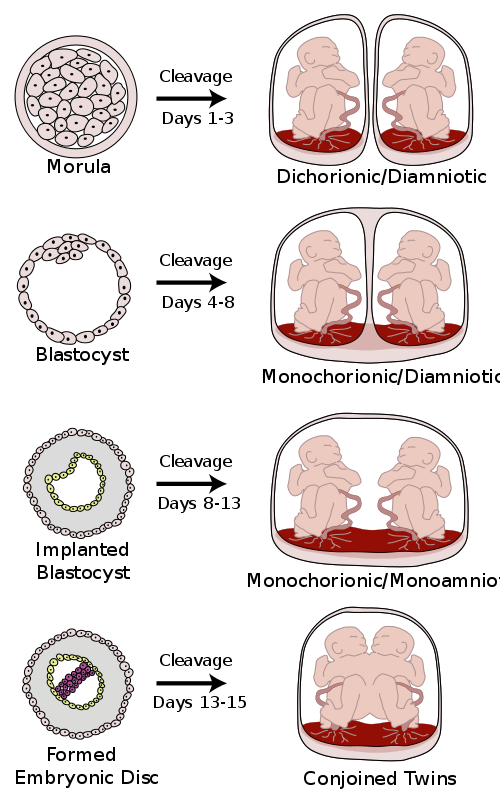
Conjoined twins
Conjoined twins are monozygotic twins whose bodies are joined together during pregnancy. This occurs when the zygote starts to split after day 12 following fertilization and fails to separate completely. This condition occurs in about 1 in 50,000 human pregnancies. Most conjoined twins are now evaluated for surgery to attempt to separate them into separate functional bodies. The degree of difficulty rises if a vital organ or structure is shared between twins, such as the brain, heart, or liver.
Vanishing twins
Researchers suspect that as many as 1 in 8 pregnancies start out as multiples, but only a single fetus is brought to full term because the other fetus has died very early in the pregnancy and has not been detected or recorded. Early obstetric ultrasonography exams sometimes reveal an “extra” fetus, which fails to develop and instead disintegrates and vanishes in the uterus. There are several reasons for the “vanishing” fetus, including it being embodied or absorbed by the other fetus, placenta or the mother. This is known as vanishing twin syndrome. Also, in an unknown proportion of cases, two zygotes may fuse soon after fertilization, resulting in a single chimeric embryo, and, later, fetus.
Twin Studies
Using the features of height and spoken language as examples, let’s take a look at how nature and nurture apply: identical twins, unsurprisingly, are almost perfectly similar for height. The heights of fraternal twins, however, are like any other sibling pairs: more similar to each other than to people from other families, but hardly identical. This contrast between twin types gives us a clue about the role genetics plays in determining height.

Now consider spoken language. If one identical twin speaks Spanish at home, the co-twin with whom she is raised almost certainly does too. But the same would be true for a pair of fraternal twins raised together. In terms of spoken language, fraternal twins are just as similar as identical twins, so it appears that the genetic match of identical twins doesn’t make much difference.
Twin and adoption studies are two instances of a much broader class of methods for observing nature-nurture called quantitative genetics, the scientific discipline in which similarities among individuals are analyzed based on how biologically related they are. We can do these studies with siblings and half-siblings, cousins, and twins who have been separated at birth and raised separately (Bouchard, Lykken, McGue, & Segal, 1990). Such twins are very rare and play a smaller role than is commonly believed in the science of nature-nurture, or with entire extended families (Plomin, DeFries, Knopik, & Neiderhiser, 2012).
