11 Sensory Systems
Learning Objectives
- Apply the rules of medical language to build, analyze, spell, pronounce, abbreviate, and define terms as they relate to the sensory system
- Identify meanings of key word components of the sensory system
- Use terms related to the sensory system
Sensory System Word Parts
Click on prefixes, combining forms, and suffixes to reveal a list of word parts to memorize for the Sensory System.
Introduction to the Sensory Systems
Ask anyone what the senses are, and they are likely to list the five major senses as taste, smell, touch, hearing, and sight. However, these are not all of the senses. The most obvious omission from this list is balance. Touch can be further subdivided into pressure, vibration, stretch, and hair-follicle position, on the basis of the type of mechanoreceptors that perceive these touch sensations. Other overlooked senses include temperature perception by thermoreceptors and pain perception by nociceptors.
Within the realm of physiology, senses can be classified as either general or special. A general sense is one that is distributed throughout the body and has receptor cells within the structures of other organs. Mechanoreceptors in the skin, muscles, or the walls of blood vessels are examples of this type. General senses often contribute to the sense of touch, as described above, or to proprioception and kinesthesia , or to a visceral sense, which is most important to autonomic functions. A special sense is one that has a specific organ devoted to it, namely the eye, inner ear, tongue, or nose. The figure below shows the series of events that lead to stimulation of a sense organ.

Gustation (Taste) and Olfaction (Smell)
Watch Taste & Smell: Crash Course Anatomy & Physiology #16 (10 minutes)
Sensory System Medical Terms
Gustation (Taste)
Gustation is the special sense associated with the tongue. The surface of the tongue, along with the rest of the oral cavity, is lined by a stratified squamous epithelium. Raised bumps called papillae contain the structures for gustatory transduction. There are four types of papillae, based on their appearance:
- circumvallate
- foliate
- filiform
- fungiform
Within the structure of the papillae are taste buds that contain specialized gustatory receptor cells for the transduction of taste stimuli. These receptor cells are sensitive to the chemicals contained within foods that are ingested, and they release neurotransmitters based on the amount of the chemical in the food. Neurotransmitters from the gustatory cells can activate sensory neurons in the facial, glossopharyngeal, and vagus cranial nerves.
