4 Respiratory System
Learning Objectives
- Apply the rules of medical language to build, analyze, spell, pronounce, abbreviate, and define terms as they relate to the respiratory system
- Identify meanings of key word components of the respiratory system
- Use terms related to the respiratory system
Respiratory System Word Parts
Click on prefixes, combining forms, and suffixes to reveal a list of word parts to memorize for the Respiratory System.
Introduction to the Respiratory System
How long you can hold your breath as you continue reading… How long can you do it? Chances are you are feeling uncomfortable already. A typical human cannot survive without breathing for more than three minutes, and even if you wanted to hold your breath longer, your autonomic nervous system would take control. Although oxygen is critical for cells, it is the accumulation of carbon dioxide that primarily drives your need to breathe.
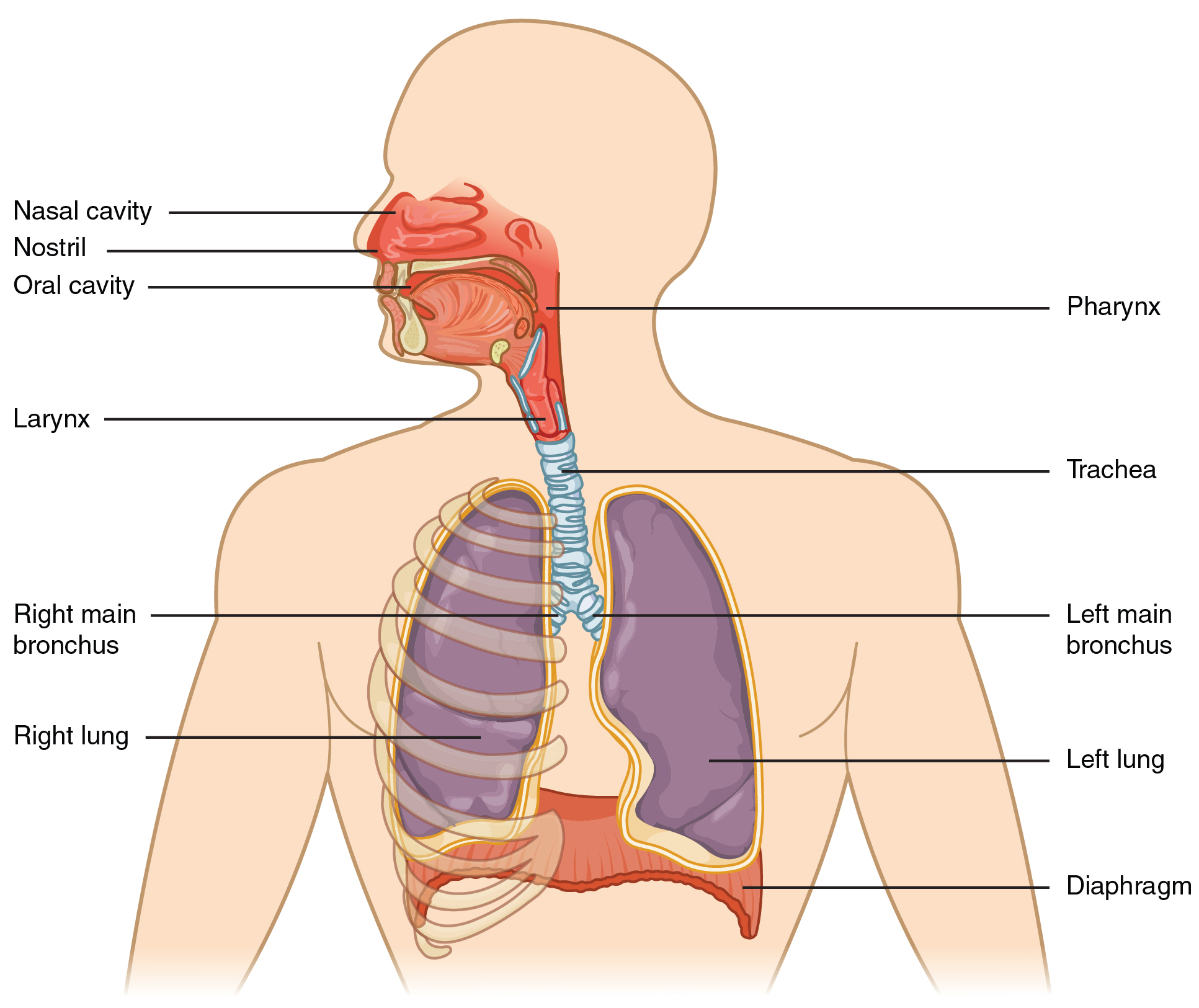
The major structures of the respiratory system function primarily to provide oxygen to body tissues for cellular respiration, remove the waste product carbon dioxide, and help to maintain acid-base balance. Portions of the respiratory system are also used for non-vital functions, such as sensing odors, speech production, and for straining, such as coughing.
Respiratory System Medical Terms
Anatomy (Structures) of the Respiratory System
The Nose and its Adjacent Structures
The major entrance and exit for the respiratory system is through the nose. When discussing the nose, it is helpful to divide it into two major sections:
The nares open into the nasal cavity, which is separated into left and right sections by the nasal septum (Figure 4.2). The nasal septum is formed anteriorly by a portion of the septal cartilage and posteriorly by the perpendicular plate of the ethmoid bone and the thin vomer bones.
Each lateral wall of the nasal cavity has three bony projections the inferior conchae are separate bones and the superior and middle conchae are portions of the ethmoid bone. Conchae increase the surface area of the nasal cavity, disrupt the flow of air as it enters the nose, causing air to bounce along the epithelium, where it is cleaned and warmed. The conchae and meatuses trap water during exhalation preventing dehydration.