It would be satisfying to be able to say that nature-nurture studies have given us conclusive and complete evidence about where traits come from, with some traits clearly resulting from genetics and others almost entirely from environmental factors, such as child-rearing practices and personal will; but that is not the case. Instead, everything has turned out to have some footing in genetics. The more genetically-related people are, the more similar they are—for everything: height, weight, intelligence, personality, mental illness, etc. Sure, it seems like common sense that some traits have a genetic bias. For example, adopted children resemble their biological parents even if they have never met them, and identical twins are more similar to each other than are fraternal twins. And while certain psychological traits, such as personality or mental illness (e.g., schizophrenia), seem reasonably influenced by genetics, it turns out that the same is true for political attitudes, how much television people watch (Plomin, Corley, DeFries, & Fulker, 1990), and whether or not they get divorced (McGue & Lykken, 1992).
What you’ll learn to do: explain the main stages of prenatal development
How did you come to be who you are? From beginning as a one-cell structure to your birth, your prenatal development occurred in an orderly and delicate sequence. There are three stages of prenatal development: germinal, embryonic, and fetal. Keep in mind that this is different than the three trimesters of pregnancy. Let’s take a look at what happens to the developing baby in each of these stages.
Learning outcomes
- Differentiate between development during the germinal, embryonic, and fetal periods
- Examine risks to prenatal development posed by exposure to teratogens
- Explain potential complications of pregnancy and delivery
Prenatal Development
“The body of the unborn baby is more complex than ours. The preborn baby has several extra parts to his body which he needs only so long as he lives inside his mother. He has his own space capsule, the amniotic sac. He has his own lifeline, the umbilical cord, and he has his own root system, the placenta. These all belong to the baby himself, not to his mother. They are all developed from his original cell.”
Periods of Prenatal Development
Let’s take a look at some of the changes that take place during each of the three periods of prenatal development: the germinal period, the embryonic period, and the fetal period.
The Germinal Period (Weeks 1-2)

Conception occurs when a sperm fertilizes an egg and forms a zygote, which begins as a one-cell structure. The mother and father’s DNA is passed on to the child at the moment of conception. The genetic makeup and sex of the baby are set at this point. The germinal period (about 14 days in length) lasts from conception to implantation of the zygote (fertilized egg) in the lining of the uterus.
During the first week after conception, the zygote divides and multiplies, going from a one-cell structure to two cells, then four cells, then eight cells, and so on. The process of cell division is called mitosis. After the fourth division, differentiation of the cells begins to occur as well. Differentiated cells become more specialized, forming different organs and body parts. After 5 days of mitosis, there are 100 cells, and after 9 months there are billions of cells. Mitosis is a fragile process, and fewer than one-half of all zygotes survive beyond the first two weeks (Hall, 2004).
After the zygote divides for about 7–10 days and has 150 cells, it travels down the fallopian tubes and implants itself in the lining of the uterus. It’s estimated that about 60 percent of natural conceptions fail to implant in the uterus. The rate is higher for in vitro conceptions. Once the zygote attaches to the uterus, the next stage begins.
The Embryonic Period (Weeks 3-8)

The embryonic period begins once the zygote is implanted in the uterine wall. It lasts from the third through the eighth week after conception. Upon implantation, this multi-cellular organism is called an embryo. Now blood vessels grow, forming the placenta. The placenta is a structure connected to the uterus that provides nourishment and oxygen from the mother to the developing embryo via the umbilical cord.
During this period, cells continue to differentiate. Basic structures of the embryo start to develop into areas that will become the head, chest, and abdomen. During the embryonic stage, the heart begins to beat and organs form and begin to function. At 22 days after conception, the neural tube forms along the back of the embryo, developing into the spinal cord and brain.
Growth during prenatal development occurs in two major directions: from head to tail (cephalocaudal development) and from the midline outward (proximodistal development). This means that those structures nearest the head develop before those nearest the feet and those structures nearest the torso develop before those away from the center of the body (such as hands and fingers).
The head develops in the fourth week and the precursor to the heart begins to pulse. In the early stages of the embryonic period, gills and a tail are apparent. But by the end of this stage, they disappear and the organism takes on a more human appearance. The embryo is approximately 1 inch in length and weighs about 4 grams at the end of this period. The embryo can move and respond to touch at this time.