Only a few recognized submodalities exist within the sense of taste, or gustation. Until recently, only four tastes were recognized: sweet, salty, sour, and bitter. Research at the turn of the 20th century led to recognition of the fifth taste, umami, during the mid-1980s. Very recent research has suggested that there may also be a sixth taste for fats, or lipids.
Olfaction (Smell)
Like taste, olfaction, is also responsive to chemical stimuli. The olfactory receptor neurons are located in a small region within the superior nasal cavity. The nasal epithelium, including the olfactory cells, can be harmed by airborne toxic chemicals.] Scent receptor messages travel to the cerebrum, specifically to the primary olfactory cortex that is located in the inferior and medial areas of the temporal lobe and additionally to the hypothalamus, where smells become associated with long-term memory and emotional response.
Concept Check
- Which parts of the brain are active with recording and associating scents with memories and emotions?
- Recall and list the four types of papillae (taste buds) found on the tongue.
Audition (Hearing), Equilibrium (Balance), and Somatosensation (Touch)
Watch Hearing & Balance: Crash Course Anatomy & Physiology #17 (11 minutes)
Audition (Hearing)
Hearing, or audition, is the transduction of sound waves into a neural signal that is made possible by the structures of the ear (see Figure 11.2).
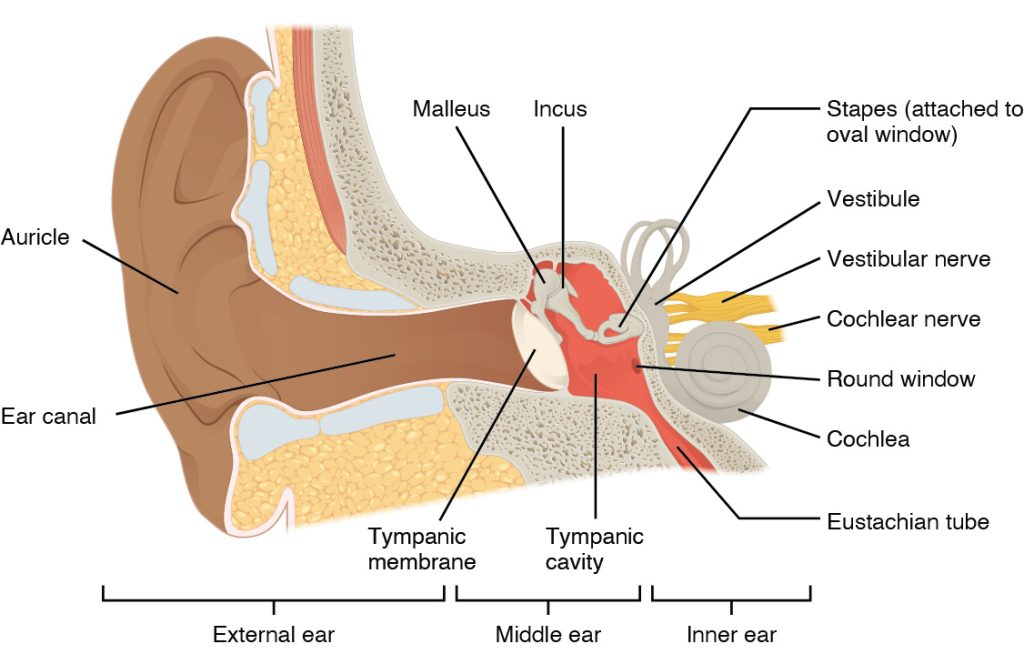
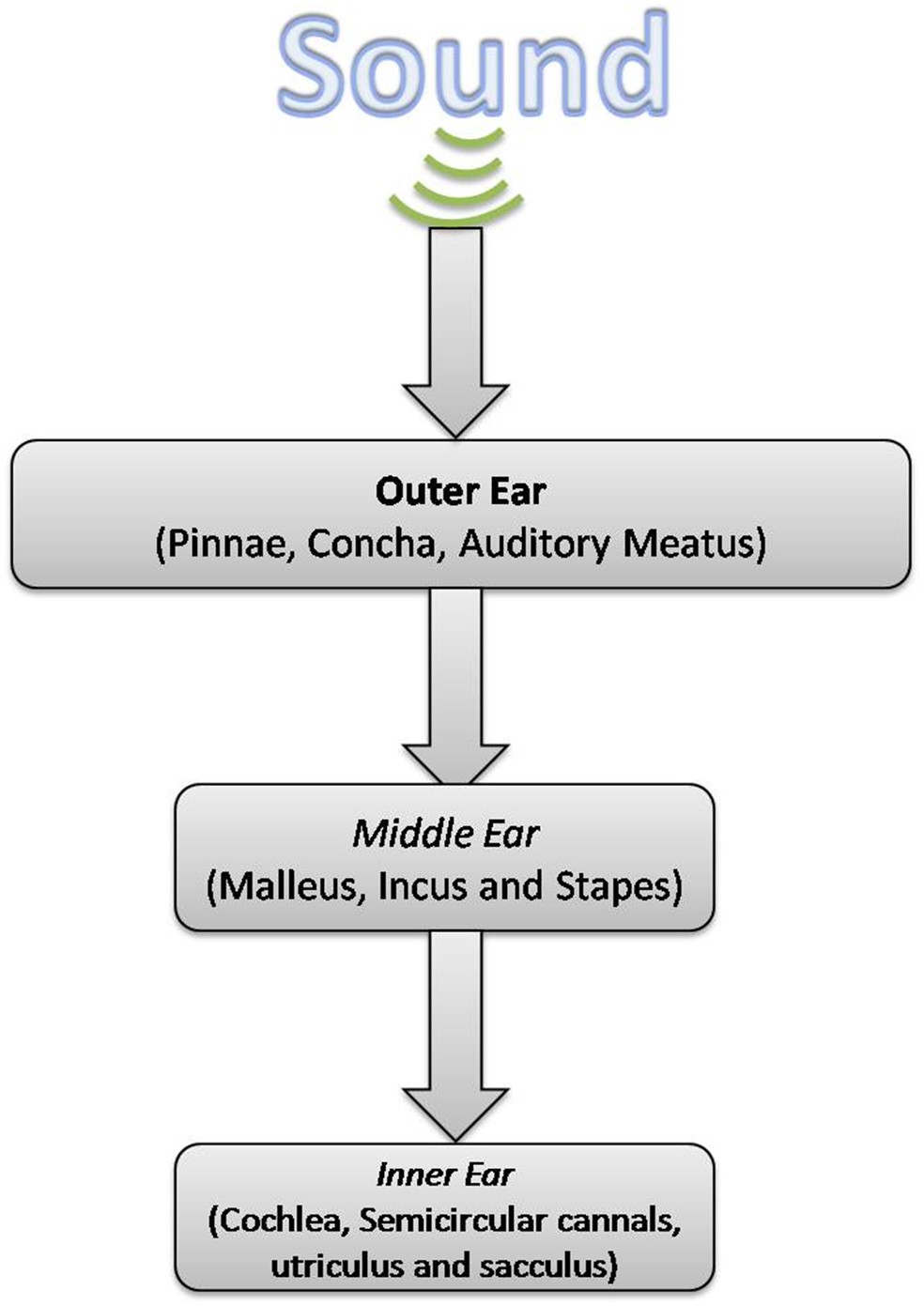
- The external ear consists of the auricle sometimes referred to as the pinna, ear canal, and tympanic membrane.
- The C-shaped curves of the auricle direct sound waves toward the auditory canal. The canal enters the skull through the external auditory meatus of the temporal bone. At the end of the auditory canal is the tympanic membrane, which vibrates after it is struck by sound waves.
- The middle ear consists of the ossicles, oval window, and tympanic membrane.
- The three ossicles are the malleus, incus, and stapes, which are Latin names that roughly translate to hammer, anvil, and stirrup. The malleus is attached to the tympanic membrane and articulates with the incus. The incus, in turn, articulates with the stapes. The stapes is then attached to the inner ear, where the sound waves will be transduced into a neural signal. Vibrations of the ossicles travel through the oval window, moving fluid in a wave-like motion. The frequency of the fluid waves match the frequencies of the sound waves. The middle ear is connected to the pharynx through the Eustachian tube, which helps equilibrate air pressure across the tympanic membrane. The tube is normally closed but will pop open when the muscles of the pharynx contract during swallowing or yawning.
