Open Resources for Nursing (Open RN)
An infection is the invasion and growth of a microorganism within the body. Infection can lead to disease that causes signs and symptoms, resulting in a deviation from the normal structure or functioning of the host. Infection occurs when nonspecific innate immunity and specific adaptive immunity defenses are inadequate to protect an individual against the invasion of a pathogen. The ability of a microorganism to cause disease is called pathogenicity, and the degree to which a microorganism is likely to become a disease is called virulence. Virulence is a continuum. On one end of the spectrum are organisms that are not harmful, but on the other end are organisms that are highly virulent. Highly virulent pathogens will almost always lead to a disease state when introduced to the body, and some may even cause multi-organ and body system failure in healthy individuals. Less virulent pathogens may cause an initial infection, but may not always cause severe illness. Pathogens with low virulence usually result in mild signs and symptoms of disease, such as a low-grade fever, headache, or muscle aches, and some individuals may even be asymptomatic.[1]
An example of a highly virulent microorganism is Bacillus anthracis, the pathogen responsible for anthrax. The most serious form of anthrax is inhalation anthrax. After Bacillus anthracis spores are inhaled, they germinate. An active infection develops, and the bacteria release potent toxins that cause edema (fluid buildup in tissues), hypoxia (a condition preventing oxygen from reaching tissues), and necrosis (cell death and inflammation). Signs and symptoms of inhalation anthrax include high fever, difficulty breathing, vomiting, coughing up blood, and severe chest pains suggestive of a heart attack. With inhalation anthrax, the toxins and bacteria enter the bloodstream, which can lead to multi-organ failure and death of the client.[2]
Primary Pathogens Versus Opportunistic Pathogens
Pathogens can be classified as either primary pathogens or opportunistic pathogens. A primary pathogen can cause disease in a host regardless of the host’s microbiome or immune system. An opportunistic pathogen, by contrast, can cause disease only in situations that compromise the host’s defenses, such as the body’s protective barriers, immune system, or normal microbiome. Individuals susceptible to opportunistic infections include the very young, the elderly, women who are pregnant, clients undergoing chemotherapy, people with immunodeficiencies (such as acquired immunodeficiency syndrome [AIDS]), clients who are recovering from surgery, and those who have nonintact skin (such as a severe wound or burn).[3]
An example of a primary pathogen is enterohemorrhagic Escherichia coli (E. coli) that produces a toxin that leads to severe and bloody diarrhea, inflammation, and renal failure, even in clients with healthy immune systems. Staphylococcus epidermidis, on the other hand, is an opportunistic pathogen that is a frequent cause of healthcare acquired infection.[4] Staphylococcus epidermidis, often referred to as “staph,” is a member of the normal flora of the skin. However, in hospitals, it can grow in biofilms that form on catheters, implants, or other devices that are inserted into the body during surgical procedures. Once inside the body, it can cause serious infections such as endocarditis.[5]