The floor of the nasal cavity is composed of the hard palate and the soft palate. Air exits the nasal cavities via the internal nares and moves into the pharynx.
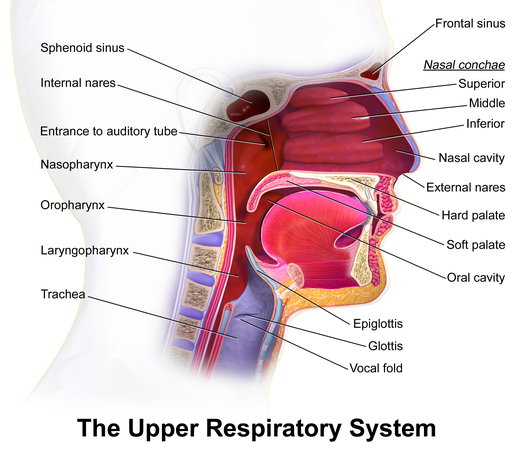
Paranasal sinuses serve to warm and humidify incoming air. They are lined with a mucosa which produces mucus. Paranasal sinuses are named for their associated bone:
- frontal sinus
- maxillary sinus
- sphenoidal sinus
- ethmoidal sinus
The nares and anterior portion of the nasal cavities are lined with mucous membranes, containing sebaceous glands and hair follicles that serve to prevent the passage of large debris, such as dirt, through the nasal cavity. An olfactory epithelium used to detect odors is found deeper in the nasal cavity.
The cilia of the respiratory epithelium help to remove mucus and debris with a constant beating motion, sweeping materials towards the throat to be swallowed. This moist epithelium functions to warm and humidify incoming air.
Pharynx
The pharynx is divided into three major regions: the nasopharynx, the oropharynx, and the laryngopharynx (see Figure 4.3).
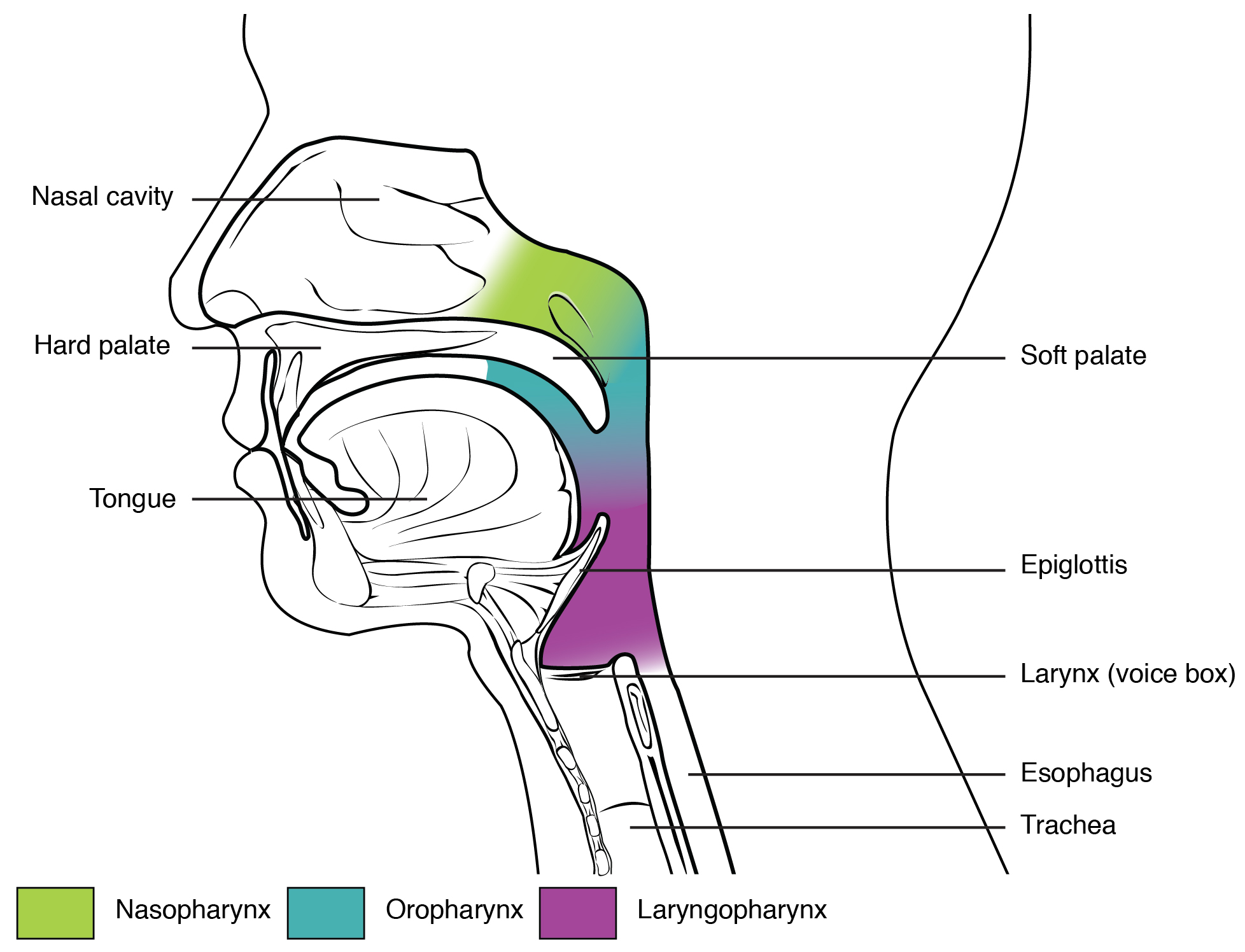
At the top of the nasopharynx are the pharyngeal tonsils. The function of the pharyngeal tonsil is not well understood, but it contains a rich supply of lymphocytes and is covered with ciliated epithelium that traps and destroys invading pathogens that enter during inhalation. The pharyngeal tonsils are large in children, but tend to regress with age and may even disappear. The uvula and soft palate move like a pendulum during swallowing, swinging upward to close off the nasopharynx to prevent ingested materials from entering the nasal cavity. Auditory (Eustachian) tubes that connect to each middle ear cavity open into the nasopharynx. This connection is why colds often lead to ear infections.