- The inner ear is often described as a bony labyrinth, as it is composed of a series of canals embedded within the temporal bone.
- It consists of the cochlea that is responsible for hearing and the vestibule that is responsible for balance. The neural signals from these two regions are relayed to the brain stem through separate fiber bundles. However, these two distinct bundles travel together from the inner ear to the brain stem as the vestibulocochlear nerve. Sound is transduced into neural signals within the cochlear region of the inner ear, which contains the sensory neurons of the spiral ganglia. These ganglia are located within the spiral-shaped cochlea of the inner ear. The cochlea is attached to the stapes through the oval window.
The image below is a cross-sectional view of the cochlea that shows the scala vestibuli and scala tympani run along both sides of the cochlear duct (see Figure 11.4). The cochlear duct contains several organs of Corti, which tranduce the wave motion of the two scala into neural signals. The organs of Corti lie on top of the basilar membrane, which is the side of the cochlear duct located between the organs of Corti and the scala tympani. As the fluid waves move through the scala vestibuli and scala tympani, the basilar membrane moves at a specific spot, depending on the frequency of the waves. Higher frequency waves move the region of the basilar membrane that is close to the base of the cochlea. Lower frequency waves move the region of the basilar membrane that is near the tip of the cochlea.
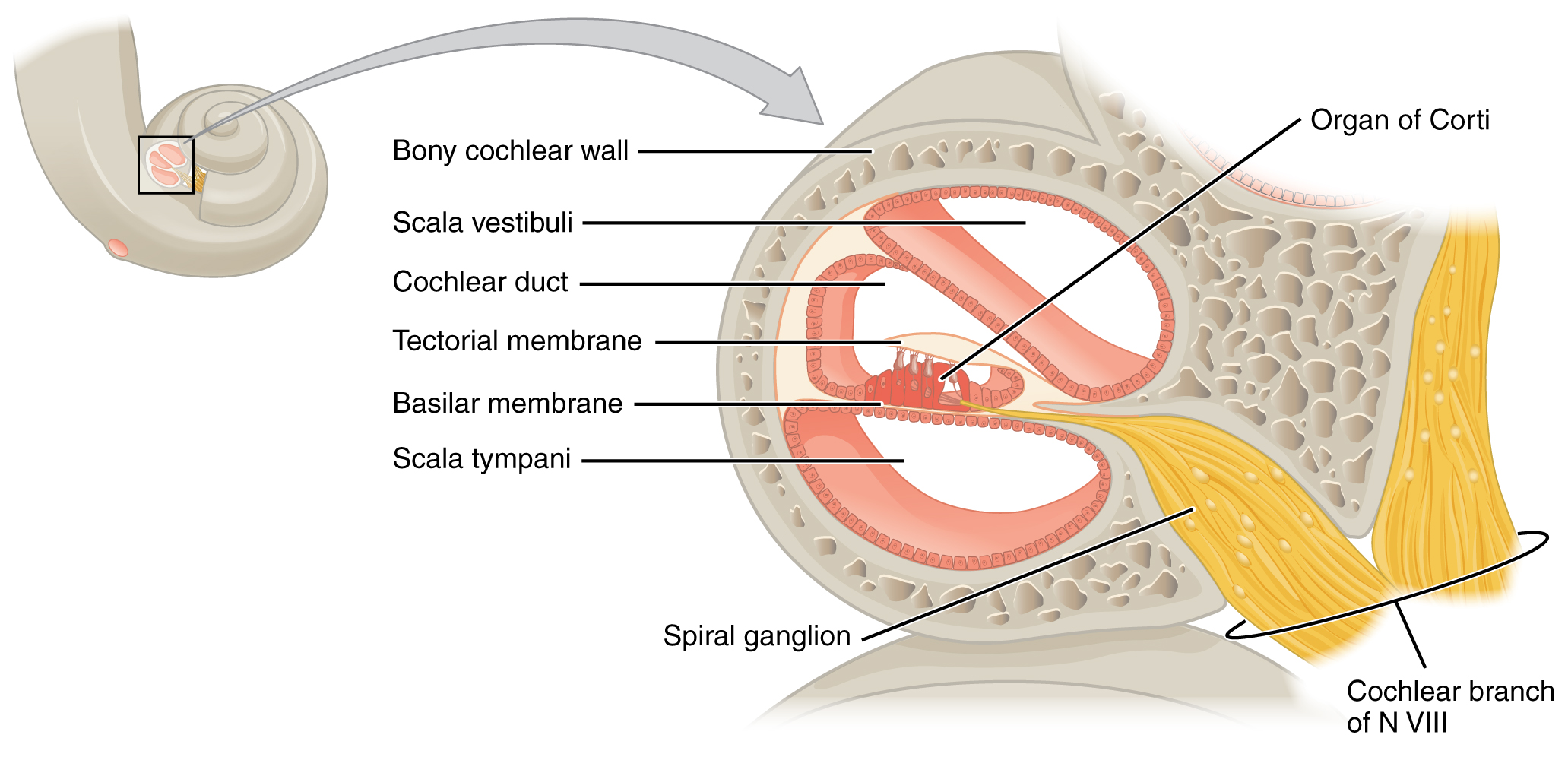
The cochlea encodes auditory stimuli for frequencies between 20 and 20,000 Hz, which is the range of sound that human ears can detect. The unit of Hertz measures the frequency of sound waves in terms of cycles produced per second. Frequencies as low as 20 Hz are detected by hair cells at the apex, or tip, of the cochlea. Frequencies in the higher ranges of 20 KHz are encoded by hair cells at the base of the cochlea, close to the round and oval windows. Most auditory stimuli contain a mixture of sounds at a variety of frequencies and intensities (represented by the amplitude of the sound wave). The hair cells along the length of the cochlear duct, which are each sensitive to a particular frequency, allow the cochlea to separate auditory stimuli by frequency, just as a prism separates visible light into its component colors. To learn more about hearing and the cochlea, watch this Medline Plus video.