About 20 percent of organisms fail during the embryonic period, usually due to gross chromosomal abnormalities. As in the case of the germinal period, often the mother does not yet know that she is pregnant. It is during this stage that the major structures of the body are taking form making the embryonic period the time when the organism is most vulnerable to the greatest amount of damage if exposed to harmful substances. Potential mothers are not often aware of the risks they introduce to the developing child during this time.
The Fetal Period (Weeks 9-40)

When the organism is about nine weeks old, the embryo is called a fetus. At this stage, the fetus is about the size of a kidney bean and begins to take on the recognizable form of a human being as the “tail” begins to disappear.
From 9–12 weeks, the sex organs begin to differentiate. By the 12th week, the fetus has all its body parts including external genitalia. In the following weeks, the fetus will develop hair, nails, teeth and the excretory and digestive systems will continue to develop. At the end of the 12th week, the fetus is about 3 inches long and weighs about 28 grams.
At about 16 weeks, the fetus is approximately 4.5 inches long. Fingers and toes are fully developed, and fingerprints are visible. During the 4-6th months, the eyes become more sensitive to light and hearing develops. The respiratory system continues to develop. Reflexes such as sucking, swallowing, and hiccuping develop during the 5th month. Cycles of sleep and wakefulness are present at that time as well. Throughout the fetal stage, the brain continues to grow and develop, nearly doubling in size from weeks 16 to 28. The majority of the neurons in the brain have developed by 24 weeks although they are still rudimentary and the glial or nurse cells that support neurons continue to grow. At 24 weeks the fetus can feel pain (Royal College of Obstetricians and Gynecologists, 1997).
The first chance of survival outside the womb, known as the age of viability is reached at about 22 to 26 weeks (Moore & Persaud, 1998). By the time the fetus reaches the sixth month of development (24 weeks), it weighs up to 1.4 pounds. The hearing has developed, so the fetus can respond to sounds. The internal organs, such as the lungs, heart, stomach, and intestines, have formed enough that a fetus born prematurely at this point has a chance to survive outside of the mother’s womb.
Between the 7th and 9th months, the fetus is primarily preparing for birth. It is exercising its muscles, its lungs begin to expand and contract. It is developing fat layers under the skin. The fetus gains about 5 pounds and 7 inches during this last trimester of pregnancy which includes a layer of fat gained during the 8th month. This layer of fat serves as insulation and helps the baby regulate body temperature after birth.
Around 36 weeks, the fetus is almost ready for birth. It weighs about 6 pounds and is about 18.5 inches long, and by week 37 all of the fetus’s organ systems are developed enough that it could survive outside the mother’s uterus without many of the risks associated with premature birth. The fetus continues to gain weight and grow in length until approximately 40 weeks. By then, the fetus has very little room to move around and birth becomes imminent.

Environmental Risks
Teratology
Good prenatal care is essential. The developing child is most at risk for some of the most severe problems during the first three months of development. Unfortunately, this is a time at which most mothers are unaware that they are pregnant. It is estimated that 10% of all birth defects are caused by prenatal exposure or teratogen. Teratogens are factors that can contribute to birth defects which include some maternal diseases, drugs, alcohol, and stress. These exposures can also include environmental and occupational exposures. Today, we know many of the factors that can jeopardize the health of the developing child. Teratogen-caused birth defects are potentially preventable.
The study of factors that contribute to birth defects is called teratology. Teratogens are usually discovered after an increased prevalence of a particular birth defect. For example, in the early 1960s, a drug known as thalidomide was used to treat morning sickness. Exposure of the fetus during this early stage of development resulted in cases of phocomelia, a congenital malformation in which the hands and feet are attached to abbreviated arms and legs.
A Look at Some Teratogens
Alcohol

One of the most commonly used teratogens is alcohol. Because half of all pregnancies in the United States are unplanned, it is recommended that women of child-bearing age take great caution against drinking alcohol when not using birth control and when pregnant (Surgeon General’s Advisory on Alcohol Use During Pregnancy, 2005). Alcohol consumption, particularly during the second month of prenatal development, but at any point during pregnancy, may lead to neurocognitive and behavioral difficulties that can last a lifetime.