The oropharynx is bordered superiorly by the nasopharynx and anteriorly by the oral cavity. The oropharynx contains two distinct sets of tonsils:
- The palatine tonsils.
- A palatine tonsil is one of a pair of structures located laterally in the oropharynx
- The lingual tonsils.
- The lingual tonsil is located at the base of the tongue.
Similar to the pharyngeal tonsil, the palatine and lingual tonsils are composed of lymphoid tissue, and trap and destroy pathogens entering the body through the oral or nasal cavities.
The laryngopharynx is inferior to the oropharynx and posterior to the larynx. It continues the route for ingested material and air until its inferior end, where the digestive and respiratory systems diverge. The stratified squamous epithelium of the oropharynx is continuous with the laryngopharynx. Anteriorly, the laryngopharynx opens into the larynx, whereas posteriorly, it enters the esophagus.
Larynx
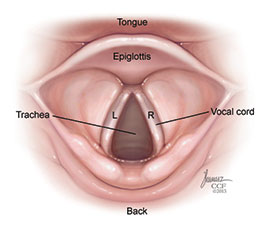
The structure of the larynx is formed by several pieces of cartilage (see Figure 4.4). Three large cartilage pieces form the major structure of the larynx.
- Thyroid cartilage (anterior)
- Epiglottis (superior)
- Cricoid cartilage (inferior)
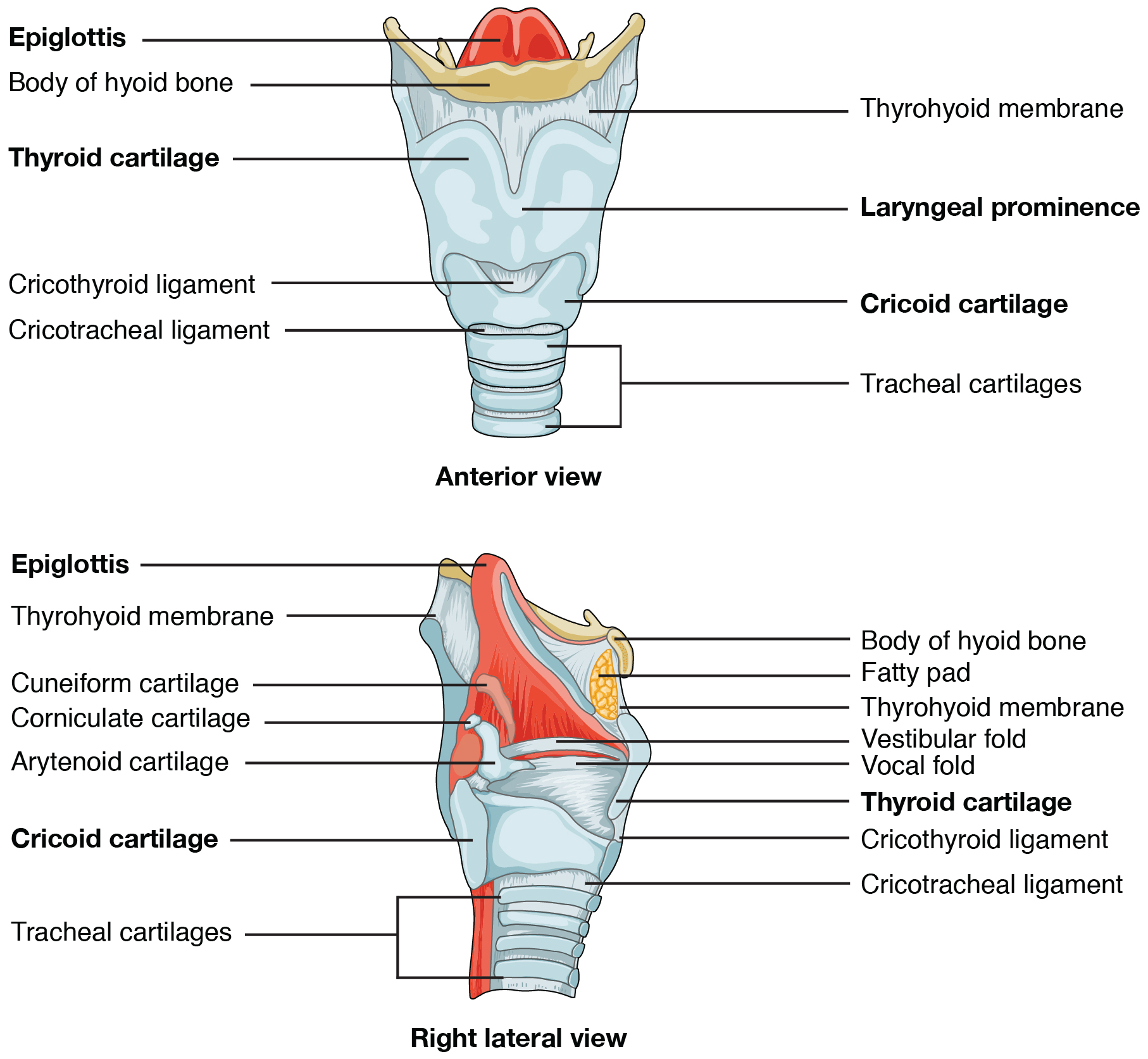
When the epiglottis is in the “closed” position, the unattached end of the epiglottis rests on the glottis.
