Open Resources for Nursing (Open RN)
Learning Objectives
- Safely administer medication orally, rectally, and via enteral tubes
- Accurately check medication administration rights three times
- Calculate correct amount of medication to administer
- Explain medication information to patient
- Collect appropriate assessment data prior to and after medication administration
- Modify procedure to reflect variations across the life span
- Document actions and observations
“Enteral” means related to the intestines. The term enteral medication describes medications that are administered into the gastrointestinal tract, including orally (PO), rectally (PR), or through a tube such as a nasogastric (NG) tube, nasointestinal (NI) tube, or percutaneous endoscopic gastrostomy (PEG) tube.
This chapter will review overall concepts related to safe medication administration, as well as specific information regarding the administration of oral medication, rectal medication, and medication via a gastric tube. Information regarding administering injections and intravenous medications can be found in “Administration of Parenteral Medications” and additional information about administering medications via other routes can be found in “Administration of Medications via Other Routes.”
An infection is the invasion and growth of a microorganism within the body. Infection can lead to disease that causes signs and symptoms, resulting in a deviation from the normal structure or functioning of the host. Infection occurs when nonspecific innate immunity and specific adaptive immunity defenses are inadequate to protect an individual against the invasion of a pathogen. The ability of a microorganism to cause disease is called pathogenicity, and the degree to which a microorganism is likely to become a disease is called virulence. Virulence is a continuum. On one end of the spectrum are organisms that are not harmful, but on the other end are organisms that are highly virulent. Highly virulent pathogens will almost always lead to a disease state when introduced to the body, and some may even cause multi-organ and body system failure in healthy individuals. Less virulent pathogens may cause an initial infection, but may not always cause severe illness. Pathogens with low virulence usually result in mild signs and symptoms of disease, such as a low-grade fever, headache, or muscle aches, and some individuals may even be asymptomatic.[1]
An example of a highly virulent microorganism is Bacillus anthracis, the pathogen responsible for anthrax. The most serious form of anthrax is inhalation anthrax. After Bacillus anthracis spores are inhaled, they germinate. An active infection develops, and the bacteria release potent toxins that cause edema (fluid buildup in tissues), hypoxia (a condition preventing oxygen from reaching tissues), and necrosis (cell death and inflammation). Signs and symptoms of inhalation anthrax include high fever, difficulty breathing, vomiting, coughing up blood, and severe chest pains suggestive of a heart attack. With inhalation anthrax, the toxins and bacteria enter the bloodstream, which can lead to multi-organ failure and death of the client.[2]
Primary Pathogens Versus Opportunistic Pathogens