Other members of normal flora can cause opportunistic infections. Some microorganisms that reside harmlessly in one location of the body can cause disease if they are passed to a different body system. For example, E. coli is normally found in the large intestine, but can cause a urinary tract infection if it enters the bladder.[6]
Normal flora can also cause disease when a shift in the environment of the body leads to overgrowth of a particular microorganism. For example, the yeast Candida is part of the normal flora of the skin, mouth, intestine, and vagina, but its population is kept in check by other organisms of the microbiome. When an individual takes antibiotics, bacteria that would normally inhibit the growth of Candida can be killed off, leading to a sudden growth in the population of Candida. An overgrowth of Candida can manifest as oral thrush (growth of yeast on mouth, throat, and tongue) or a vaginal yeast infection. Other scenarios can also provide opportunities for Candida to cause infection. For example, untreated diabetes can result in a high concentration of glucose in a client’s saliva that provides an optimal environment for the growth of Candida, resulting in oral thrush. Immunodeficiencies, such as those seen in clients with HIV, AIDS, and cancer, can also lead to Candida infections because the body’s immune system is weakened in these conditions and unable to fight off the Candida.[7]
Stages of Pathogenesis
To cause disease, a pathogen must successfully achieve four stages of pathogenesis to become an infection: exposure, adhesion (also called colonization), invasion, and infection. The pathogen must be able to gain entry to the host, travel to the location where it can establish an infection, evade or overcome the host’s immune response, and cause damage (i.e., disease) to the host. In many cases, the cycle is completed when the pathogen exits the host and is transmitted to a new host.[8]
Exposure
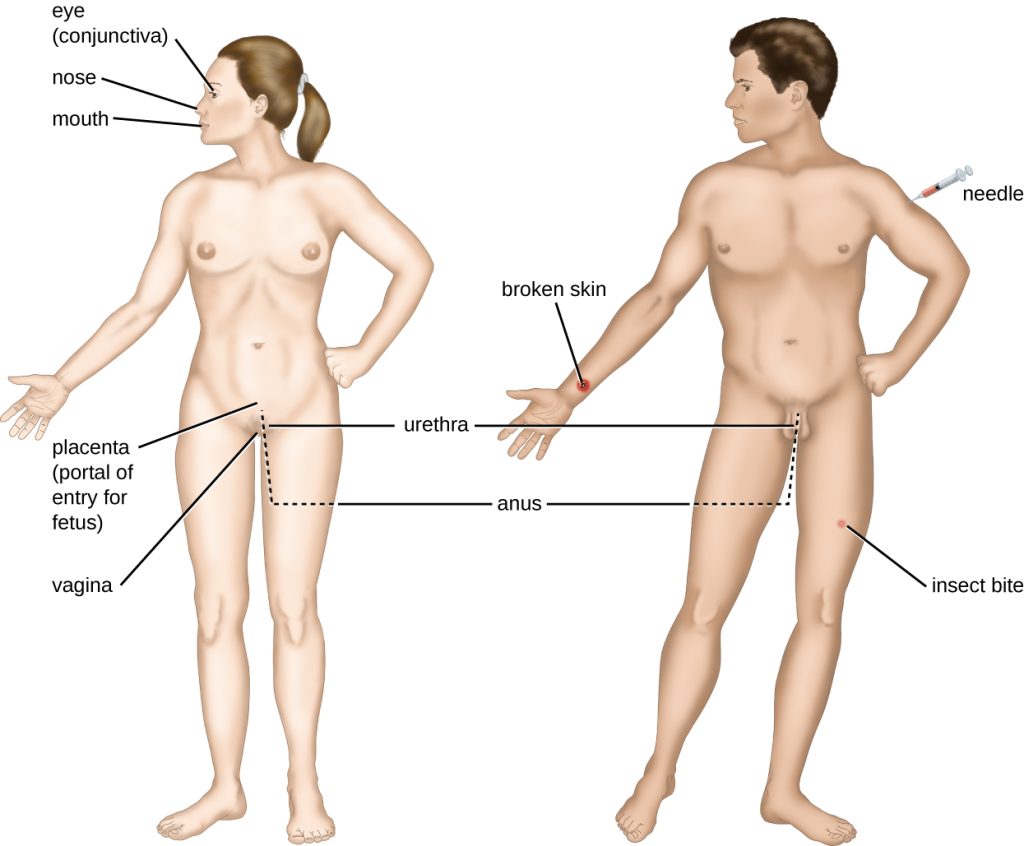
An encounter with a potential pathogen is known as exposure. The food we eat and the objects we touch are all ways that we can come into contact with potential pathogens. Yet, not all contacts result in infection and disease. For a pathogen to cause disease, it needs to be able to gain access into host tissue. An anatomic site through which pathogens can pass into host tissue is called a portal of entry. Portals of entry are locations where the host cells are in direct contact with the external environment, such as the skin, mucous membranes, respiratory, and digestive systems. Portals of entry are illustrated in Figure 9.11.[9],[10]
Adhesion
Following initial exposure, the pathogen adheres at the portal of entry. The term adhesion refers to the capability of pathogenic microbes to attach to the cells of the body, also referred to as colonization.[11]
Invasion
After successful adhesion, the invasion proceeds. Invasion means the spread of a pathogen throughout local tissues or the body. Pathogens may also produce virulence factors that protect them against immune system defenses and determine the degree of tissue damage that occurs. Intracellular pathogens like viruses achieve invasion by entering the host’s cells and reproducing.[12]
Infection
Following invasion, successful multiplication of the pathogen leads to infection. Infections can be described as local, secondary, or systemic, depending on the extent of the infection.[13]
