3 Integumentary System
Learning Objectives
- Apply the rules of medical language to build, analyze, spell, pronounce, abbreviate, and define terms as they relate to the integumentary system
- Identify meanings of key word components of the integumentary system
- Use terms related to the integumentary system
Integumentary System Word Parts
Click on prefixes, combining forms, and suffixes to reveal a list of word parts to memorize for the Integumentary System.
Introduction to the Integumentary System
The integumentary system refers to the skin and its accessory structures. In the adult human body, the skin makes up about 16 percent of body weight and covers an area of 16-21 ft2.
In fact, the skin and accessory structures are the largest organ system in the human body. The skin protects your inner organs and it is in need of daily care and protection to maintain its health.
Watch the video The science of skin – Emma Bryce (5 minutes)
Anatomy (Structures) of the Integumentary System
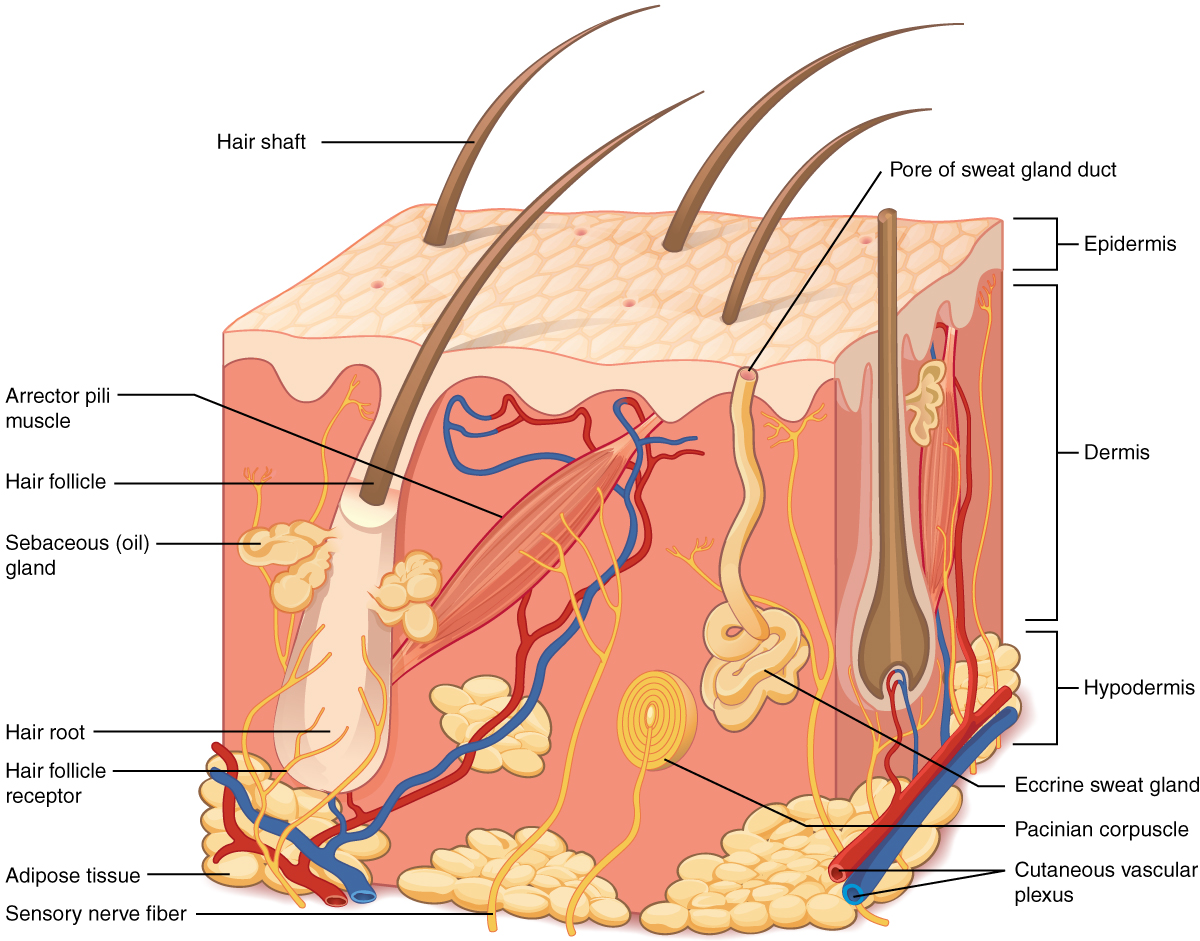
The skin and its accessory structures make up the integumentary system, which provides the body with overall protection. The skin is made of multiple layers of cells and tissues, which are held to underlying structures by connective tissue. The deeper layer of skin is well vascularized. It also has numerous sensory, and autonomic and sympathetic nerve fibers ensuring communication to and from the brain.