Pathogens can be classified as either primary pathogens or opportunistic pathogens. A primary pathogen can cause disease in a host regardless of the host’s microbiome or immune system. An opportunistic pathogen, by contrast, can cause disease only in situations that compromise the host’s defenses, such as the body’s protective barriers, immune system, or normal microbiome. Individuals susceptible to opportunistic infections include the very young, the elderly, women who are pregnant, clients undergoing chemotherapy, people with immunodeficiencies (such as acquired immunodeficiency syndrome [AIDS]), clients who are recovering from surgery, and those who have nonintact skin (such as a severe wound or burn).[3]
An example of a primary pathogen is enterohemorrhagic Escherichia coli (E. coli) that produces a toxin that leads to severe and bloody diarrhea, inflammation, and renal failure, even in clients with healthy immune systems. Staphylococcus epidermidis, on the other hand, is an opportunistic pathogen that is a frequent cause of healthcare acquired infection.[4] Staphylococcus epidermidis, often referred to as “staph,” is a member of the normal flora of the skin. However, in hospitals, it can grow in biofilms that form on catheters, implants, or other devices that are inserted into the body during surgical procedures. Once inside the body, it can cause serious infections such as endocarditis.[5]
Other members of normal flora can cause opportunistic infections. Some microorganisms that reside harmlessly in one location of the body can cause disease if they are passed to a different body system. For example, E. coli is normally found in the large intestine, but can cause a urinary tract infection if it enters the bladder.[6]
Normal flora can also cause disease when a shift in the environment of the body leads to overgrowth of a particular microorganism. For example, the yeast Candida is part of the normal flora of the skin, mouth, intestine, and vagina, but its population is kept in check by other organisms of the microbiome. When an individual takes antibiotics, bacteria that would normally inhibit the growth of Candida can be killed off, leading to a sudden growth in the population of Candida. An overgrowth of Candida can manifest as oral thrush (growth of yeast on mouth, throat, and tongue) or a vaginal yeast infection. Other scenarios can also provide opportunities for Candida to cause infection. For example, untreated diabetes can result in a high concentration of glucose in a client’s saliva that provides an optimal environment for the growth of Candida, resulting in oral thrush. Immunodeficiencies, such as those seen in clients with HIV, AIDS, and cancer, can also lead to Candida infections because the body's immune system is weakened in these conditions and unable to fight off the Candida.[7]
Stages of Pathogenesis
To cause disease, a pathogen must successfully achieve four stages of pathogenesis to become an infection: exposure, adhesion (also called colonization), invasion, and infection. The pathogen must be able to gain entry to the host, travel to the location where it can establish an infection, evade or overcome the host’s immune response, and cause damage (i.e., disease) to the host. In many cases, the cycle is completed when the pathogen exits the host and is transmitted to a new host.[8]
Exposure
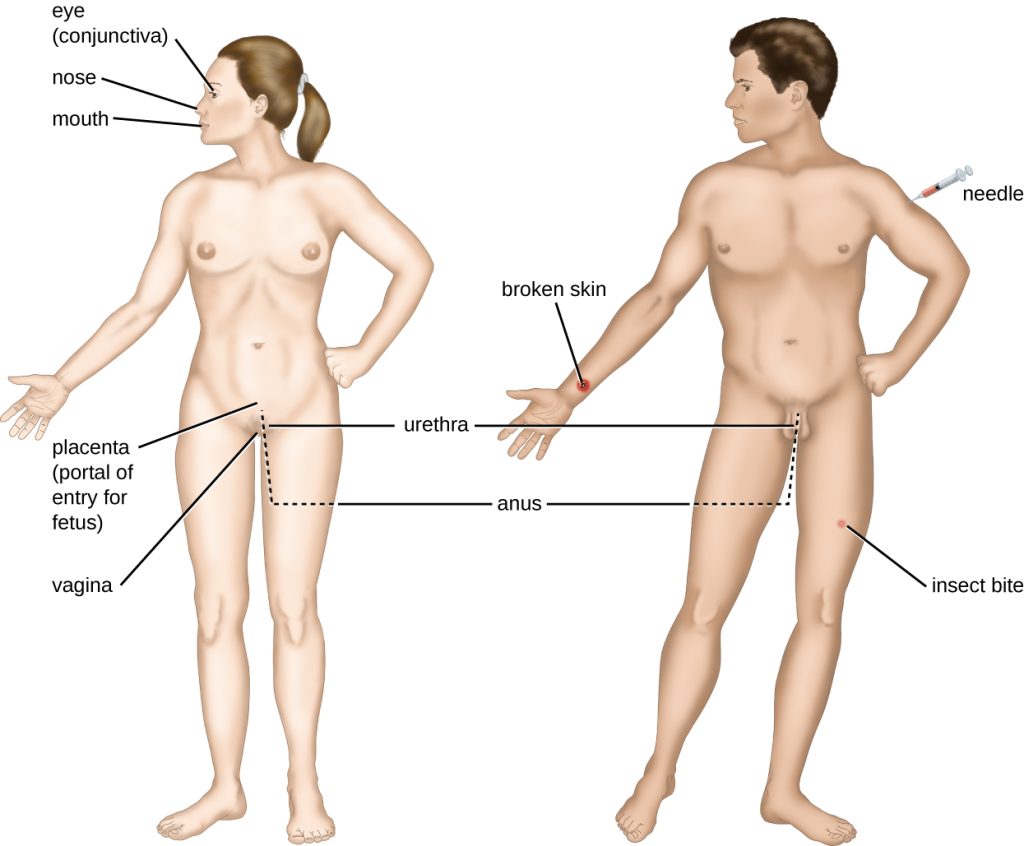
