Nervous System (SC)
Topic: Nervous System
Text Reference: Chapter 12. Nervous System
Objectives: Students should be able to…
Identify meanings of keyword components of the nervous system
Prefixes
a- (absence of, without, no, not)
an- (absence of, without, no, not)
pan- (all, total)
post- (after)
para- (beside, beyond, around, abnormal)
pre- (before)
sub- (below, under)
dys- (painful, abnormal, difficult, labored)
intra- (within)
hemi- (half)
hyper- (above, excessive)
inter- (between)
poly- (many, much)
Combining Forms
agles/o (sensitivity to pain)
cephal/o (head)
cerebell/o (cerebellum)
cerebr/o (cerebrum)
dur/o (dura mater, hard)
encephal/o (brain)
esthesi/o (sensation, sensitivity)
gangli/o (ganglion)
ganglion/o (ganglion)
gli/o (glia, gluey substance)
mening/o (meninges)
meningi/o (meninges)
ment/o (mind)
mon/o (one, single)
myel/o (spinal cord)
neur/o (nerve)
phas/o (speech)
poli/o (gray matter)
pont/o (pons- structure in the brain)
psych/o (mind)
quadr/i (four)
radic/o (nerve root)
radicul/o (nerve root)
rhiz/o (nerve root)
thalam/o (thalamus)
thec/o (sheath)
vag/o (vagus nerve)
Suffixes
-al (pertaining to)
-algia (pain)
-algesia (sensitivity to pain)
-cele (hernia, protrusion)
-cyte (cell)
-ectomy (excision, surgical removal, cutting out)
-genic (producing, originating, causing)
-gram (the record, radiographic image)
-graph (instrument used to record)
-graphy (process of recording, radiographic imaging)
-ia (condition of, diseased state or abnormal state)
-ic (pertaining to)
-iatrist (specialist, physician)
-iatry (specialty, treatment)
-ictal (seizure, attack)
-itis (inflammation)
-lepsy (seizure)
-logist (specialist, physician)
-logy (study of)
-lysis (loosening, dissolution, separating)
-malacia (softening)
-oid (resembling)
-oma (tumor)
-osis (abnormal condition)
-paresis (slight paralysis)
-pathy (disease)
-phasia (speech)
-plasty (surgical repair)
-plegia (paralysis)
-praxia (to perform, action)
-sclerosis (hardening)
-rrhaphy (suturing, repairing)
-tomy (incision, cut into)
Apply the rules of medical language to pronounce, break into word parts, and define the following terms.
Label each word part by using the following abbreviations:
P = Prefix
WR = Word Root
CV = Combining Vowel
S = Suffix
CF = Combining Form
Example: osteoarthropathy (ä-stē-ō-är-THROP-ă-thē) – disease of bone and joint
WR CV WR CV S
oste / o / arthr / o /pathy
CF CF
Practice pronouncing and defining these commonly abbreviated nervous system terms.
AD (Alzheimer’s disease)
ADHD (attention deficit hyperactivity disorder)
ALS (amyotrophic lateral sclerosis)
CNS (central nervous system)
CP (cerebral palsy)
CSF (cerebrospinal fluid)
CTE (chronic traumatic encephalopathy)
CVA (cerebrovascular accident)
EEG (electroencephalogram)
EP studies (evoked potential studies)
LP (lumbar puncture)
MRI (magnetic resonance imaging)
MS (multiple sclerosis)
OCD (obsessive-compulsive disorder)
PD (Parkinson’s disease)
PET (positron emission tomography)
PNS (peripheral nervous system)
PTSD (post-traumatic stress disorder)
SAH (subarachnoid hemorrhage)
TIA (transient ischemic attack)
Sort the terms from the word lists above into the following categories.
- Disease and Disorder (terms describing any deviation from normal structure and function)
- Diagnostic (terms related to process of identifying a disease, condition, or injury from its signs and symptoms)
- Therapeutic (terms related to treatment or curing of diseases)
- Anatomic (terms related to body structure)
Use terms related to the nervous system.
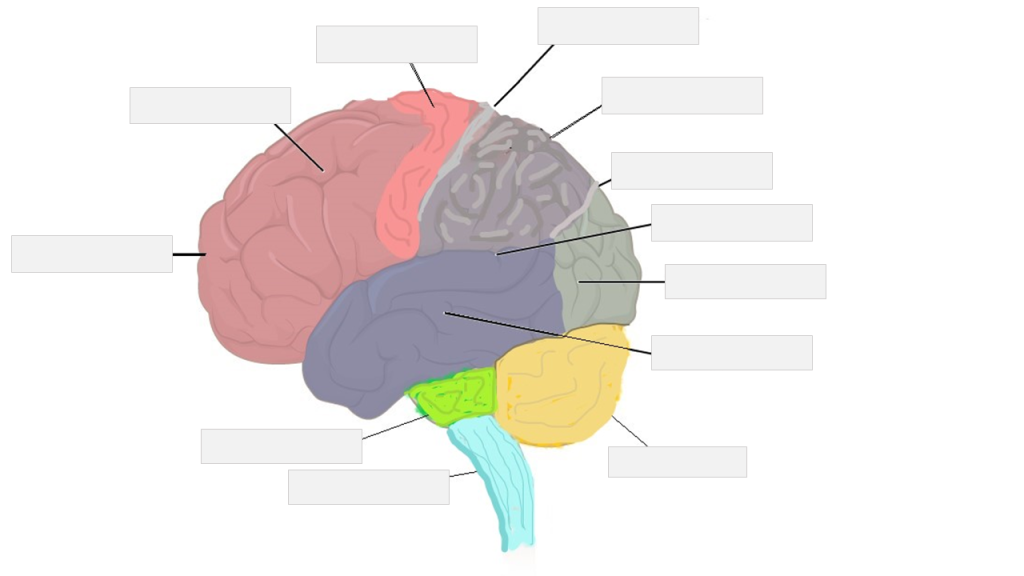
Label the following nervous system anatomy.