The skin is composed of two main layers:
- The epidermis
- The dermis
- Beneath the dermis lies the hypodermis
Concept Check
- On the diagram above find the two layers of the skin; epidermis and dermis.
- The literal breakdown for hypodermis is below the dermis. On the diagram above, where can you locate it?
- Can you find a hair follicle, hair root, and hair shaft?
Epidermis
The epidermis is composed of keratinized, stratified squamous epithelium. It is made of four or five layers of epithelial cells, depending on its location in the body. It is avascular.
The cells in all of the layers except the stratum basale are called keratinocytes. Keratin is an intracellular fibrous protein that gives hair, nails, and skin their hardness and water-resistant properties. The keratinocytes in the stratum corneum are dead and regularly slough away, being replaced by cells from the deeper layers.
Dermis

Papillary Layer
The papillary layer is made of loose, areolar connective tissue, which means the collagen and elastin fibers of this layer form a loose mesh. This superficial layer of the dermis projects into the stratum basale of the epidermis to form finger-like dermal papillae (see Figure 3.2). Within the papillary layer are fibroblasts, a small number adipocytes, and an abundance of small blood vessels. In addition, the papillary layer contains phagocytes, that help fight bacteria or other infections that have breached the skin. This layer also contains lymphatic capillaries, nerve fibers, and Meissner corpuscles.
Reticular Layer
Underlying the papillary layer is the much thicker reticular layer, composed of dense, irregular connective tissue. This layer is well vascularized and has a rich sensory and sympathetic nerve supply. The reticular layer appears reticulated due to a tight meshwork of fibers. Elastin fibers provide some elasticity to the skin, enabling movement. Collagen fibers provide structure and tensile strength, with strands of collagen extending into both the papillary layer and the hypodermis. In addition, collagen binds water to keep the skin hydrated. Collagen injections and Retin-A creams help restore skin turgor by either introducing collagen externally or stimulating blood flow and repair of the dermis, respectively.
Hypodermis
The hypodermis serves to connect the skin to the underlying fascia of the bones and muscles. It is not strictly a part of the skin, although the border between the hypodermis and dermis can be difficult to distinguish. The hypodermis consists of well-vascularized, loose, areolar connective tissue and adipose tissue, which functions as a mode of fat storage and provides insulation and cushioning for the integument.
Practice labeling the layers of the skin.
Physiology (Function) of the Integumentary System
The skin and accessory structures perform a variety of essential functions, such as protecting the body from invasion by microorganisms, chemicals, and other environmental factors; preventing dehydration; acting as a sensory organ; modulating body temperature and electrolyte balance; and synthesizing vitamin D. The underlying hypodermis has important roles in storing fats, forming a “cushion” over underlying structures, and providing insulation from cold temperatures.
Protection
The skin protects the body from wind, water, and UV sunlight. It acts as a protective barrier against water loss and it also is the first line of defense against abrasive activity such as grit, microbes, or harmful chemicals. Sweat excreted from sweat glands deters microbes from over-colonizing the skin surface.