A local infection is confined to a small area of the body, typically near the portal of entry. For example, a hair follicle infected by Staphylococcus aureus infection may result in a boil around the site of infection, but the bacterium is largely contained to this small location. Other examples of local infections that involve more extensive tissue involvement include urinary tract infections confined to the bladder or pneumonia confined to the lungs. Localized infections generally demonstrate signs of inflammation, such as redness, swelling, warmth, pain, and purulent drainage. However, extensive tissue involvement can also cause decreased functioning of the organ affected.[14]
A secondary infection is an infection that occurs during or after treatment for a different infection. It may be caused by the treatment for the first infection or a result of a diminished immune system or the elimination of normal flora. For example, a yeast infection that occurs after a client is treated with antibiotics is a secondary infection.[15]
When an infection becomes disseminated throughout the body, it is called a systemic infection. For example, infection by the varicella-zoster virus typically gains entry through a mucous membrane of the upper respiratory system. It then spreads throughout the body, resulting in a classic red rash associated with chicken pox. Because these lesions are not sites of initial infection, they are signs of a systemic infection. Systemic infections can cause fever, increased heart and respiratory rates, lethargy, malaise, anorexia, and tenderness and enlargement of the lymph nodes.[16]
Sometimes a primary infection can lead to a secondary infection by an opportunistic pathogen. For example, when a client experiences a primary infection from influenza, it can damage and decrease the defense mechanisms of the lungs, making the client more susceptible to a secondary pneumonia by a bacterial pathogen like Haemophilus influenzae. Additionally, treatment of the primary infection may lead to a secondary infection caused by an opportunistic pathogen. For example, antibiotic therapy targeting the primary infection alters the normal flora and creates an opening for opportunistic pathogens like Clostridium difficile or Candida Albicans to cause a secondary infection.[17]
Bacteremia, SIRS, Sepsis, and Septic Shock
When infection occurs, pathogens can enter the bloodstream. The presence of bacteria in blood is called bacteremia. If bacteria are both present and multiplying in the blood, it is called septicemia.[18]
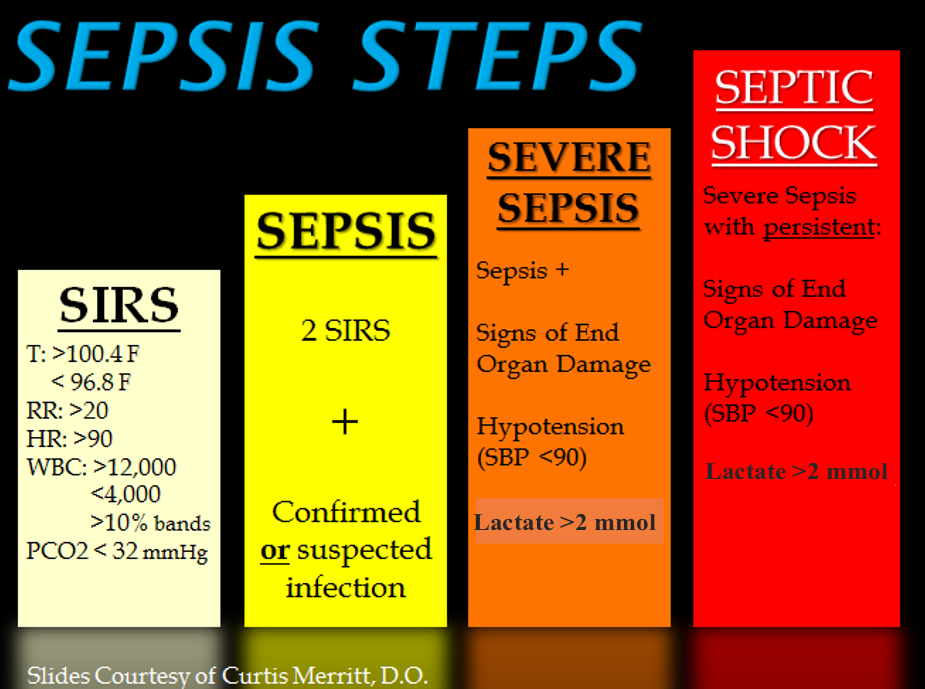
Systemic inflammatory response syndrome (SIRS) is an exaggerated inflammatory response that affects the entire body. It is the body’s reaction to a noxious stressor, including causes such as infection and acute inflammation, but other conditions can trigger it as well. Signs of SIRS are as follows:
- Body temperature over 38 or under 36 degrees Celsius
- Heart rate greater than 90 beats/minute
- Respiratory rate greater than 20 breaths/minute or PaCO2 less than 32 mmHg
- White blood cell count greater than 12,000 or less than 4,000 /microliters or over 10% of immature forms (bands)[19]
Even though the purpose of SIRS is to defend against a noxious stressor, the uncontrolled release of massive amounts of cytokines, called cytokine storm, can lead to organ dysfunction and even death.[20]
Sepsis refers to SIRS that is caused by an infection. Sepsis occurs when an existing infection triggers an exaggerated inflammatory reaction throughout the body. If left untreated, sepsis causes tissue and organ damage. It can quickly spread to multiple organs and is a life-threatening medical emergency.