The act of swallowing causes the pharynx and larynx to lift upward, allowing the pharynx to expand and the epiglottis of the larynx to swing downward, closing the opening to the trachea. These movements produce a larger area for food to pass through, while preventing food and beverages from entering the trachea.
Similar to the nasal cavity and nasopharynx, this specialized epithelium produces mucus to trap debris and pathogens as they enter the trachea. The cilia beat the mucus upward towards the laryngopharynx, where it can be swallowed down the esophagus.
Trachea
The trachea is formed by 16 to 20 stacked, C-shaped pieces of hyaline cartilage that are connected by dense connective tissue (see Figure 4.6). The trachealis muscle and elastic connective tissue together form the fibroelastic membrane. The fibroelastic membrane allows the trachea to stretch and expand slightly during inhalation and exhalation, whereas the rings of cartilage provide structural support and prevent the trachea from collapsing. The trachealis muscle can be contracted to force air through the trachea during exhalation. The trachea is lined with pseudostratified ciliated columnar epithelium, which is continuous with the larynx. The esophagus borders the trachea posteriorly.
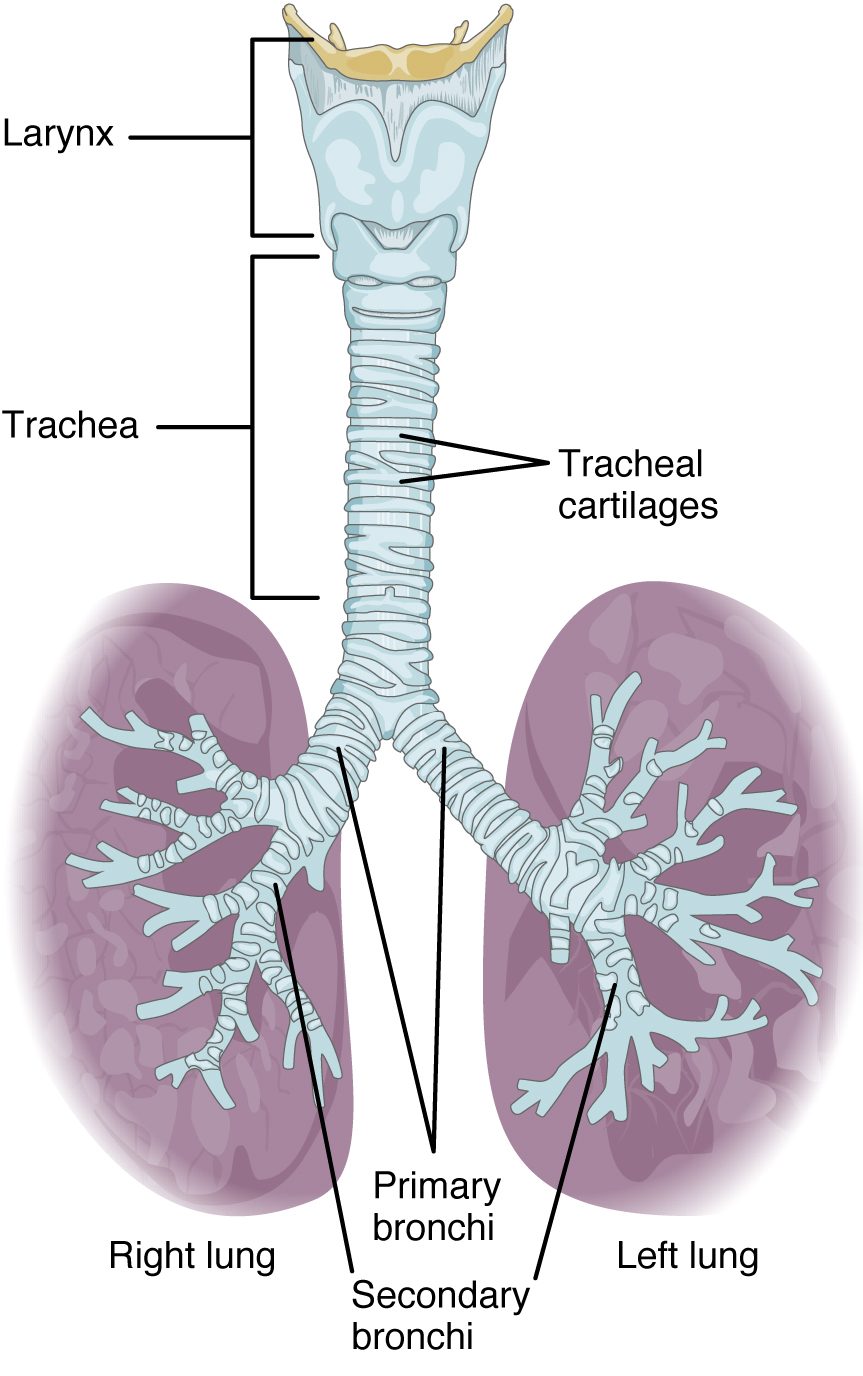
Bronchial Tree
The trachea branches into the right and left primary bronchi at the carina. The carina is a raised structure that contains specialized nervous tissue that induces violent coughing if a foreign body, such as food, is present. Rings of cartilage, similar to those of the trachea, support the structure of the bronchi and prevent their collapse. The primary bronchi enter the lungs at the hilum. The bronchi continue to branch into bronchial a tree. A bronchial tree (or respiratory tree) is the collective term used for these multiple-branched bronchi. The main function of the bronchi, like other conducting zone structures, is to provide a passageway for air to move into and out of each lung. The mucous membrane traps debris and pathogens.