Sensory Function
The skin acts as a sense organ because the epidermis, dermis, and the hypodermis contain specialized sensory nerve structures that detect touch, surface temperature, and pain. These receptors are more concentrated on the tips of the fingers, which are most sensitive to touch, especially the Meissner corpuscle, which responds to light touch, and the Pacinian corpuscle , which responds to vibration. Merkel cells, seen scattered in the stratum basale, are also touch receptors. In addition to these specialized receptors, there are sensory nerves connected to each hair follicle, pain and temperature receptors scattered throughout the skin, and motor nerves innervate the arrector pili muscles and glands. This rich innervation helps us sense our environment and react accordingly,
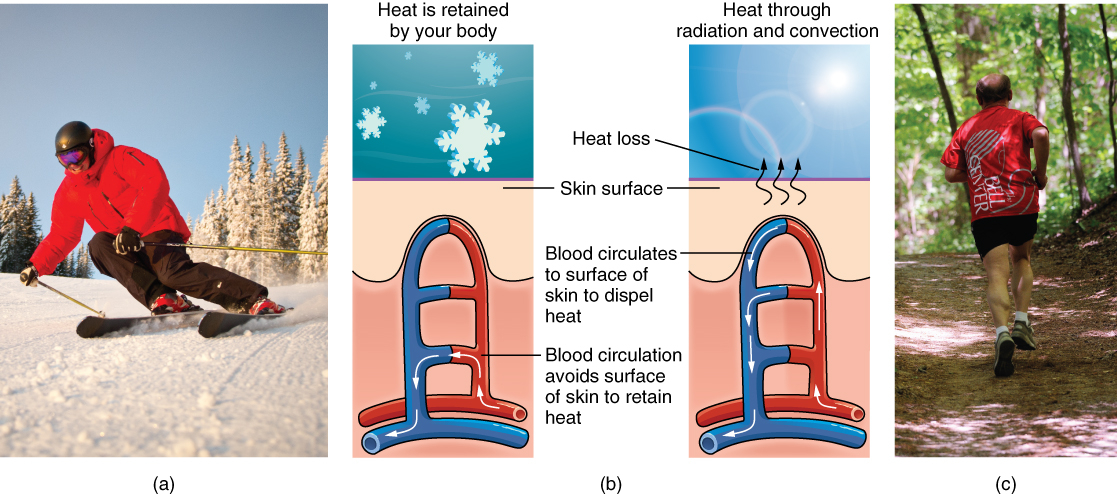
Thermoregulation
The integumentary system helps regulate body temperature through its tight association with the sympathetic nervous system. The sympathetic nervous system is continuously monitoring body temperature and initiating appropriate motor responses.
- When the body becomes warm sweat glands, accessory structures to the skin, secrete water, salt, and other substances to cool the body.
- Even when the body does not appear to be noticeably sweating, approximately 500 mL of sweat are secreted a day.
- If the body becomes excessively warm due to high temperatures, vigorous activity, or a combination of the two, sweat glands will be stimulated by the sympathetic nervous system to produce large amounts of sweat.
- When the sweat evaporates from the skin surface, the body is cooled as body heat is dissipated.
- In addition to sweating, arterioles in the dermis dilate so that excess heat carried by the blood can dissipate through the skin and into the surrounding environment.
- This accounts for the skin redness that many people experience when exercising.
- When body temperatures drop, the arterioles constrict to minimize heat loss, particularly in the ends of the digits and tip of the nose.
- This reduced circulation can result in the skin taking on a whitish hue.
- Although the temperature of the skin drops as a result, passive heat loss is prevented, and internal organs and structures remain warm.
- If the temperature of the skin drops too much (such as environmental temperatures below freezing), the conservation of body core heat can result frostbite.
Vitamin D Synthesis
The epidermal layer of human skin synthesizes Vitamin D when exposed to UV radiation. In the presence of sunlight, a form of Vitamin D3 called cholecalciferol is synthesized from a derivative of the steroid cholesterol in the skin. The liver converts cholecalciferol to calcidiol, which is then converted to calcitriol (the active chemical form of the vitamin) in the kidneys.
- Vitamin D is essential for normal absorption of calcium and phosphorous, which are required for healthy bones.
- The absence of sun exposure can lead to a lack of vitamin D in the body, in children this can cause rickets. Vitamin D deficiency in elderly individuals may lead to osteomalacia.
- In present-day society, Vitamin D is added as a supplement to many foods, including milk and orange juice, compensating for the need for sun exposure. In addition to its essential role in bone health, Vitamin D is essential for general immunity against bacterial, viral, and fungal infections.
Watch the video: The Integumentary System, Part 2 – Skin Deeper: Crash Course Anatomy & Physiology #7 (10 minutes)
Accessory Structures
Accessory structures of the skin include hair, nails, sweat glands, and sebaceous glands. These structures embryologically originate from the epidermis and can extend down through the dermis into the hypodermis.