Sepsis causing damage to one or more organs (such as the kidneys) is called severe sepsis. Severe sepsis can lead to septic shock, a life-threatening decrease in blood pressure (systolic pressure <90 mm Hg) that prevents cells and other organs from receiving enough oxygen and nutrients, causing multi-organ failure and death. See Figure 9.12[21] for an illustration of the progression of sepsis from SIRS to septic shock.
Unfortunately, almost any type of infection in any individual can lead to sepsis. Infections that lead to sepsis most often start in the lungs, urinary tract, gastrointestinal tract, or skin. Some people are especially at risk for developing sepsis, such as adults over age 65; children younger than one year old; people who are immunocompromised or have chronic medical conditions, such as diabetes, lung disease, cancer, and kidney disease; and survivors of a previous sepsis episode.[22]
In addition to exhibiting signs of SIRS, clients with sepsis may also have additional signs such as elevated fever and shivering, confusion, shortness of breath, pain or discomfort, and clammy or sweaty skin. Diligent nursing care is vital for recognizing early signs of SIRS and sepsis and promptly notifying the health care provider and/or following sepsis protocols in place at your health care facility.[23]
Use the following to read more information about sepsis:
- Read more information about sepsis at the CDC’s Sepsis web page.
- Read the CDC infographic on Protect Your Patients From Sepsis.
- Read an article about caring for clients with sepsis titled Something Isn’t Right: The Subtle Changes of Early Deterioration.
- Read more about the Surviving Sepsis Campaign with early recognition and treatment of sepsis using the Hour-1 Bundle.
Toxins
Some pathogens release toxins that are biological poisons that assist in their ability to invade and cause damage to tissues. For example, Botulinum toxin is a neurotoxin produced by the gram-positive bacterium Clostridium botulinum that is an acutely toxic substance because it blocks the release of the neurotransmitter acetylcholine. The toxin’s blockage of acetylcholine results in muscle paralysis with the potential to stop breathing due to its effect on the respiratory muscles. This condition is referred to as botulism, a type of food poisoning that can be caused by improper sterilization of canned foods. However, because of its paralytic action, low concentrations of Botox are also used for beneficial purposes such as cosmetic procedures to remove wrinkles and in the medical treatment of overactive bladder.[24]
Another type of neurotoxin is tetanus toxin, which is produced by the gram-positive bacterium Clostridium tetani. Tetanus toxin inhibits the release of GABA, resulting in permanent muscle contraction. The first symptom of tetanus is typically stiffness of the jaw. Violent muscle spasms in other parts of the body follow, typically culminating with respiratory failure and death. Because of the severity of tetanus, it is important for nurses to encourage individuals to regularly receive tetanus vaccination boosters throughout their lifetimes.[25]
Stages of Disease
When a pathogen becomes an infection-causing disease, there are five stages of disease, including the incubation, prodromal, illness, decline, and convalescence periods. See Figure 9.13[26] for an illustration of the stages of disease.