The bronchiole branches from the tertiary bronchi. Bronchioles, which are about 1 mm in diameter, further branch until they become the tiny terminal bronchioles, which lead to the structures of gas exchange. There are more than 1000 terminal bronchioles in each lung. The muscular walls of the bronchioles do not contain cartilage like those of the bronchi. This muscular wall can change the size of the tubing to increase or decrease airflow through the tube.
Respiratory Zone
In contrast to the conducting zone, the respiratory zone includes structures that are directly involved in gas exchange. The respiratory zone begins where the terminal bronchioles join a respiratory bronchiole, the smallest type of bronchiole (see Figure 4.7), which then leads to an alveolar duct, opening into a cluster of alveoli.
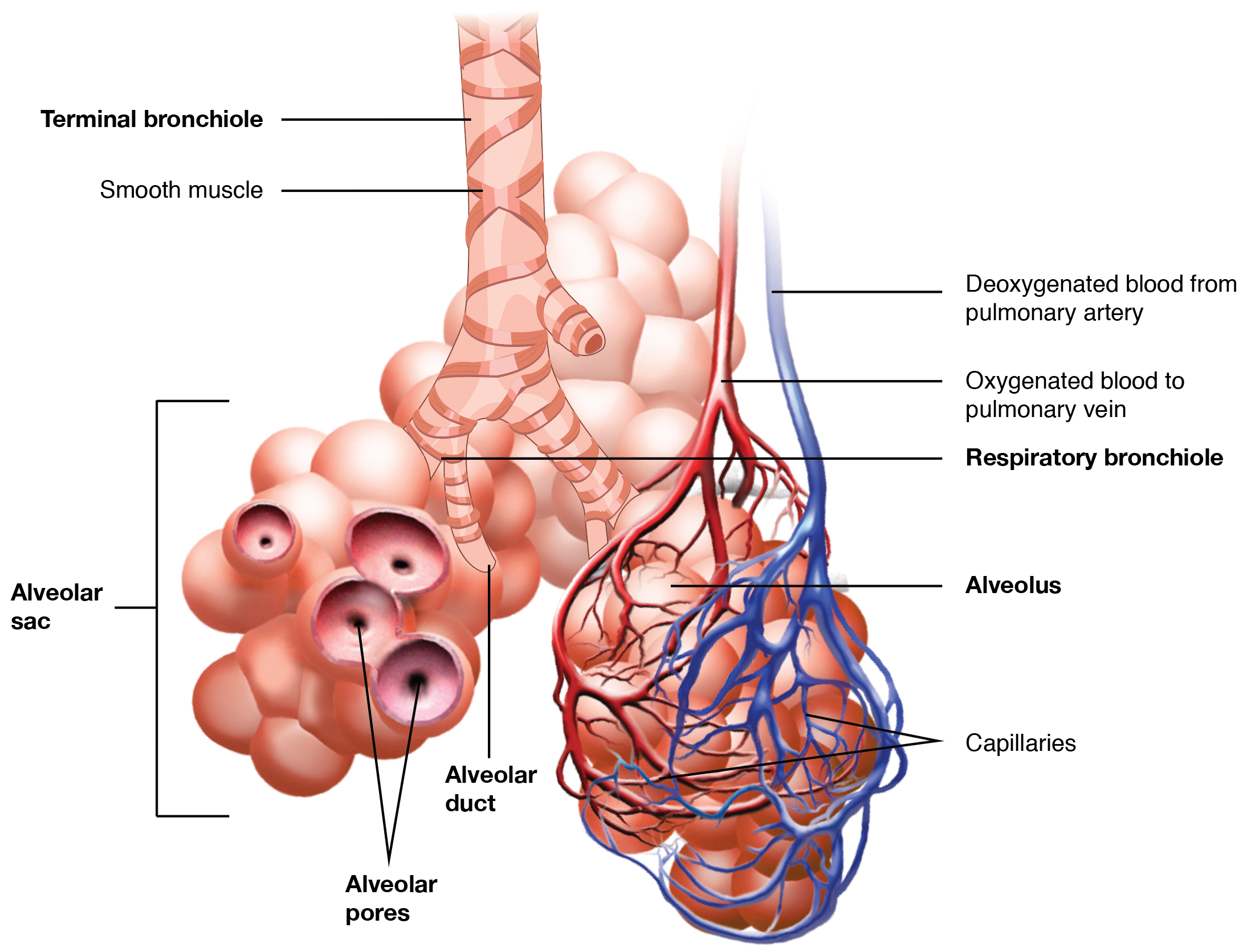
Alveoli
An alveolar duct opens into a cluster of alveoli. An alveolus is one of the many small, grape-like sacs that are attached to the alveolar ducts. An alveolar sac is a cluster of many individual alveoli that are responsible for gas exchange. An alveolus is approximately 0.2 millimeters in diameter with elastic walls that allow the alveolus to stretch during air intake, which greatly increases the surface area available for gas exchange. Alveoli are connected to their neighbors by alveolar pores, which help maintain equal air pressure throughout the alveoli and lung (see Fig. 4.7).
Concept Check
- What are the components of the bronchial tree?
- What is the purpose of cilia?
- Where does gas exchange take place?
Gross Anatomy of the Lungs
The lungs are pyramid-shaped, paired organs that are connected to the trachea by the right and left bronchi; on the inferior surface, the lungs are bordered by the diaphragm. The lungs are enclosed by the pleurae, which are attached to the mediastinum. The right lung is shorter and wider than the left lung, and the left lung occupies a smaller volume than the right. The cardiac notch allows space for the heart (see Figure 4.8). The apex of the lung is the superior region, whereas the base is the opposite region near the diaphragm. The costal surface of the lung borders the ribs. The mediastinal surface faces the mid line.