Hair
Hair is a keratinous filament growing out of the epidermis. It is primarily made of dead, keratinized cells. Strands of hair originate in an epidermal penetration of the dermis called the hair follicle. The hair shaft is the part of the hair not anchored to the follicle, and much of this is exposed at the skin’s surface. The rest of the hair, which is anchored in the follicle, lies below the surface of the skin and is referred to as the hair root. The hair root ends deep in the dermis at the hair bulb, and includes a layer of mitotically active basal cells called the hair matrix. The hair bulb surrounds the hair papilla, which is made of connective tissue and contains blood capillaries and nerve endings from the dermis (see Figure 3.4).
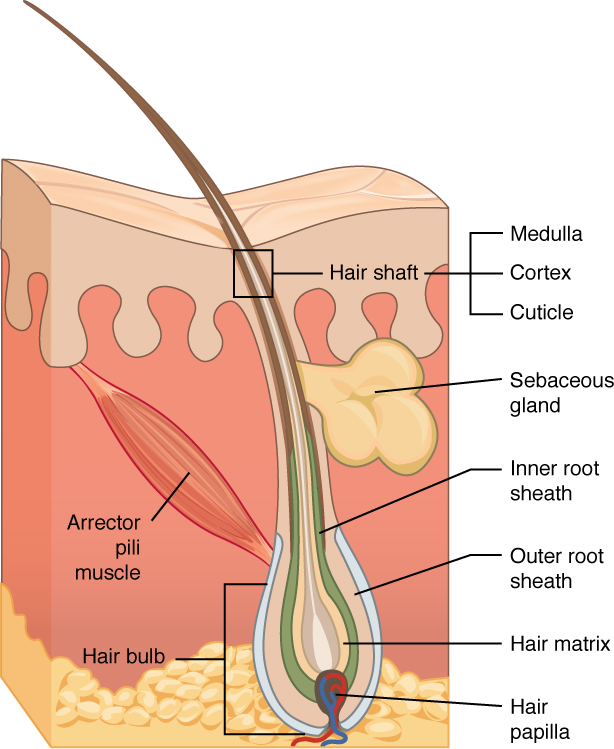
Hair Function
Hair serves a variety of functions, including protection, sensory input, thermoregulation, and communication. For example:
- Hair on the head protects the skull from the sun.
- Hair in the nose and ears, and around the eyes (eyelashes) defends the body by trapping and excluding dust particles that may contain allergens and microbes.
- Hair of the eyebrows prevents sweat and other particles from dripping into and bothering the eyes.
Hair also has a sensory function due to sensory innervation by a hair root plexus surrounding the base of each hair follicle. Hair is extremely sensitive to air movement or other disturbances in the environment, much more so than the skin surface. This feature is also useful for the detection of the presence of insects or other potentially damaging substances on the skin surface.
Each hair root is connected to a smooth muscle called the arrector pili that contracts in response to nerve signals from the sympathetic nervous system, making the external hair shaft “stand up.” The primary purpose for this is to trap a layer of air to add insulation. This is visible in humans as goose bumps and even more obvious in animals, such as when a frightened cat raises its fur. Of course, this is much more obvious in organisms with a heavier coat than most humans, such as dogs and cats.
Hair Growth, Loss and Color
Hair grows and is eventually shed and replaced by new hair. Hair typically grows at the rate of 0.3 mm per day. On average, 50 hairs are lost and replaced per day. Hair loss occurs if there is more hair shed than what is replaced and can happen due to hormonal or dietary changes. Hair loss can also result from the aging process, or the influence of hormones. Similar to the skin, hair gets its color from the pigment melanin, produced by melanocytes in the hair papilla. Different hair color results from differences in the type of melanin. As a person ages, the melanin production decreases, and hair tends to lose its color and becomes gray and/or white.
Nails
The nail bed is a specialized structure of the epidermis that is found at the tips of our fingers and toes. The nail body is formed on the nail bed, and protects the tips of our fingers and toes as they are the farthest extremities and the parts of the body that experience the maximum mechanical stress (see Figure 3.5). The nail body forms a back-support for picking up small objects with the fingers. The nail body is composed of densely packed dead keratinocytes.