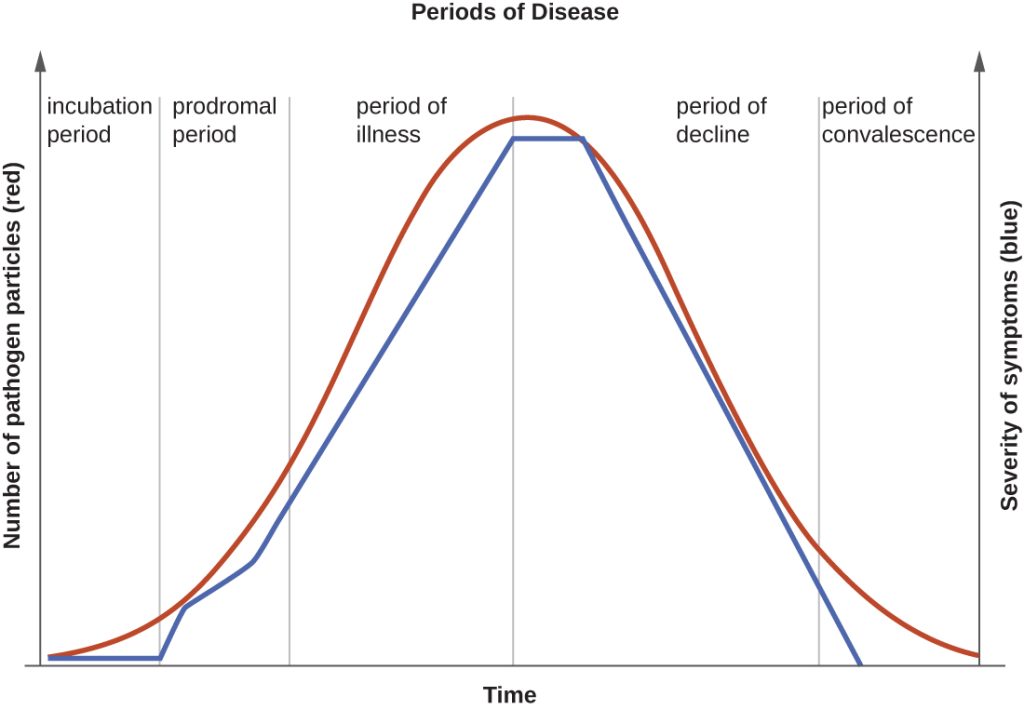
Incubation Period
The incubation period occurs after the initial entry of the pathogen into the host when it begins to multiply, but there are insufficient numbers of the pathogen present to cause signs and symptoms of disease. Incubation periods can vary from a day or two in acute disease to months or years in chronic disease, depending upon the pathogen. Factors involved in determining the length of the incubation period are diverse and can include virulence of the pathogen, strength of the host immune defenses, site of infection, and the amount of the pathogen received during exposure. During this incubation period, the client is unaware that a disease is beginning to develop.[27]
Prodromal Period
The prodromal period occurs after the incubation period. During this phase, the pathogen continues to multiply, and the host begins to experience general signs and symptoms of illness caused from activation of the nonspecific innate immunity, such as not feeling well (malaise), low-grade fever, pain, swelling, or inflammation. These signs and symptoms are often too general to indicate a particular disease is occurring.[28]
Acute Phase
Following the prodromal period is the period of acute illness, during which the signs and symptoms of a specific disease become obvious and can become severe. This period of acute illness is followed by the period of decline as the immune system overcomes the pathogen. The number of pathogen particles begins to decline and thus the signs and symptoms of illness begin to decrease. However, during the decline period, clients may become susceptible to developing secondary infections because their immune systems have been weakened by the primary infection.[29]
Convalescent Period
The final period of disease is known as the convalescent period. During this stage, the client generally returns to normal daily functioning, although some diseases may inflict permanent damage that the body cannot fully repair.[30] For example, if a strep infection becomes systemic and causes a secondary infection of the client’s heart valves, the heart valves may never return to full function and heart failure may develop.
Infectious diseases can be contagious during all five of the periods of disease. The transmissibility of an infection during these periods depends upon the pathogen and the mechanisms by which the disease develops and progresses. For example, with many viral diseases associated with rashes (e.g., chicken pox, measles, rubella, roseola), clients are contagious during the incubation period up to a week before the rash develops. In contrast, with many respiratory infections (e.g., colds, influenza, diphtheria, strep throat, and pertussis) the client becomes contagious with the onset of the prodromal period. Depending upon the pathogen, the disease, and the individual infected, transmission can still occur during the periods of decline, convalescence, and even long after signs and symptoms of the disease disappear. For example, an individual recovering from a diarrheal disease may continue to carry and shed the pathogen in feces for a long time, posing a risk of transmission to others through direct or indirect contact.[31]
Types of Infection
Acute vs. Chronic
Acute, self-limiting infections develop rapidly and generally last only 10-14 days. Colds and ear infections are considered acute, self-limiting infections. See Figure 9.14[32] for an image of an individual with an acute, self-limiting infection. Conversely, chronic infections may persist for months. Hepatitis and mononucleosis are examples of chronic infections.[33]

Healthcare-Associated Infections
An infection that is contracted in a health care facility or under medical care is known as a healthcare-associated infection (HAI), formerly referred to as a nosocomial infection. On any given day, about 1 in 31 hospital clients has at least one healthcare-associated infection. HAIs increase the cost of care and delay recovery and are associated with permanent disability, loss of wages, and even death.[34],[35]
The U.S. Department of Health and Human Services (HHS) has established these goals to reduce these common healthcare-associated infections in health care institutions:
- Reduce central line-associated bloodstream infections (CLABSI)
- Reduce catheter-associated urinary tracts infections (CAUTI)
- Reduce the incidence of invasive health care-associated Methicillin-resistant Staphylococcus aureus (MRSA)
- Reduce hospital-onset MRSA bloodstream infections
- Reduce hospital-onset Clostridium difficile infections
- Reduce the rate of Clostridium difficile hospitalizations
- Reduce surgical site infections (SSI)[36],[37]
Blood-borne Pathogens
Blood-borne pathogens are potentially present in a client’s blood and body fluids, placing other clients and health care providers at risk for infection if they are exposed. The most common blood-borne pathogens include hepatitis B, hepatitis C, and human immunodeficiency virus (HIV).