There is no acceptable safe limit for alcohol use during pregnancy, but binge drinking (5 or more drinks on a single occasion) or having 7 or more drinks during a single week places a child at particularly high risk. In extreme cases, alcohol consumption can lead to fetal death, but more frequently it can result in fetal alcohol spectrum disorders (FASD). This terminology is now used when looking at the effects of exposure and replaces the term fetal alcohol syndrome. It is preferred because it recognizes that symptoms occur on a spectrum and that all individuals do not have the same characteristics. Children with FASD share certain physical features such as flattened noses, small eye openings, small heads, intellectual developmental delays, and behavioral problems. Those with FASD are more at risk for lifelong problems such as criminal behavior, psychiatric problems, and unemployment (CDC, 2006).
The terms alcohol-related neurological disorder (ARND) and alcohol-related birth defects (ARBD) have replaced the term Fetal Alcohol Effects to refer to those with less extreme symptoms of FASD. ARBD includes kidney, bone, and heart problems.
Tobacco
Smoking is also considered a teratogen because nicotine travels through the placenta to the fetus. When the mother smokes, the developing baby experiences a reduction in blood oxygen levels. Tobacco use during pregnancy has been associated with low birth weight, placenta previa, birth defects, preterm delivery, fetal growth restriction, and sudden infant death syndrome. Smoking in the month before getting pregnant and throughout pregnancy increases the chances of these risks. Quitting smoking before getting pregnant is best. However, for women who are already pregnant, quitting as early as possible can still help protect against some health problems for the mother and baby.
Drugs
Prescription, over-the-counter, or recreational drugs can have serious teratogenic effects. In general, if medication is required, the lowest dose possible should be used. Combination drug therapies and first trimester exposures should be avoided. Almost three percent of pregnant women use illicit drugs such as marijuana, cocaine, Ecstasy, and other amphetamines, and heroin. These drugs can cause low birth-weight, withdrawal symptoms, birth defects, or learning or behavioral problems. Babies born with a heroin addiction need heroin just like an adult addict. The child will need to be gradually weaned from the heroin under medical supervision; otherwise, the child could have seizures and die.
Environmental Chemicals
Environmental chemicals can include exposure to a wide array of agents including pollution, organic mercury compounds, herbicides, and industrial solvents. Some environmental pollutants of major concern include lead poisoning, which is connected with low birth weight and slowed neurological development. Children who live in older housing in which lead-based paints have been used have been known to eat peeling paint chips thus being exposed to lead. The chemicals in certain herbicides are also potentially damaging. Radiation is another environmental hazard that a pregnant woman must be aware of. If a mother is exposed to radiation, particularly during the first three months of pregnancy, the child may suffer some congenital deformities. There is also an increased risk of miscarriage and stillbirth. Mercury leads to physical deformities and intellectual disabilities (Dietrich, 1999).
Sexually Transmitted Infections
Sexually transmitted infections (STIs) can complicate pregnancy and may have serious effects on both the mother and the developing baby. Most prenatal care today includes testing for STIs, and early detection is important. STIs, such as chlamydia, gonorrhea, syphilis, trichomoniasis, and bacterial vaginosis can all be treated and cured with antibiotics that are safe to take during pregnancy. STIs that are caused by viruses, like genital herpes, hepatitis B, or HIV cannot be cured. However, in some cases these infections can be treated with antiviral medications or other preventive measures can be taken to reduce the risk of passing the infection to the baby.