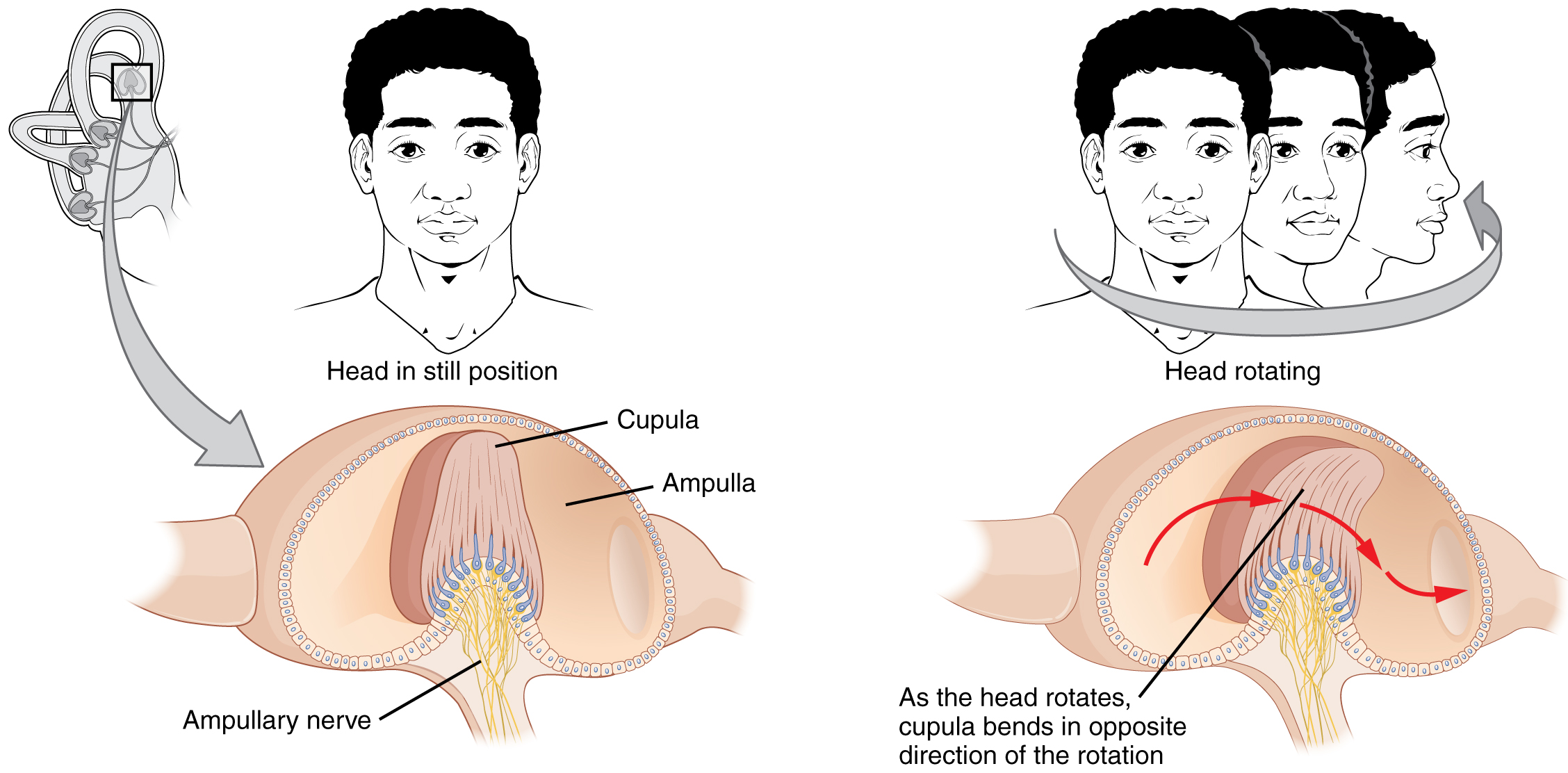
Equilibrium (Balance)
Along with audition, the inner ear is responsible for encoding information about equilibrium. The cells that sense head position, head movement, and body motion are located within the vestibule of the inner ear. Head position is sensed by otolith organs, whereas head movement is sensed by the semicircular canals (see Figure 11.5). The neural signals generated in the vestibular ganglion are transmitted through the vestibulocochlear nerve to the brain stem and cerebellum.