The epidermis in this part of the body has evolved a specialized structure upon which nails can form. The nail body forms at the nail root, which has a matrix of proliferating cells from the stratum basale that enables the nail to grow continuously. The lateral nail fold overlaps the nail on the sides, helping to anchor the nail body. The nail fold that meets the proximal end of the nail body forms the nail cuticle, also called the eponychium.
The nail bed is rich in blood vessels, making it appear pink, except at the base, where a thick layer of epithelium over the nail matrix forms a crescent-shaped region called the lunula (the “little moon”). The area beneath the free edge of the nail, furthest from the cuticle, is called the hyponychium. It consists of a thickened layer of stratum corneum.
Sweat Glands
Sudoriferous Glands
When the body becomes warm, sudoriferous glands produce sweat to cool the body. Sweat glands develop from epidermal projections into the dermis and are classified as merocrine glands; that is, the secretions are excreted by exocytosis through a duct without affecting the cells of the gland. There are two types of sweat glands, each secreting slightly different products.
An eccrine sweat gland is type of gland that produces a hypotonic sweat for thermoregulation as described previously. These glands are found all over the skin’s surface, but are especially abundant on the palms of the hand, the soles of the feet, and the forehead (Figure 3.6). They are coiled glands lying deep in the dermis, with the duct rising up to a pore on the skin surface, where the sweat is released. This type of sweat, released by exocytosis, is hypotonic and composed mostly of water, with some salt, antibodies, traces of metabolic waste, and dermicidin, an antimicrobial peptide. Eccrine glands are a primary component of thermoregulation in humans and thus help to maintain homeostasis .
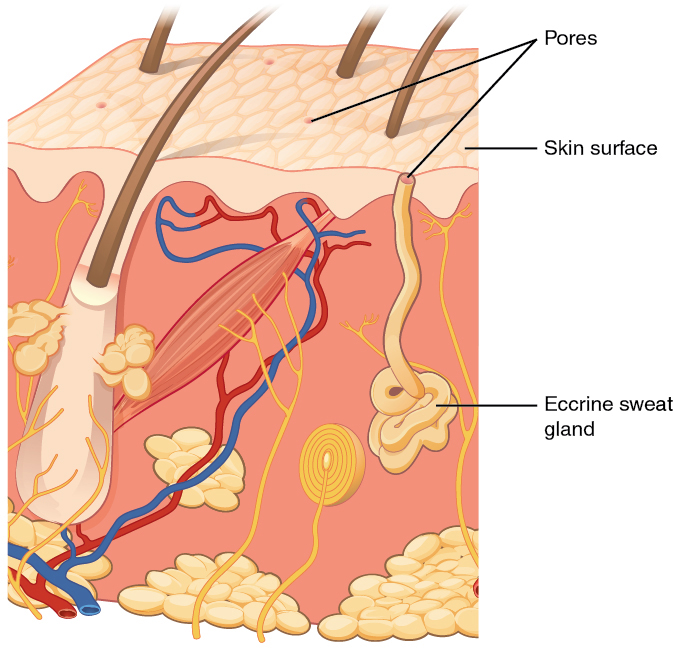
An apocrine sweat gland is usually associated with hair follicles in densely hairy areas, such as armpits and genital regions. Apocrine sweat glands are larger than eccrine sweat glands and lie deeper in the dermis, sometimes even reaching the hypodermis, with the duct normally emptying into the hair follicle. In addition to water and salts, apocrine sweat includes organic compounds that make the sweat thicker and subject to bacterial decomposition and subsequent smell. The release of this sweat is under both nervous and hormonal control, and plays a role in the poorly understood human pheromone response. Most commercial antiperspirants use an aluminum-based compound as their primary active ingredient to stop sweat. When the antiperspirant enters the sweat gland duct, the aluminum-based compounds precipitate due to a change in pH and form a physical block in the duct, which prevents sweat from coming out of the pore.