An encounter with a potential pathogen is known as exposure. The food we eat and the objects we touch are all ways that we can come into contact with potential pathogens. Yet, not all contacts result in infection and disease. For a pathogen to cause disease, it needs to be able to gain access into host tissue. An anatomic site through which pathogens can pass into host tissue is called a portal of entry. Portals of entry are locations where the host cells are in direct contact with the external environment, such as the skin, mucous membranes, respiratory, and digestive systems. Portals of entry are illustrated in Figure 9.11.[9],[10]
Adhesion
Following initial exposure, the pathogen adheres at the portal of entry. The term adhesion refers to the capability of pathogenic microbes to attach to the cells of the body, also referred to as colonization.[11]
Invasion
After successful adhesion, the invasion proceeds. Invasion means the spread of a pathogen throughout local tissues or the body. Pathogens may also produce virulence factors that protect them against immune system defenses and determine the degree of tissue damage that occurs. Intracellular pathogens like viruses achieve invasion by entering the host’s cells and reproducing.[12]
Infection
Following invasion, successful multiplication of the pathogen leads to infection. Infections can be described as local, secondary, or systemic, depending on the extent of the infection.[13]
A local infection is confined to a small area of the body, typically near the portal of entry. For example, a hair follicle infected by Staphylococcus aureus infection may result in a boil around the site of infection, but the bacterium is largely contained to this small location. Other examples of local infections that involve more extensive tissue involvement include urinary tract infections confined to the bladder or pneumonia confined to the lungs. Localized infections generally demonstrate signs of inflammation, such as redness, swelling, warmth, pain, and purulent drainage. However, extensive tissue involvement can also cause decreased functioning of the organ affected.[14]
A secondary infection is an infection that occurs during or after treatment for a different infection. It may be caused by the treatment for the first infection or a result of a diminished immune system or the elimination of normal flora. For example, a yeast infection that occurs after a client is treated with antibiotics is a secondary infection.[15]
When an infection becomes disseminated throughout the body, it is called a systemic infection. For example, infection by the varicella-zoster virus typically gains entry through a mucous membrane of the upper respiratory system. It then spreads throughout the body, resulting in a classic red rash associated with chicken pox. Because these lesions are not sites of initial infection, they are signs of a systemic infection. Systemic infections can cause fever, increased heart and respiratory rates, lethargy, malaise, anorexia, and tenderness and enlargement of the lymph nodes.[16]
Sometimes a primary infection can lead to a secondary infection by an opportunistic pathogen. For example, when a client experiences a primary infection from influenza, it can damage and decrease the defense mechanisms of the lungs, making the client more susceptible to a secondary pneumonia by a bacterial pathogen like Haemophilus influenzae. Additionally, treatment of the primary infection may lead to a secondary infection caused by an opportunistic pathogen. For example, antibiotic therapy targeting the primary infection alters the normal flora and creates an opening for opportunistic pathogens like Clostridium difficile or Candida Albicans to cause a secondary infection.[17]