Maternal Diseases
Maternal illnesses increase the chance that a baby will be born with a birth defect or have a chronic health problem. Some of the diseases that are known to potentially have an adverse effect on the fetus include diabetes, cytomegalovirus, toxoplasmosis, Rubella, varicella, hypothyroidism, and Strep B. If the mother contracts Rubella during the first three months of pregnancy, damage can occur in the eyes, ears, heart, or brain of the unborn child. On a positive note, Rubella has been nearly eliminated in the industrial world due to the vaccine created in 1969. Diagnosing these diseases early and receiving appropriate medical care can help improve the outcomes. Routine prenatal care now includes screening for gestational diabetes and Strep B.
Maternal Stress
Stress represents the effects of any factor able to threaten the homeostasis of an organism; these either real or perceived threats are referred to as the “stressors” and comprise a long list of potential adverse factors, which can be emotional or physical. Because of a link in blood supply between a mother and fetus, it has been found that stress can leave lasting effects on a developing fetus, even before a child is born. The best-studied outcomes of fetal exposure to maternal prenatal stress are preterm birth and low birth weight. Maternal prenatal stress is also considered responsible for a variety of changes of the child’s brain, and a risk factor for conditions such as behavioral problems, learning disorders, high levels of anxiety, attention deficit hyperactivity disorder, autism, and schizophrenia. Furthermore, maternal prenatal stress has been associated with a higher risk for a variety of immune and metabolic changes in the child such as asthma, allergic disorders, cardiovascular diseases, hypertension, hyperlipidemia, diabetes, and obesity (Konstantinos et al., 2017).
WHAT DO YOU THINK? Should Women Who Use Drugs During Pregnancy Be Arrested and Jailed?
As you now know, women who use drugs or alcohol during pregnancy can cause serious lifelong harm to their child. Some people have advocated mandatory screenings for women who are pregnant and have a history of drug abuse, and if the women continue using, to arrest, prosecute, and incarcerate them (Figdor & Kaeser, 1998). This policy was tried in Charleston, South Carolina, as recently as 20 years ago. The policy was called the Interagency Policy on Management of Substance Abuse During Pregnancy and had disastrous results.
The Interagency Policy applied to patients attending the obstetrics clinic at MUSC, which primarily serves patients who are indigent or on Medicaid. It did not apply to private obstetrical patients. The policy required patient education about the harmful effects of substance abuse during pregnancy. . . . [A] statement also warned patients that protection of unborn and newborn children from the harms of illegal drug abuse could involve the Charleston police, the Solicitor of the Ninth Judicial Court, and the Protective Services Division of the Department of Social Services (DSS). (Jos, Marshall, & Perlmutter, 1995, pp. 120–121)
This policy seemed to deter women from seeking prenatal care, deterred them from seeking other social services, and was applied solely to low-income women, resulting in lawsuits. The program was canceled after 5 years, during which 42 women were arrested. A federal agency later determined that the program involved human experimentation without the approval and oversight of an institutional review board (IRB). What were the flaws in the program and how would you correct them? What are the ethical implications of charging pregnant women with child abuse?
Factors influencing prenatal risks
There are several considerations in determining the type and amount of damage that might result from exposure to a particular teratogen (Berger, 2004). These include:
- The timing of the exposure: Structures in the body are vulnerable to the most severe damage when they are forming. If a substance is introduced during a particular structure’s critical period (time of development), the damage to that structure may be greater. For example, the ears and arms reach their critical periods at about 6 weeks after conception. If a mother exposes the embryo to certain substances during this period, the arms and ears may be malformed.
- The amount of exposure: Some substances are not harmful unless the amounts reach a certain level. The critical level depends in part on the size and metabolism of the mother.
- Genetics: Genetic make-up also plays a role in the impact a particular teratogen might have on the child. This is suggested by fraternal twin studies who are exposed to the same prenatal environment, yet do not experience the same teratogenic effects. The genetic make-up of the mother can also have an effect; some mothers may be more resistant to teratogenic effects than others.
- Being male or female: Males are more likely to experience damage due to teratogens than are females. It is believed that the Y chromosome, which contains fewer genes than the X, may have an impact.