Somatosensation (Touch)
Somatosensation is considered a general sense, as opposed to the special senses discussed in this section. Somatosensation is the group of sensory modalities that are associated with touch, proprioception, and interoception. These modalities include pressure, vibration, light touch, tickle, itch, temperature, pain, proprioception, and kinesthesia. This means that its receptors are not associated with a specialized organ, but are instead spread throughout the body in a variety of organs. Many of the somatosensory receptors are located in the skin, but receptors are also found in muscles, tendons, joint capsules, ligaments, and in the walls of visceral organs.
The two types of somatosensory signals that are transduced by free nerve endings are pain and temperature. Temperature receptors are stimulated when local temperatures differ from body temperature. Some thermoreceptors are sensitive to just cold and others to just heat. Nociception is the sensation of potentially damaging stimuli. Mechanical, chemical, or thermal stimuli beyond a set threshold will elicit painful sensations. Stressed or damaged tissues release chemicals that activate receptor proteins in the nociceptors.
Concept Check
- What structure exists within the ear to assist with maintaining equilibrium?
- What are the medical terms used to describe the sense of taste and touch?
Ear Anatomy Labeling Activity
Vision (Sight)
Watch Vision: Crash Course Anatomy & Physiology #18 (10 minutes)
Vision is the special sense of sight that is based on the transduction of light stimuli received through the eyes. The eyes are located within either orbit in the skull. The bony orbits surround the eyeballs, protecting them and anchoring the soft tissues of the eye (see Figure 11.6). The eyelids, with lashes at their leading edges, help to protect the eye from abrasions by blocking particles that may land on the surface of the eye.
The inner surface of each lid is a thin membrane known as the palpebral conjunctiva. The conjunctiva extends over the sclera, connecting the eyelids to the eyeball. Tears are produced by the lacrimal gland, located beneath the lateral edges of the nose. Tears produced by this gland flow through the lacrimal duct to the medial corner of the eye, where the tears flow over the conjunctiva, washing away foreign particles.
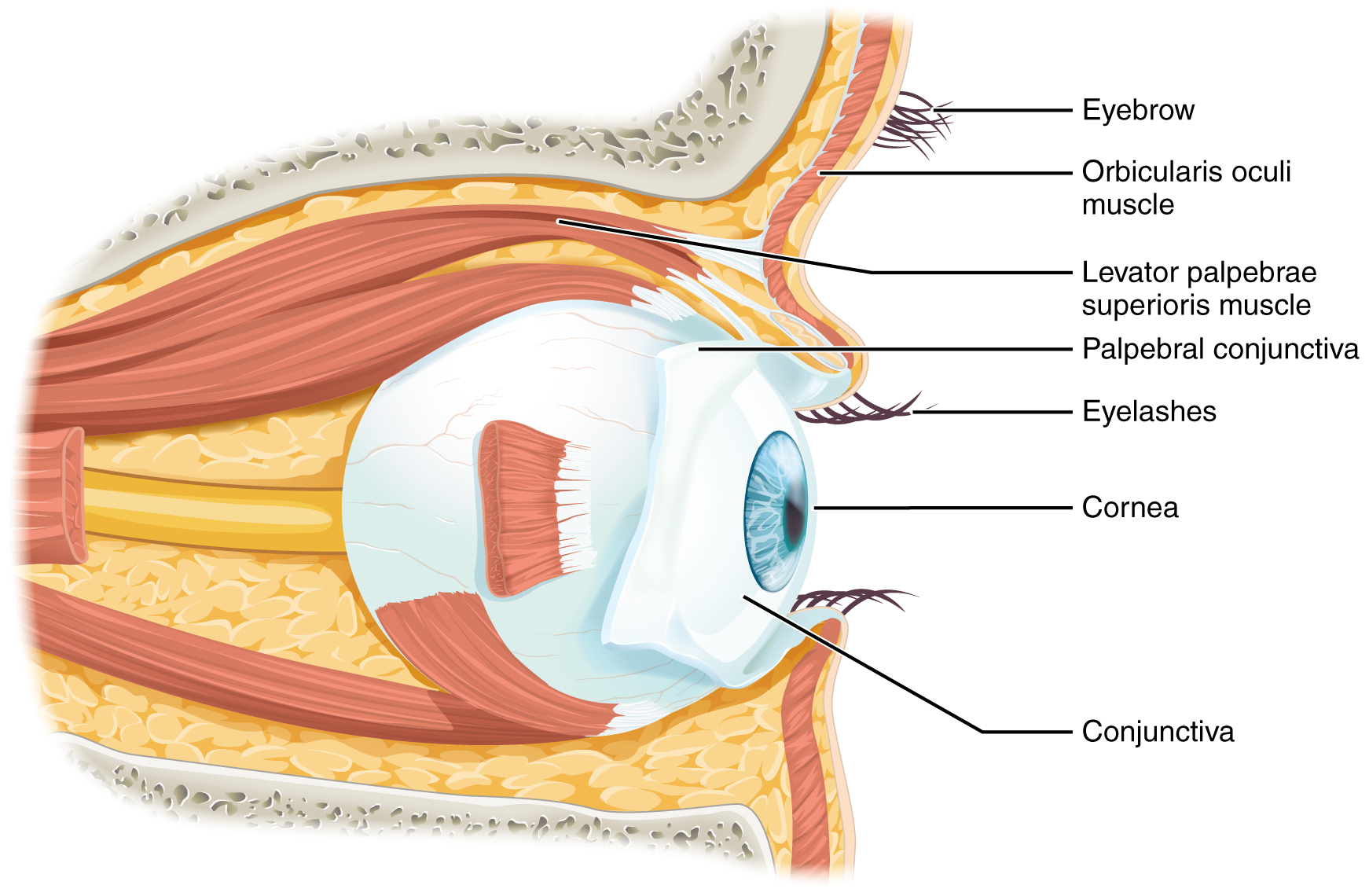
Movement of the eye within the orbit is accomplished by the contraction of six extraocular muscles that originate from the bones of the orbit and insert into the surface of the eyeball. Four of the muscles are arranged at the cardinal points around the eye and are named for those locations. They are the:
- superior rectus
- medial rectus
- inferior rectus
- lateral rectus.