Bacteremia, SIRS, Sepsis, and Septic Shock
When infection occurs, pathogens can enter the bloodstream. The presence of bacteria in blood is called bacteremia. If bacteria are both present and multiplying in the blood, it is called septicemia.[18]
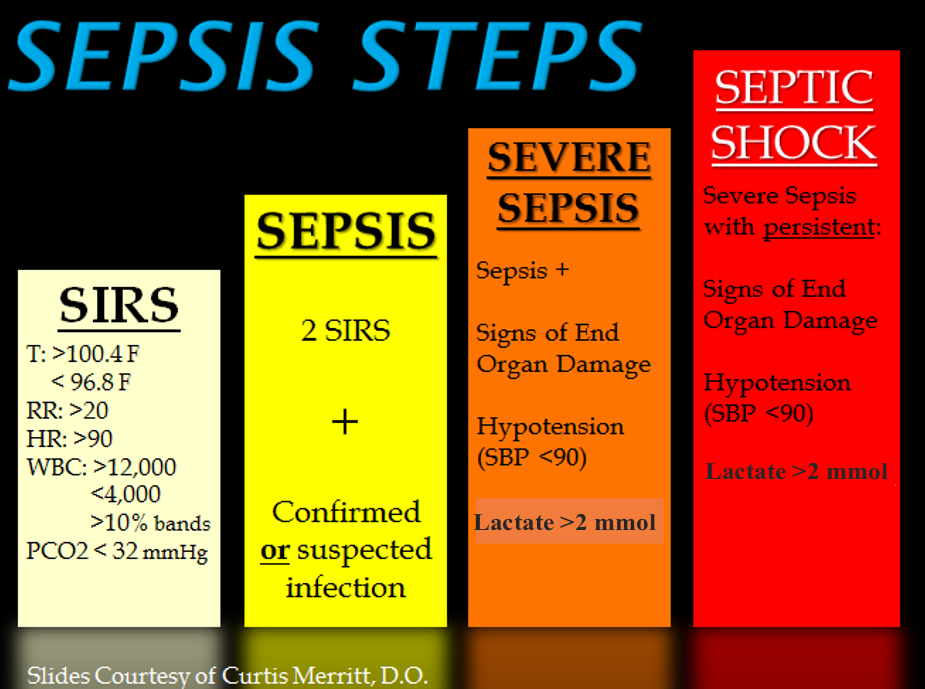
Systemic inflammatory response syndrome (SIRS) is an exaggerated inflammatory response that affects the entire body. It is the body’s reaction to a noxious stressor, including causes such as infection and acute inflammation, but other conditions can trigger it as well. Signs of SIRS are as follows:
- Body temperature over 38 or under 36 degrees Celsius
- Heart rate greater than 90 beats/minute
- Respiratory rate greater than 20 breaths/minute or PaCO2 less than 32 mmHg
- White blood cell count greater than 12,000 or less than 4,000 /microliters or over 10% of immature forms (bands)[19]
Even though the purpose of SIRS is to defend against a noxious stressor, the uncontrolled release of massive amounts of cytokines, called cytokine storm, can lead to organ dysfunction and even death.[20]
Sepsis refers to SIRS that is caused by an infection. Sepsis occurs when an existing infection triggers an exaggerated inflammatory reaction throughout the body. If left untreated, sepsis causes tissue and organ damage. It can quickly spread to multiple organs and is a life-threatening medical emergency.
Sepsis causing damage to one or more organs (such as the kidneys) is called severe sepsis. Severe sepsis can lead to septic shock, a life-threatening decrease in blood pressure (systolic pressure <90 mm Hg) that prevents cells and other organs from receiving enough oxygen and nutrients, causing multi-organ failure and death. See Figure 9.12[21] for an illustration of the progression of sepsis from SIRS to septic shock.
Unfortunately, almost any type of infection in any individual can lead to sepsis. Infections that lead to sepsis most often start in the lungs, urinary tract, gastrointestinal tract, or skin. Some people are especially at risk for developing sepsis, such as adults over age 65; children younger than one year old; people who are immunocompromised or have chronic medical conditions, such as diabetes, lung disease, cancer, and kidney disease; and survivors of a previous sepsis episode.[22]
In addition to exhibiting signs of SIRS, clients with sepsis may also have additional signs such as elevated fever and shivering, confusion, shortness of breath, pain or discomfort, and clammy or sweaty skin. Diligent nursing care is vital for recognizing early signs of SIRS and sepsis and promptly notifying the health care provider and/or following sepsis protocols in place at your health care facility.[23]
Use the following to read more information about sepsis:
- Read more information about sepsis at the CDC's Sepsis web page.
- Read the CDC infographic on Protect Your Patients From Sepsis.
- Read an article about caring for clients with sepsis titled Something Isn't Right: The Subtle Changes of Early Deterioration.
- Read more about the Surviving Sepsis Campaign with early recognition and treatment of sepsis using the Hour-1 Bundle.