Each lung is composed of smaller units called lobes. Fissures separate these lobes from each other. The right lung consists of three lobes: the superior, middle, and inferior lobes. The left lung consists of two lobes: the superior and inferior lobes. A pulmonary lobule is a subdivision formed as the bronchi branch into bronchioles. Each lobule receives its own large bronchiole that has multiple branches. An interlobular septum is a wall, composed of connective tissue, which separates lobules from one another.
Can you correctly label the respiratory system structures?
Physiology (Function) of the Respiratory System
Blood Supply
The major function of the lungs is to perform gas exchange, which requires blood from the pulmonary circulation.
- This blood supply contains deoxygenated blood and travels to the lungs where erythrocytes pick up oxygen to be transported to tissues throughout the body.
- The pulmonary artery carries deoxygenated, arterial blood to the alveoli.
- The pulmonary artery branches multiple times as it follows the bronchi, and each branch becomes progressively smaller in diameter.
- One arteriole and an accompanying venule supply and drain one pulmonary lobule. As they near the alveoli, the pulmonary arteries become the pulmonary capillary network.
- The pulmonary capillary network consists of tiny vessels with very thin walls that lack smooth muscle fibers.
- The capillaries branch and follow the bronchioles and structure of the alveoli. It is at this point that the capillary wall meets the alveolar wall, creating the respiratory membrane.
- Once the blood is oxygenated, it drains from the alveoli by way of multiple pulmonary veins, which exit the lungs through the hilum.
Nervous Innervation
The blood supply of the lungs plays an important role in gas exchange and serves as a transport system for gases throughout the body. Innervation by the both the parasympathetic and sympathetic nervous systems provides an important level of control through dilation and constriction of the airway.
- The parasympathetic system causes bronchoconstriction.
- The sympathetic nervous system stimulates bronchodilation.
Reflexes such as coughing, and the ability of the lungs to regulate oxygen and carbon dioxide levels, also result from autonomic nervous system control.
Pleura of the Lungs
Each lung is enclosed within a cavity that is surrounded by the pleura. The pleura (plural = pleurae) is a serous membrane that surrounds the lung. The right and left pleurae, which enclose the right and left lungs, respectively, are separated by the mediastinum.
The pleurae consist of two layers:
- The visceral pleura is the layer that is superficial to the lungs, and extends into and lines the lung fissures (see Figure 4.9).
- The parietal pleura is the outer layer that connects to the thoracic wall, the mediastinum, and the diaphragm.
The visceral and parietal pleurae connect to each other at the hilum. The pleural cavity is the space between the visceral and parietal layers.
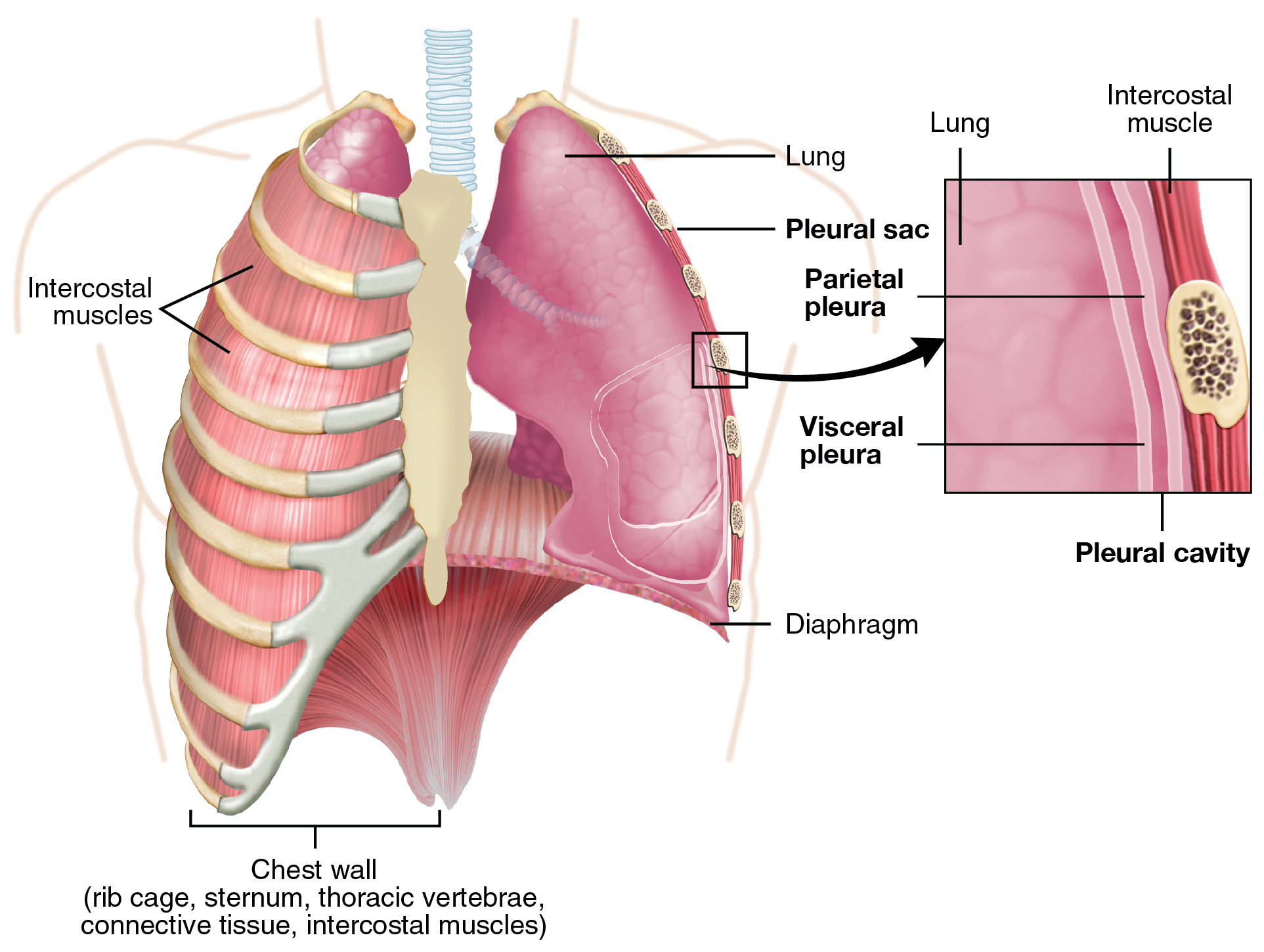
The pleurae perform two major functions:
- Produce pleural fluid that that lubricates surfaces, reduces friction to prevent trauma during breathing, and creates surface tension that helps maintain the position of the lungs against the thoracic wall. This adhesive characteristic of the pleural fluid causes the lungs to enlarge when the thoracic wall expands during ventilation, allowing the lungs to fill with air.