Complications of Pregnancy and Delivery

There are a number of common side effects of pregnancy. Not everyone experiences all of these nor do women experience them to the same degree. And although they are considered “minor” these problems are potentially very uncomfortable. These side effects include nausea (particularly during the first 3-4 months of pregnancy as a result of higher levels of estrogen in the system), heartburn, gas, hemorrhoids, backache, leg cramps, insomnia, constipation, shortness of breath or varicose veins (as a result of carrying a heavy load on the abdomen). What is the cure? Delivery!
Major Complications
The following are some serious complications of pregnancy that can pose health risks to mother and child and that often require special care.
- Gestational diabetes is when a woman without diabetes develops high blood sugar levels during pregnancy.
- Hyperemesis gravidarum is the presence of severe and persistent vomiting, causing dehydration and weight loss. It is more severe than the more common morning sickness.
- Preeclampsia is gestational hypertension. Severe preeclampsia involves blood pressure over 160/110 with additional signs. Eclampsia is seizures in a pre-eclamptic patient.
- Deep vein thrombosis is the formation of a blood clot in a deep vein, most commonly in the legs.
- A pregnant woman is more susceptible to infections. This increased risk is caused by an increased immune tolerance in pregnancy to prevent an immune reaction against the fetus.
- Peripartum cardiomyopathy is a decrease in heart function which occurs in the last month of pregnancy, or up to six months post-pregnancy.
Maternal Mortality
Maternal mortality is unacceptably high. About 295,000 women died during and following pregnancy and childbirth in 2017. The vast majority of these deaths (94%) occurred in low-resource settings, and most could have been prevented. The high number of maternal deaths in some areas of the world reflects inequalities in access to quality health services and highlights the gap between rich and poor. The MMR in low-income countries in 2017 is 462 per 100,000 live births versus 11 per 100,000 live births in high-income countries. The high number of maternal deaths in some areas of the world reflects inequities in access to health services and highlights the gap between rich and poor.
Women in less developed countries have, on average, many more pregnancies than women in developed countries, and their lifetime risk of death due to pregnancy is higher. A woman’s lifetime risk of maternal death is the probability that a 15-year-old woman will eventually die from a maternal cause. In high-income countries, this is 1 in 5400, versus 1 in 45 in low-income countries. Every day in 2017, approximately 810 women died from preventable causes related to pregnancy and childbirth.
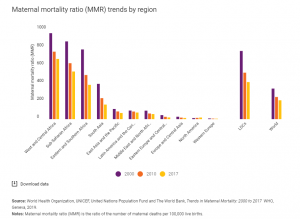
Figure 8. The number of women and girls who died each year from complications of pregnancy and childbirth declined from 451,000 in 2000 to 295,000 in 2017. These improvements are particularly remarkable in light of rapid population growth in many of the countries where maternal deaths are highest. Still, over 800 women are dying each day from complications in pregnancy and childbirth. And for every woman who dies, approximately 20 others suffer serious injuries, infections or disabilities. Source: UNICEF, https://data.unicef.org/topic/maternal-health/maternal-mortality/.Even though maternal mortality in the United States is relatively rare today because of advances in medical care, it is still an issue that needs to be addressed. Sadly, about 700 women die each year in the United States as a result of pregnancy or delivery complications. The Centers for Disease Control and Prevention define a pregnancy-related death as the death of a woman while pregnant or within 1 year of the end of a pregnancy–regardless of the outcome, duration, or site of the pregnancy–from any cause related to or aggravated by the pregnancy or its management, but not from accidental or incidental causes.
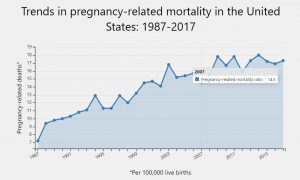
Since the Pregnancy Mortality Surveillance System was implemented, the number of reported pregnancy-related deaths in the United States steadily increased from 7.2 deaths per 100,000 live births in 1987 to 17.3 deaths per 100,000 live births in 2017. The graph above shows trends in pregnancy-related mortality ratios between 1987 and 2017 (the latest available year of data).