Toxins
Some pathogens release toxins that are biological poisons that assist in their ability to invade and cause damage to tissues. For example, Botulinum toxin is a neurotoxin produced by the gram-positive bacterium Clostridium botulinum that is an acutely toxic substance because it blocks the release of the neurotransmitter acetylcholine. The toxin’s blockage of acetylcholine results in muscle paralysis with the potential to stop breathing due to its effect on the respiratory muscles. This condition is referred to as botulism, a type of food poisoning that can be caused by improper sterilization of canned foods. However, because of its paralytic action, low concentrations of Botox are also used for beneficial purposes such as cosmetic procedures to remove wrinkles and in the medical treatment of overactive bladder.[24]
Another type of neurotoxin is tetanus toxin, which is produced by the gram-positive bacterium Clostridium tetani. Tetanus toxin inhibits the release of GABA, resulting in permanent muscle contraction. The first symptom of tetanus is typically stiffness of the jaw. Violent muscle spasms in other parts of the body follow, typically culminating with respiratory failure and death. Because of the severity of tetanus, it is important for nurses to encourage individuals to regularly receive tetanus vaccination boosters throughout their lifetimes.[25]
Stages of Disease
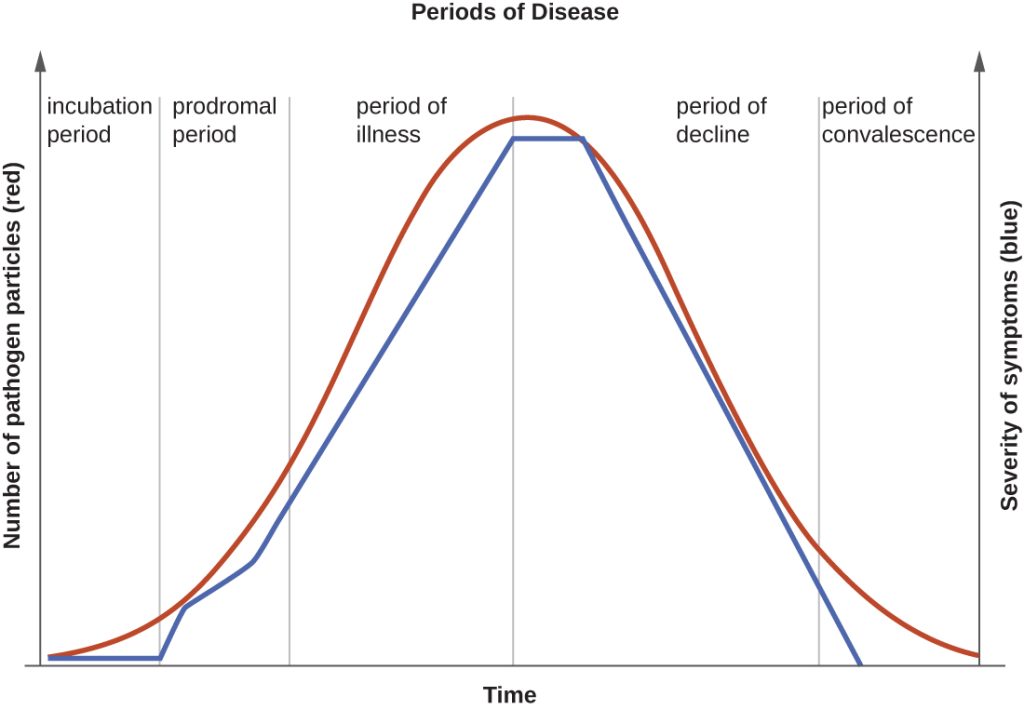
When a pathogen becomes an infection-causing disease, there are five stages of disease, including the incubation, prodromal, illness, decline, and convalescence periods. See Figure 9.13[26] for an illustration of the stages of disease.