When each of these muscles contract, the eye moves toward the contracting muscle. For example, when the superior rectus contracts, the eye rotates to look up.
The eye itself is a hollow sphere composed of three layers of tissue.
- The outermost layer is the fibrous tunic, which includes the white sclera and clear cornea. The sclera accounts for five sixths of the surface of the eye, most of which is not visible, though humans are unique compared with many other species in having so much of the “white of the eye” visible (see Figure 11.7). The transparent cornea covers the anterior tip of the eye and allows light to enter the eye.
- The middle layer of the eye is the vascular tunic, which is mostly composed of the choroid, ciliary body, and iris. The choroid is a layer of highly vascularized connective tissue that provides a blood supply to the eyeball. The choroid is posterior to the ciliary body, a muscular structure that is attached to the lens by zonule fibers. These two structures bend the lens, allowing it to focus light on the back of the eye. Overlaying the ciliary body, and visible in the anterior eye, is the iris—the colored part of the eye. The iris is a smooth muscle that opens or closes the pupil, which is the hole at the center of the eye that allows light to enter. The iris constricts the pupil in response to bright light and dilates the pupil in response to dim light.
- The innermost layer of the eye is the neural tunic, or retina, which contains the nervous tissue responsible for photoreception.
The eye is also divided into two cavities:
- The anterior cavity
- The anterior cavity is the space between the cornea and lens, including the iris and ciliary body. It is filled with a watery fluid called the aqueous humor.
- The posterior cavity
- The posterior cavity is the space behind the lens that extends to the posterior side of the interior eyeball, where the retina is located. The posterior cavity is filled with a more viscous fluid called the vitreous humor.
The retina is composed of several layers and contains specialized cells for the initial processing of visual stimuli. The photoreceptors (rods and cones) change their membrane potential when stimulated by light energy. The change in membrane potential alters the amount of neurotransmitter that the photoreceptor cells release onto bipolar cells in the outer synaptic layer. It is the bipolar cell in the retina that connects a photoreceptor to a retinal ganglion cell (RGC) in the inner synaptic layer. There, amacrine cells additionally contribute to retinal processing before an action potential is produced by the RGC. The axons of RGCs, which lie at the innermost layer of the retina, collect at the optic disc and leave the eye at the optic nerve (see Figure 11.7). Because these axons pass through the retina, there are no photoreceptors at the very back of the eye, where the optic nerve begins. This creates a “blind spot” in the retina, and a corresponding blind spot in our visual field.