The reasons for the overall increase in pregnancy-related mortality are unclear. What do you think are some reasons for this surprising increase in the United States? What can be done to change this statistic?
Watch It: Maternal Mortality in the United States
In the United States, black women are disproportionately more likely to die from complications related to pregnancy or childbirth than any other race; they are three or four times more likely than white women to die due to pregnancy-related death and are more likely to receive worse maternal care. Black women from higher income groups and with advanced education levels also have heightened risks—even tennis superstar Serena Williams had near-deadly complications during the birth of her daughter, Olympia. Why is this the case in our modern world? Watch this video to learn more.
Considerable racial/ethnic disparities in pregnancy-related mortality exist.2,3 During 2014–2017, the pregnancy-related mortality ratios were:
- 41.7 deaths per 100,000 live births for non-Hispanic Black women.
- 28.3 deaths per 100,000 live births for non-Hispanic American Indian or Alaska Native women.
- 13.8 deaths per 100,000 live births for non-Hispanic Asian or Pacific Islander women.
- 13.4 deaths per 100,000 live births for non-Hispanic White women.
- 11.6 deaths per 100,000 live births for Hispanic or Latina women.
Variability in the risk of death by race/ethnicity may be due to several factors including access to care, quality of care, prevalence of chronic diseases, structural racism, and implicit biases.
Why do women die in Pregnancy and Childbirth Worldwide?
Women die as a result of complications during and following pregnancy and childbirth. Most of these complications develop during pregnancy and most are preventable or treatable. Other complications may exist before pregnancy but are worsened during pregnancy, especially if not managed as part of the woman’s care. The major complications that account for nearly 75% of all maternal deaths are:
- severe bleeding (mostly bleeding after childbirth)
- infections (usually after childbirth)
- high blood pressure during pregnancy (pre-eclampsia and eclampsia)
- complications from delivery
The remainder are caused by or associated with infections such as malaria or related to chronic conditions like cardiac diseases or diabetes.
Why do women die in Pregnancy and Childbirth in the United States?
Compare the data that you learned about above with percentages of pregnancy-related deaths in the United States during 2014–2017.
- Other cardiovascular conditions, 15.5%.
- Infection or sepsis, 12.7%.
- Cardiomyopathy, 11.5%.
- Hemorrhage, 10.7%.
- Thrombotic pulmonary or other embolism, 9.6%.
- Cerebrovascular accidents, 8.2%.
- Hypertensive disorders of pregnancy, 6.6%.
- Amniotic fluid embolism, 5.5%.
- Anesthesia complications, 0.4%.
- Other noncardiovascular medical conditions, 12.5%.
The cause of death is unknown for 6.7% of all 2014–2017 pregnancy-related deaths.
While the contributions of hemorrhage, hypertensive disorders of pregnancy (i.e., preeclampsia, eclampsia), and anesthesia complications to pregnancy-related deaths have declined, the contributions of cardiovascular, cerebrovascular accidents, and other medical conditions have increased.12 Studies show that an increasing number of pregnant women in the United States have chronic health conditions such as hypertension,13,14 diabetes,14-17 and chronic heart disease.12,18 These conditions may put a woman at higher risk of complications during pregnancy or in the year postpartum.
Miscarriage
Pregnancy loss is experienced in an estimated 20-40 percent of undiagnosed pregnancies and in another 10 percent of diagnosed pregnancies. Usually, the body aborts due to chromosomal abnormalities and this typically happens before the 12th week of pregnancy. Cramping and bleeding result and normal periods should return after several months. Or it may be necessary to have a surgical procedure called D&E (dilation and evacuation). Some women are more likely to have repeated miscarriages due to chromosomal, amniotic, or hormonal problems; but miscarriage can also be a result of defective sperm (Carroll et al., 2003).