Sebaceous Glands
A sebaceous gland is a type of oil gland that is found all over the body and helps to lubricate and waterproof the skin and hair. Most sebaceous glands are associated with hair follicles. They generate and excrete sebum, a mixture of lipids, onto the skin surface, thereby naturally lubricating the dry and dead layer of keratinized cells of the stratum corneum, keeping it pliable. The fatty acids of sebum also have antibacterial properties, and prevent water loss from the skin in low-humidity environments. The secretion of sebum is stimulated by hormones, many of which do not become active until puberty. Thus, sebaceous glands are relatively inactive during childhood.
Changes Due to Aging
All systems in the body accumulate subtle and some not-so-subtle changes as a person ages. Among these changes are reductions in cell division, metabolic activity, blood circulation, hormonal levels, and muscle strength (see Figure 3.7). In the skin, these changes are reflected in decreased mitosis in the stratum basale, leading to a thinner epidermis. The dermis, which is responsible for the elasticity and resilience of the skin, exhibits a reduced ability to regenerate, which leads to slower wound healing. The hypodermis, with its fat stores, loses structure due to the reduction and redistribution of fat, which in turn contributes to the thinning and sagging of skin.

The accessory structures also have lowered activity, generating thinner hair and nails, and reduced amounts of sebum and sweat. A reduced sweating ability can cause some elderly to be intolerant to extreme heat. Other cells in the skin, such as melanocytes and dendritic cells, also become less active, leading to a paler skin tone and lowered immunity. Wrinkling of the skin occurs due to breakdown of its structure, which results from decreased collagen and elastin production in the dermis, weakening of muscles lying under the skin, and the inability of the skin to retain adequate moisture.
Test Yourself
Use these practice activities to review the concepts in this chapter. If you prefer, there is a printable version of these activities.
Identify meanings of key word components of the integumentary system.
Click on prefixes, combining forms, and suffixes to reveal a list of word parts to memorize for the Integumentary System.
Apply the rules of medical language to pronounce, break into word parts, and define the following integumentary system words.
Practice pronouncing and defining these commonly abbreviated integumentary system terms.
Practice filling in the blanks with the correct word parts.
Practice labeling the layers of the skin.
References
Centers for Disease Control and Prevention. (2018, October 25). Psoriasis. Centers for Disease Control and Prevention: Fungal Diseases. https://www.cdc.gov/psoriasis/
Centers for Disease Control and Prevention. (2018a, August 6). Ringworm. Centers for Disease Control and Prevention: Fungal Diseases. https://www.cdc.gov/fungal/diseases/ringworm/definition.html
Mayo Clinic Staff. (2017, September 6). Mohs surgery. Mayo Clinic. https://www.mayoclinic.org/tests-procedures/mohs-surgery/about/pac-20385222#:~:text=Mohs%20surgery%20is%20a%20precise,known%20as%20Mohs%20micrographic%20surgery.
Chapter Attributions
This chapter was adapted by Jerry Casteel from “Integumentary System” by Stacey Grimm; Coleen Allee; Elaine Strachota; Laurie Zielinski; Traci Gotz; Micheal Randolph; and Heidi Belitz. Licensed under a CC BY 4.0 license.
Media Attributions
The science of skin – Emma Bryce by TED-Ed is licensed under the Standard YouTube license.
The Integumentary System, Part 2 – Skin Deeper: Crash Course Anatomy & Physiology #7 by CrashCourse is licensed under the Standard YouTube license.
has numerous blood vessels
unconsciously regulates
flight or fight response
outer layer of skin, made of closely packed epithelial cells
The layer that is made of dense, irregular connective tissue that houses blood vessels, hair follicles, sweat glands, and other structures
Literally means below the dermis. The layer of the skin below the dermis that is composed mainly of loose connective and fatty tissues
without blood vessels
an epidermal cell which produces keratin
fat cells
Cells that engulf and absorb bacteria and cell particles
Tactile corpsucle that responds to light and touch, touch receptors.
net like
fibrous tissue
used for the storage of fat
tactile corpuscle that responds to light and touch, touch receptor
lamellated corpuscle that responds to vibration
fight or flight responses
Conservation of the body core heat results in the skin actually freezing
A painful condition in children where bones are misshapen due to a lack of calcium, causing bow leggedness
Softening of the bone(s)
Specialized cells that produce melanin which is a dark pigment responsible for colouration of skin and hair.
Molecules are transported out of cells. A form of active transport.
biological process that results in stable equilibrium
Pertaining to dendrites