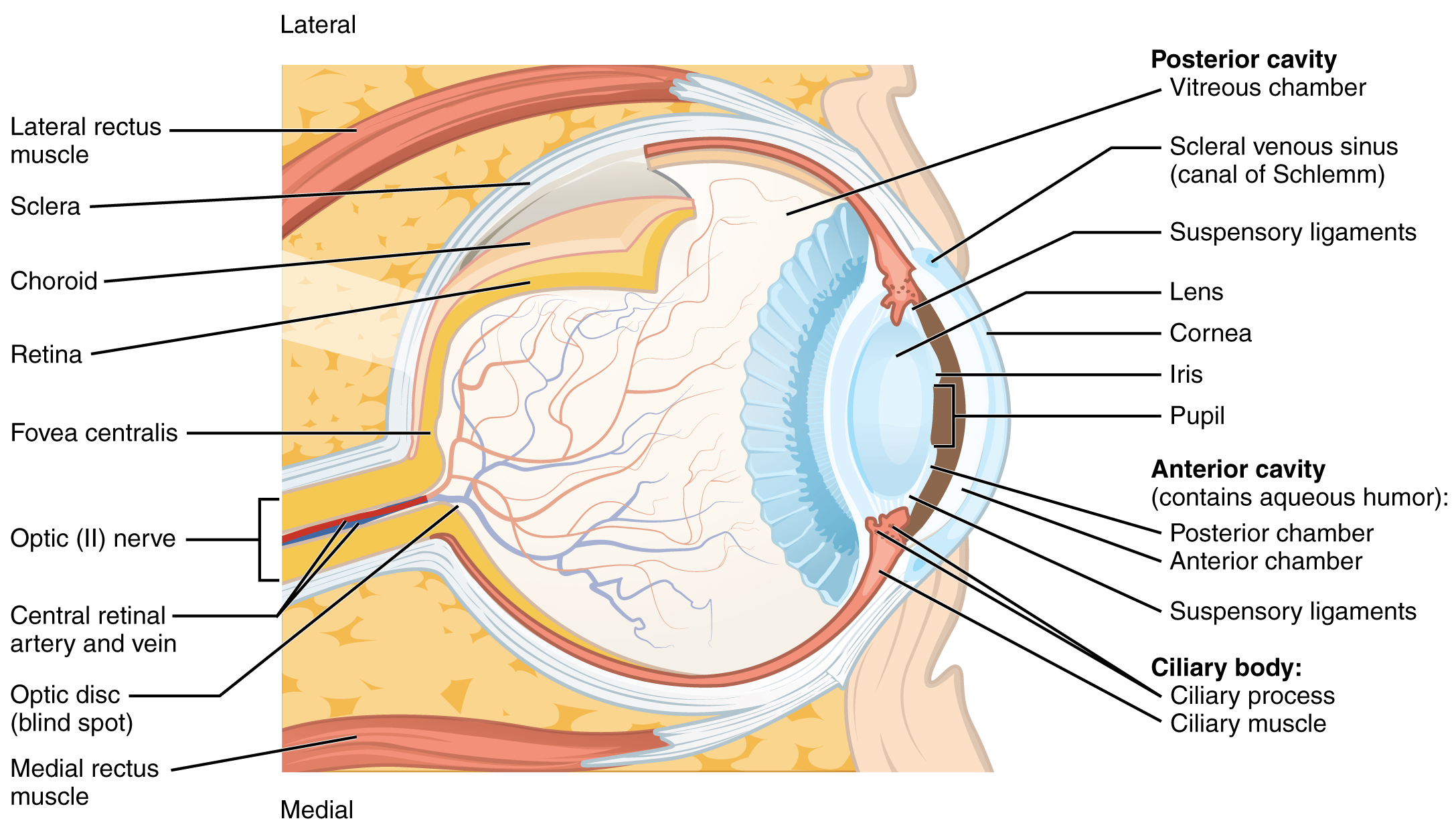
Photoreceptors in the retina (rods and cones) are located behind the axons, RGCs, bipolar cells, and retinal blood vessels. A significant amount of light is absorbed by these structures before the light reaches the photoreceptor cells. At the exact center of the retina is a small area known as the fovea. At the fovea, the retina lacks the supporting cells and blood vessels, and only contains photoreceptors. Therefore, visual acuity, is greatest at the fovea. This is because the fovea is where the least amount of incoming light is absorbed by other retinal structures (see Figure 11.7). As one moves in either direction from this central point of the retina, visual acuity drops significantly.
Example: Visual Acuity (VA) between the fovea and peripheral retina.
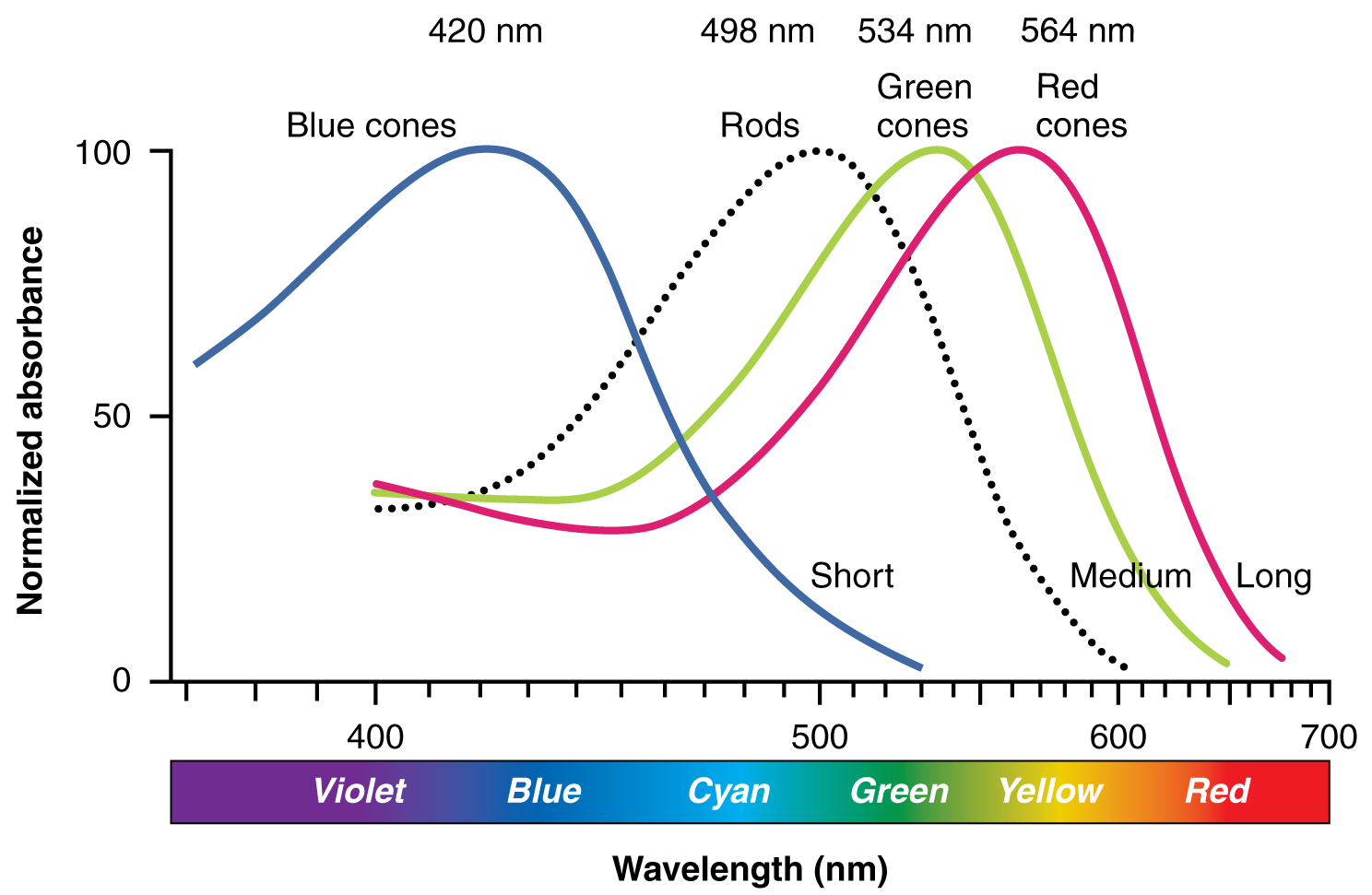
There are three types of cone opsins, that are sensitive to different wavelengths of light and provide us with color vision. By comparing the activity of the three different cones, the brain can extract color information from visual stimuli (see Figure 11.8). For example, a bright blue light that has a wavelength of approximately 450 nm would activate the “red” cones minimally, the “green” cones marginally, and the “blue” cones predominantly. The relative activation of the three different cones is calculated by the brain, which perceives the color as blue. However, cones cannot react to low-intensity light, and rods do not sense the color of light. Therefore, our low-light vision is, in essence, in grayscale. In other words, in a dark room, everything appears as a shade of gray. If you think that you can see colors in the dark, it is most likely because your brain knows what color something is and is relying on that memory.
Medical Specialties and Procedures Related to the Sensory Systems
Several medical specialties support the sensory systems. An optometrist is an eye specialist that examines and evaluates for ocular pathology and an optometrist prescribes corrective lenses. An ophthalmologist evaluates and manage eye pathology as well as perform surgery. An otorhinolaryngologist (ENT) is a physician that specializes in ears, nose and throat treatment and conditions. An audiologist evaluates and manages individuals with hearing loss.
Ophthalmic Medical Assistant