Incubation Period
The incubation period occurs after the initial entry of the pathogen into the host when it begins to multiply, but there are insufficient numbers of the pathogen present to cause signs and symptoms of disease. Incubation periods can vary from a day or two in acute disease to months or years in chronic disease, depending upon the pathogen. Factors involved in determining the length of the incubation period are diverse and can include virulence of the pathogen, strength of the host immune defenses, site of infection, and the amount of the pathogen received during exposure. During this incubation period, the client is unaware that a disease is beginning to develop.[27]
Prodromal Period
The prodromal period occurs after the incubation period. During this phase, the pathogen continues to multiply, and the host begins to experience general signs and symptoms of illness caused from activation of the nonspecific innate immunity, such as not feeling well (malaise), low-grade fever, pain, swelling, or inflammation. These signs and symptoms are often too general to indicate a particular disease is occurring.[28]
Acute Phase
Following the prodromal period is the period of acute illness, during which the signs and symptoms of a specific disease become obvious and can become severe. This period of acute illness is followed by the period of decline as the immune system overcomes the pathogen. The number of pathogen particles begins to decline and thus the signs and symptoms of illness begin to decrease. However, during the decline period, clients may become susceptible to developing secondary infections because their immune systems have been weakened by the primary infection.[29]
Convalescent Period
The final period of disease is known as the convalescent period. During this stage, the client generally returns to normal daily functioning, although some diseases may inflict permanent damage that the body cannot fully repair.[30] For example, if a strep infection becomes systemic and causes a secondary infection of the client’s heart valves, the heart valves may never return to full function and heart failure may develop.
Infectious diseases can be contagious during all five of the periods of disease. The transmissibility of an infection during these periods depends upon the pathogen and the mechanisms by which the disease develops and progresses. For example, with many viral diseases associated with rashes (e.g., chicken pox, measles, rubella, roseola), clients are contagious during the incubation period up to a week before the rash develops. In contrast, with many respiratory infections (e.g., colds, influenza, diphtheria, strep throat, and pertussis) the client becomes contagious with the onset of the prodromal period. Depending upon the pathogen, the disease, and the individual infected, transmission can still occur during the periods of decline, convalescence, and even long after signs and symptoms of the disease disappear. For example, an individual recovering from a diarrheal disease may continue to carry and shed the pathogen in feces for a long time, posing a risk of transmission to others through direct or indirect contact.[31]
Types of Infection
Acute vs. Chronic
Acute, self-limiting infections develop rapidly and generally last only 10-14 days. Colds and ear infections are considered acute, self-limiting infections. See Figure 9.14[32] for an image of an individual with an acute, self-limiting infection. Conversely, chronic infections may persist for months. Hepatitis and mononucleosis are examples of chronic infections.[33]

Healthcare-Associated Infections
An infection that is contracted in a health care facility or under medical care is known as a healthcare-associated infection (HAI), formerly referred to as a nosocomial infection. On any given day, about 1 in 31 hospital clients has at least one healthcare-associated infection. HAIs increase the cost of care and delay recovery and are associated with permanent disability, loss of wages, and even death.[34],[35]
The U.S. Department of Health and Human Services (HHS) has established these goals to reduce these common healthcare-associated infections in health care institutions:
- Reduce central line-associated bloodstream infections (CLABSI)
- Reduce catheter-associated urinary tracts infections (CAUTI)
- Reduce the incidence of invasive health care-associated Methicillin-resistant Staphylococcus aureus (MRSA)
- Reduce hospital-onset MRSA bloodstream infections
- Reduce hospital-onset Clostridium difficile infections
- Reduce the rate of Clostridium difficile hospitalizations
- Reduce surgical site infections (SSI)[36],[37]
Blood-borne Pathogens
Blood-borne pathogens are potentially present in a client’s blood and body fluids, placing other clients and health care providers at risk for infection if they are exposed. The most common blood-borne pathogens include hepatitis B, hepatitis C, and human immunodeficiency virus (HIV).
When a nurse or other health care worker experiences exposure due to a needlestick injury or the splashing of body fluids, it should be immediately washed or flushed and then reported so that careful monitoring can occur. When the source of the exposure is known, the health care worker and client are initially tested. Repeat testing and medical prophylaxis may be warranted for the health care worker, depending on the results.[38]
Needlesticks and sharps injuries are the most common causes of blood-borne pathogen exposure for nurses. The National Institute for Occupational Safety and Health (NIOSH) has developed a comprehensive Sharps Injury Prevention Program to decrease needle and sharps injury in health care workers.[39]
Needles are also used in the community, such as at home, work, airports, or public restrooms as individuals use needles to administer prescribed medications or to inject illegal drugs. Nurses can help prevent needlestick and sharps injuries in their community by implementing a community needle disposal program.
Read more about needlestick and sharps injury prevention in the “Aseptic Technique” chapter in Open RN Nursing Skills, 2e.