brainstem | central sulcus, longitudinal fissure | cerebellum | cerebrum | frontal lobe | lateral sulcus | occipital lobe | parietal lobe | parieto-occipital sulcus | pons | precentral gyrus | temporal lobe
Place the following medical terms in context to complete the scenario below.
cognition | depression | downgoing | fatigue | festination | postural | q.i.d. | rigidity
NEUROLOGICAL SYSTEM – HISTORY AND PHYSICAL EXAMINATION
PATIENT NAME: Susan LOGAN
AGE: 62
SEX: Female
DOB: March 24
DATE OF ASSESSMENT: December 10
ADMITTING PHYSICIAN: Martin Lewis, MD, Neurology
DIAGNOSIS: Parkinson disease
HISTORY: This pleasant and co-operative 62-year-old woman has advanced parkinsonism which presents for more than 10 years. It is affecting her daily living to a great degree. She has minor difficulty with ADLs noted in difficulty dressing and meal preparation. She has had frequent falls occasionally related to freezing or to ________ but also occurring without any apparent cause. She has marked hesitancy on changing direction and unsteadiness after exertion and develops ________. She has a minor problem with sialorrhea, eating, and swallowing. She can maintain basic personal hygiene without any difficulty. However, showering or bathing requires assistance. She has had some symptoms of anxiety and ________ along with her Parkinson disease.
PHYSICAL EXAMINATION: On neurologic exam, she did have mild-to-moderate impairment in ________ and short-time memory, although she is alert and oriented x3. She has pronounced tremor, worse in the left arm than the right. She has marked ________ in the upper left extremity; mild in the right. She has marked reduction of movement with long delays in initiating movement and frequent freezing. She has a moderately-flexed posture and cannot straighten to command. She has ________ instability. Her speech is mildly dysarthric. She has paucity of spontaneous facial expression. She has an unsteady and erratic gait characterized by shuffling strides with festination in propulsion. She can arise from a chair with difficulty only after multiple attempts. Deep tendon reflexes (DTRs) are symmetrical, and toes are ________. Cranial nerves are intact and unremarkable.
TREATMENT AND PLAN: She has been on Sinemet 25/100 t.i.d. for the last 7 years or so. She will be going on vacation soon, and I do not wish to start a second antiparkinsonian medication while she away from medical supervision. However, I have asked her to increase her Sinemet dose to ________. We will see how she does with Sinemet and plan to add bromocriptine 1 mg per day when she returns.
FOLLOW UP: The patient has been scheduled for follow up in 3 weeks, upon her return from vacation. Her treatment regimen will be adjusted at that time.
________________________
Martin Lewis, MD, Neurology
Place the following medical terms in context to complete the scenario below.
blurred | cognition | dementia | downgoing | hypertension | MRI | neurological | stroke | symptomatic
NEUROLOGICAL SYSTEM – CONSULTATION REPORT
PATIENT NAME: Robert BROWN
AGE: 74
SEX: Male
DOB: July 5
DATE OF CONSULTATION: April 15
CONSULTING PHYSICIAN: Martin Lewis, MD, Neurology
REASON FOR CONSULTATION: Assessment of cognitive changes and testing.
HISTORY: The patient presented a few days ago with a marked change in ________ identified by his family members and care staff. The reports describe two episodes of the patient presenting a somewhat confused state, instability with a “holding of the temples” and a report of blurring vision. The patient was also observed holding on to walls and furniture to walk around. This seems to have been two transient episodes and has not recurred since. Prior to that, he had maintained excellent cognitive abilities with full lingual ability, no signs of aphasia, ________, or loss of consciousness. The cognitive decline noticed was not of gradual onset but rather an acute change within hours to a day. The time span is unclear as the patient lives alone and there was a time lapse between a family visit and the arrival of a personal care assistant.
The patient is a good historian to questioning and does admit to some recent occasional headaches and ________ vision. These are new to him as he reports never having “had a headache” in his “whole life”. He reports that the blurring is not constant but only seems to occur when he turns his head to right or left suddenly. There is a “tilting sensation” like he will fall but this clears when he brings his head back to center. He has no history of epilepsy or seizure disorders. No history of TM or ear trauma.