- The pleurae also create a division between major organs that prevents interference due to the movement of the organs, while preventing the spread of infection.
Pulmonary Ventilation
The difference in pressures drives pulmonary ventilation because air flows down a pressure gradient, that is, air flows from an area of higher pressure to an area of lower pressure.
- Air flows into the lungs largely due to a difference in pressure; atmospheric pressure is greater than intra-alveolar pressure, and intra-alveolar pressure is greater than intrapleural pressure.
- Air flows out of the lungs during expiration based on the same principle; pressure within the lungs becomes greater than the atmospheric pressure.
Pulmonary ventilation comprises two major steps: inspiration and expiration (see video below). A respiratory cycle is one sequence of inspiration and expiration.
Two muscle groups are used during normal inspiration the diaphragm and the external intercostal muscles. Additional muscles can be used if a bigger breath is required.
- The diaphragm contracts, it moves inferiorly toward the abdominal cavity, creating a larger thoracic cavity and more space for the lungs.
- The external intercostal muscles contract and moves the ribs upward and outward, causing the rib cage to expand, which increases the volume of the thoracic cavity.
Due to the adhesive force of the pleural fluid, the expansion of the thoracic cavity forces the lungs to stretch and expand as well. This increase in volume leads to a decrease in intra-alveolar pressure, creating a pressure lower than atmospheric pressure. As a result, a pressure gradient is created that drives air into the lungs.
Watch the video: Mechanics of breathing AIDA Freediving (2 minutes)
The process of normal expiration is passive, meaning that energy is not required to push air out of the lungs.
- The elasticity of the lung tissue causes the lung to recoil, as the diaphragm and intercostal muscles relax following inspiration.
- The thoracic cavity and lungs decrease in volume, causing an increase in interpulmonary pressure. The interpulmonary pressure rises above atmospheric pressure, creating a pressure gradient that causes air to leave the lungs.
There are different types, or modes, of breathing that require a slightly different process to allow inspiration and expiration:
- Quiet breathing, also known as eupnea, is a mode of breathing that occurs at rest and does not require the cognitive thought of the individual. During quiet breathing, the diaphragm and external intercostals must contract.
- Diaphragmatic breathing, also known as deep breathing, requires the diaphragm to contract. As the diaphragm relaxes, air passively leaves the lungs.
- Costal breathing, also known as a shallow breath, requires contraction of the intercostal muscles. As the intercostal muscles relax, air passively leaves the lungs.
- Forced breathing, also known as hyperpnea, is a mode of breathing that can occur during exercise or actions that require the active manipulation of breathing, such as singing.
- During forced breathing, inspiration and expiration both occur due to muscle contractions. In addition to the contraction of the diaphragm and intercostal muscles, other accessory muscles must also contract.
- During forced inspiration, muscles of the neck contract and lift the thoracic wall, increasing lung volume.
- During forced expiration, accessory muscles of the abdomen contract, forcing abdominal organs upward against the diaphragm. This helps to push the diaphragm further into the thorax, pushing more air out. In addition, accessory muscles help to compress the rib cage, which also reduces the volume of the thoracic cavity.
- During forced breathing, inspiration and expiration both occur due to muscle contractions. In addition to the contraction of the diaphragm and intercostal muscles, other accessory muscles must also contract.
Concept Check
- Breathing normally, place your hand on your stomach take in one full respiratory cycle.
- What type of breathing are you doing?
- Keeping your hand on your stomach, take in one large breath and exhale.
- What type of breathing are you doing?
- Complete 10 jumping jacks, once completed, place your hand on your stomach and take in one full respiratory cycle.
- What type of breathing are you doing?
Respiratory Rate and Control of Ventilation
Breathing usually occurs without thought, although at times you can consciously control it, such as when you swim under water, sing a song, or blow bubbles. The respiratory rate is the total number of breaths that occur each minute. Respiratory rate can be an important indicator of disease, as the rate may increase or decrease during an illness or in a disease condition. The respiratory rate is controlled by the respiratory center located within the medulla oblongata in the brain, which responds primarily to changes in carbon dioxide, oxygen, and pH levels in the blood.
The normal respiratory rate of a child decreases from birth to adolescence:
- A child under 1 year of age has a normal respiratory rate between 30 and 60 breaths per minute.
- By the time a child is about 10 years old, the normal rate is closer to 18 to 30.
- By adolescence, the normal respiratory rate is similar to that of adults, 12 to 18 breaths per minute.
Watch the video: Overview of the Respiratory System, Animation (5 minutes)
Media 4.3. Overview of the Respiratory System [Online video]. Copyright 2019 by Alila Medical Media.