Ophthalmic Medical Assistants work in ophthalmic and optometric practices and in retail optical settings. Ophthalmic Assistants perform pre-screening and specialty testing, assist with dispensing glasses and contact lenses, and perform office management duties including maintaining patient information and billing and insurance processes.
Ophthalmic Technician
Optometric Technicians work under the supervision of an optometrist or ophthalmologist. Optometric Technicians assist an optometrist during eye exams and other optometric procedures, providing eye health tests and consultations.
Test Yourself
Use these practice activities to review the concepts in this chapter. If you prefer, there is a printable version of these activities.
Identify meanings of key word components of the sensory systems.
Apply the rules of medical language to pronounce, break into word parts, and define the following terms.
Practice pronouncing and defining these medical terms that are not easily broken into word parts.
Practice pronouncing and defining these commonly abbreviated sensory system terms.
Use terms related to the sensory systems:
Label the following sensory system ear anatomy.
Label the following sensory system eye anatomy.
Place the given medical terms in context to complete the scenarios below.
Test your knowledge by answering the questions below.
Chapter Attributions
This chapter was adapted by Karen Hobbs from “Sensory Systems” by Stacey Grimm; Coleen Allee; Elaine Strachota; Laurie Zielinski; Traci Gotz; Micheal Randolph; and Heidi Belitz. Licensed under a CC BY 4.0 license.
Media Attributions
Taste & Smell: Crash Course Anatomy & Physiology #16 by CrashCourse is licensed under the Standard YouTube license.
Hearing & Balance: Crash Course Anatomy & Physiology #17 by CrashCourse is licensed under the Standard YouTube license.
Vision: Crash Course Anatomy & Physiology #18 by CrashCourse is licensed under the Standard YouTube license.
A sensory neuron that responds to mechanical pressure
specialized neurons that respond to changes in temperature
Sensory neurons that respond to pain
awareness of the position of the body in space
body movement
pertaining to internal organs
Chemical messengers which transmit signals across a chemical synapse from one neuron to another neuron/nerve cell.
pertaining to tongue and throat
Umami is a Japanese word that means delicious taste, and is often translated to mean savory
sense of smell
ear drum
balance
to secrete externally, directly or through a duct
Terms that are named after a place or person.
sharpness of vision