PHYSICAL EXAMINATION: HEENT: Head is normocephalic. EYES: PERRLA. EARS: Auditory exam reveals intact TMs bilaterally. No erythema. The nose and throat exam is unremarkable. NECK: JVD appears normal. VITAL SIGNS: Blood pressure is 132/86 with no previous history of ________. Pulse is 83 and resp. 22 but the patient does admit to feeling anxious during the assessment. Temperature 37C.
NEURO: Orientation and language are normal. Extremity strength testing show some minimal weakness in the right upper. Reflexes are normal. Toes are ________ bilaterally. Has difficulty with heel-and toe-walk and is unable to tandem walk. The gait is alternately normal and minimally spastic.
IMPRESSION: What appears to be a transient or acute cognitive change with altered awareness, headache and cephalo-positional blurring of vision. There is some ________ change, although minimal and not clinically diagnostic, as evidenced by the slight changes in gait during testing but it does not remain consistently. This is puzzling.
PLAN: It is still not clear to me what these spells are. Some of the neurological possibilities to be considered are TIA, ________, brain and spinal cord tumors, inflammation, infection, vascular irregularities, and some neurodegenerative disorders. I have ordered a stat cerebral ________, electroencephalogram (EEG) and blood levels for CBC, chem panel. However, I feel we should also rule out the more common possibilities of pseudo-seizure, vertigo, and inner ear anomalies and am in the process of making these appropriate bookings.
I have booked a follow up with this patient in 10 days to review the results. He and his family have been advised to contact me immediately if he has another “spell” or to present to the ER where we can complete testing when the patient is ________.
Thank you for this most interesting referral. I will be in touch after I have reviewed the patient.
_________________________
Martin Lewis, MD, Neurology
Place the following medical terms in context to complete the scenario below.
balance | calcifications | coordination | electroencephalogram | hemorrhagic | mass | pathology | somnolence | symptomatic | vertigo | wasting | white matter
NEUROLOGICAL SYSTEM – FOLLOW UP REPORT
PATIENT NAME: Randy NORTON
AGE: 74
SEX: Male
DOB: October 14
DATE OF ASSESSMENT: January 18
ASSESSING PHYSICIAN: Martin Lewis, MD, Neurology
REASON FOR ASSESSMENT: Follow up assessment of cognitive changes and testing.
HISTORY: This 74-year-old patient was seen in consultation 10 days ago for assessment of cognitive changes. He underwent prescribed testing in the forms of cerebral MRI, ________ (EEG) and blood was drawn for CBC and chem panel. The patient was seen by our local ENT for inner ear and ________ testing. Test results showed normal hearing. No evidence of an inner ear ________ that might have contributed to the ________ or lack of balance and ________ reported as part of the presenting symptoms.
TEST RESULTS: Cerebral MRI reveals a few T2 hyperintensities in the ________ in the left temporal lobe. The right hemisphere shows some diffuse ________ and some occipital wasting. There are multiple, small dark ________ areas and a few areas indicative of ischemia.
EEG: This showed some depressive effect indicative of an encephalopathy. The patient did not sleep during the exam but did show some signs of ________. CBC and chem panels were normal.
IMPRESSIONS: This patient present with testing result that may be warning for Alzheimer wasting and also, some localized hemorrhagic events that have since stopped. This type of “leakage” is often not ________, and I do not feel that they are connected to his presenting complaints. I see no signs of tumor or ________ formation nor infectious process.
On repeat verbal assessment, the patient reports he has not experienced any more of the spells. We will follow him closely in regards to the ________ with a repeat MRI and perhaps a CT also in 3 months for results comparison to see whether the wasting has advanced or receded.
Thank you for asking me in on this most interesting case.
_________________________
Martin Lewis, MD, Neurology
Test your knowledge by answering the questions below.
The outer gray matter covering the forebrain, marked by wrinkles and folds known as gyri and sulci…
- Multipolar
- Cerebral cortex
- Dendrite
The large opening in the occipital bone of the skull through which the spinal cord emerges and the vertebral arteries enter the cranium…
- Foramen magnum
- Corpus callosum
- Dura mater
The disruption of blood flow to the brain because blood cannot flow through blood vessels as a result of a blockage or narrowing of the vessel…
- Embolus
- Ischemic stroke
- Initial segment
The major region of the diencephalon that is responsible for coordinating autonomic and endocrine control of homeostasis…
- Neuron
- Hypothalamus
- Myelin
The single process of the neuron that carries an electrical signal (action potential) away from the cell body toward a target cell…
- Cauda equina
- Axon
- Cerebrum
Chapter Attributions
This chapter was adapted by Karen Hobbs from “Nervous System” in Medical Terminology Student Companion by Stacey Grimm; Colleen Allee; Heidi Belitz; Traci Gotz; Micheal Randolph; Elaine Strachota; and Laurie Zielinski. Licensed under a CC BY 4.0 license.