Medical Terms not Easily Broken into Word Parts
Common Respiratory Abbreviations
Medical Specialties and Procedures Related to the Respiratory System
Pulmonologist
Respiratory medicine is concerned with the diagnosis and treatment of diseases related to the respiratory system. Respiratory medicine requires in-depth knowledge of internal medicine. A physician who specializes in the respiratory system is called a pulmonologist. For more information, visit the American Lung Association’s page on pulmonologists.
Respiratory Therapists (RTs)
Respiratory Therapists (RTs) are health care professionals that monitor, assess and treat people who are having problems breathing. RTs are licensed in the state in which they practice. In Wisconsin, licensure is renewed every two years (American Association for Respiratory Care, 2021a). RTs are trained in ventilation and airway management, cardiopulmonary resuscitation, oxygen and aerosol therapy. They care for patients during cardiac stress-testing, pulmonary function testing, smoking cessation, high-risk births, rehabilitation, and surgery. They treat patients with asthma, bronchitis, COPD, emphysema, heart disease, and pneumonia (American Association for Respiratory Care, 2021b). For more information, visit the American Association for Respiratory Care’s What is a Respiratory Therapist? web page.
Thoracic Surgeon
A thoracic surgeon refers to a surgeon who has specialized in either thoracic (chest) surgery or cardiothoracic (heart and chest) surgery and care or perform surgery for patients with serious conditions of the chest (American Board of Thoracic Surgery, n.d.). To learn more, visit the American Board of Thoracic Surgery web page.
Test Yourself
Use these practice activities to review the concepts in this chapter. If you prefer, there is a printable version of these activities.
Identify meanings of key word components of the respiratory system.
Apply the rules of medical language to pronounce, break into word parts, and define the following terms.
Practice pronouncing and defining these medical terms that are not easily broken into word parts.
Practice pronouncing and defining these commonly abbreviated terms.
Label the following respiratory system structures.
Test your knowledge by answering the questions below.
References
American Association for Respiratory Care. (2021a). Respiratory Therapist State Licensure Information. https://www.aarc.org/advocacy/state-society-resources/state-licensure-information/https://www.aarc.org/careers/what-is-an-rt/
American Association for Respiratory Care. (2021b). What is an RT? https://www.aarc.org/careers/what-is-an-rt/
American Board of Thoracic Surgery. (n.d.). What is a thoracic surgeon? https://www.abts.org/ABTS/Public/For_Patients/Patient_Landing_Page_v2.aspx
Kimble, Brenda. (2019). Know your providers: What does a pulmonologist do? American Lung Association. https://www.lung.org/blog/know-your-providers-pulmonologist
Chapter Attributions
This chapter was adapted by Jerry Casteel from “Respiratory System” by Stacey Grimm; Coleen Allee; Elaine Strachota; Laurie Zielinski; Traci Gotz; Micheal Randolph; and Heidi Belitz. Licensed under a CC BY 4.0 license.
Media Attributions
Mechanics of breathing AIDA Freediving by Steven Chandra is licensed under the Standard YouTube license.
Overview of the Respiratory System, Animation by Alila Medical Media is licensed under the Standard YouTube license.
unconsciously regulates
The external nose consists of the surface and skeletal structures that result in the outward appearance of the nose and contribute to its numerous functions
nasal cavity
the flexible portion you can touch with your fingers (Betts, et al., 2013)
located at the anterior region of the nasal cavity and is composed of bone
located at the posterior portion of the nasal cavity and consists of muscle tissue
excessive flow or discharge from the nasal cavity (runny nose)
short microscopic hairlike vibrating structures
The pharynx is a tube formed by skeletal muscle and lined by mucous membrane that is continuous with that of the nasal cavities (Betts, et al., 2013). Also known as the throat.
pertaining to the pharynx
lymph cells, a type of white blood cell
The uvula is a small bulbous, teardrop-shaped structure located at the apex of the soft palate (Betts, et al., 2013)
The nasopharynx serves as an airway and is continuous with the nasal cavity
The oropharynx is a passageway for both air and food and borders the nasopharynx and the oral cavity (Betts, et al., 2013)
pertaining to the tongue
pertaining to below
pertaining to behind
Pertaining to front
pertaining to behind
The larynx is a cartilaginous structure inferior to the laryngopharynx that connects the pharynx to the trachea and helps regulate the volume of air that enters and leaves the lungs (Betts. et al., 2013) AKA the voice box
The epiglottis, attached to the thyroid cartilage, is a very flexible piece of elastic cartilage that covers the opening of the trachea (Betts. et al., 2013)
The glottis is composed of the vestibular folds, the true vocal cords, and the space between these folds (Betts et al, 2013)
The trachea (windpipe) extends from the larynx toward the lungs
a flexible membrane that closes the posterior surface of the trachea, connecting the C-shaped cartilages
ridge of cartilage that separates the two main bronchi
A concave region where blood vessels, lymphatic vessels, and nerves also enter the lungs
The major functions of the conducting zone are to provide a route for incoming and outgoing air, remove debris and pathogens from the incoming air, and warm and humidify the incoming air. Several structures within the conducting zone perform other functions as well. The epithelium of the nasal passages, for example, is essential to sensing odors, and the bronchial epithelium that lines the lungs can metabolize some airborne carcinogens (Betts, et al., 2013).
the respiratory zone includes structures that are directly involved in gas exchange (Betts, et al., 2013)
a tube composed of smooth muscle and connective tissue (Betts. et al., 2013)
A flat, dome shaped muscle located at the base of the lungs and thoracic cavity
is an indentation on the surface of the left lung
red blood cells
artery that arises from the pulmonary trunk
rest and relaxation phase
flight or fight response
serous membrane surrounding each lung (plural = pleurae)
inhalation or process of breathing air into the lungs
exhalation or the process of causing air to leave the lungs
normal breathing
forced breathing or breathing that is excessive