In the U.S., a pregnancy loss before the 20th week of pregnancy is referred to as a miscarriage, while the term stillbirth refers to the loss of a baby after 20 weeks’ gestation. A woman must still go through labor or a c-section to deliver her baby. Stillbirth affects about 1 in 160 births, and each year about 24,000 babies are stillborn in the United States. That is about the same number of babies that die during the first year of life and it is more than 10 times as many deaths as the number that occur from Sudden Infant Death Syndrome (SIDS).
As you can see, what may seem like a simple process is in fact a beautiful and delicate journey. Each pregnancy and birth story is unique and comes with surprises and sometimes challenges. As medical technology has rapidly improved, women are empowered with more information and more choices when it comes to their pregnancy and birth. However, just because interventions are available does not mean that this is the path for all mothers. As we learned in the case with Serena Williams, even in the U.S. sometimes medical care can go awry. Each mother needs to be an active advocate for herself and her baby during her pregnancy and delivery.
Where do you think we are headed with how medical advances are used in pregnancy and delivery? More women are able to get pregnant with reproductive assistance, oftentimes past the age that they would naturally conceive. At the beginning of the module, the topic of “designer babies” was introduced. After completing this module, do you think that we are headed towards this in the near future? What are the ethical ramifications?
Additional Supplemental Resources
Websites
- The Human Genome Project (Links to an external site.)
- The Human Genome Project (HGP) was an inward voyage of discovery led by an international team of researchers looking to sequence and map all of the genes — together known as the genome — of members of our species, Homo sapiens. Beginning in October 1990 and completed in April 2003, the HGP gave us the ability, for the first time, to read nature’s complete genetic blueprint for building a human being.
- Institute for Behavioral Genetics (Links to an external site.)
- Founded in 1967, IBG is one of the top research facilities in the world for genetic research on behavior. Data collection and analysis are ongoing for several internationally renowned studies including the Colorado Adoption Project, the Colorado Twin Registry, the National Youth Survey Family Study, the Colorado Learning Disabilities Research Center, and the National Longitudinal Study of Adolescent Health.
Videos
- Fertilization
- This video, created by Nucleus Medical Media, shows human fertilization, also known as conception. Shown at a cellular level magnification, sperm struggle through many obstacles in the female reproductive tract to reach the egg. Then genetic material from the egg and a single sperm combines to form a new human being.
- Conception to birth- Visualized
- Image-maker Alexander Tsiaras shares a powerful medical visualization, showing human development from conception to birth and beyond.
- What are DNA and Genes?
- The Genetic Science Learning Center sponsored by the University of Utah delivers educational materials on genetics, bioscience, and health topics. All humans have the same genes arranged in the same order. And more than 99.9% of our DNA sequence is the same. But the few differences between us (all 1.4 million of them!) are enough to make each one of us unique.
- What is Inheritance?
- The Genetic Science Learning Center sponsored by the University of Utah delivers educational materials on genetics, bioscience, and health topics. This video explains the importance of genetic variation.
- Down Syndrome- Ability Awareness
- What comes to mind when you think of a person who has Down Syndrome? Do you have a preconceived idea of what their abilities might be? Chris Burke talks about his experience and his work at the National Down Syndrome Society.
- Prenatal Testing Options
- The University of Michigan provides this video that explains the difference between prenatal screening and diagnostic testing. Pregnant women are faced with the decision of whether to undergo prenatal screening and testing – and, if so – which of the many options to choose from.
- Prenatal Development: What We Learn Inside the Womb
- Let’s watch what we experience and learn inside the womb from the fetus’ perspective.
- TED talk: How CRISPR lets us Edit our DNA
- Geneticist Jennifer Doudna co-invented a groundbreaking new technology for editing genes, called CRISPR-Cas9. The tool allows scientists to make precise edits to DNA strands, which could lead to treatments for genetic diseases … but could also be used to create so-called “designer babies.” Doudna reviews how CRISPR-Cas9 works — and asks the scientific community to pause and discuss the ethics of this new tool.