When a nurse or other health care worker experiences exposure due to a needlestick injury or the splashing of body fluids, it should be immediately washed or flushed and then reported so that careful monitoring can occur. When the source of the exposure is known, the health care worker and client are initially tested. Repeat testing and medical prophylaxis may be warranted for the health care worker, depending on the results.[38]
Needlesticks and sharps injuries are the most common causes of blood-borne pathogen exposure for nurses. The National Institute for Occupational Safety and Health (NIOSH) has developed a comprehensive Sharps Injury Prevention Program to decrease needle and sharps injury in health care workers.[39]
Needles are also used in the community, such as at home, work, airports, or public restrooms as individuals use needles to administer prescribed medications or to inject illegal drugs. Nurses can help prevent needlestick and sharps injuries in their community by implementing a community needle disposal program.
Read more about needlestick and sharps injury prevention in the “Aseptic Technique” chapter in Open RN Nursing Skills, 2e.
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- Butcher, H., Bulechek, G., Dochterman, J., & Wagner, C. (2018). Nursing interventions classification (NIC). Elsevier. pp. 214, 226-227, 346. ↵
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- “OSC_Microbio_15_02_Portal.jpg” by OpenStax is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction. ↵
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- Medline Plus. (2024). Secondary infections. https://medlineplus.gov/ency/article/002300.htm ↵
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- Mouton, C. P., Bazaldua, O., Pierce, B., & Espino, D. V. (2001). Common infections in older adults. American Family Physician, 63(2), 257-269. https://www.aafp.org/afp/2001/0115/p257.html ↵
- Mouton, C. P., Bazaldua, O., Pierce, B., & Espino, D. V. (2001). Common infections in older adults. American Family Physician, 63(2), 257-269. https://www.aafp.org/afp/2001/0115/p257.html ↵
- This work is derivative of “Sepsis_Steps.png” by Hadroncastle and is licensed under CC BY-SA 4.0 ↵
- Centers for Disease Control and Prevention. (2020, August 18). Sepsis. https://www.cdc.gov/sepsis/index.html ↵
- Centers for Disease Control and Prevention. (2020, August 18). Sepsis. https://www.cdc.gov/sepsis/index.html ↵
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- “unknown image” by OpenStax is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/15-1-characteristics-of-infectious-disease ↵
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- “392131387-huge.jpg” by Alexandr Litovchenko is used under license from Shutterstock.com ↵
- This work is a derivative of Microbiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/microbiology/pages/1-introduction ↵
- Centers for Disease Control and Prevention. (2016, March 4). Healthcare-associated infections. https://www.cdc.gov/hai/index.html ↵
- U.S. Department of Health and Human Services. (2020, January 15). Healthcare-associated infections. https://health.gov/our-work/health-care-quality/health-care-associated-infections ↵
- Centers for Disease Control and Prevention. (2016, March 4). Healthcare-associated infections. https://www.cdc.gov/hai/index.html ↵
- U.S. Department of Health and Human Services. (2020, January 15). Healthcare-associated infections. https://health.gov/our-work/health-care-quality/health-care-associated-infections ↵
- Centers for Disease Control and Prevention. (2014). Bloodborne pathogen exposure. https://www.cdc.gov/niosh/docs/2007-157/default.html ↵
- Centers for Disease Control and Prevention. (2014). How to prevent needlestick and sharps injuries. https://www.cdc.gov/niosh/docs/2012-123/ ↵
The invasion and growth of a microorganism within the body.
Signs and symptoms resulting in a deviation from the normal structure or functioning of the host.
The ability of a microorganism to cause disease.
The degree to which a microorganism is likely to become a disease.
A pathogen that can cause disease in a host regardless of the host’s resident microbiota or immune system.
A pathogen that only causes disease in situations that compromise the host’s defenses, such as the body’s protective barriers, immune system, or normal microbiota.
An encounter with a potential pathogen.
An anatomic site through which pathogens can pass into a host, such as mucous membranes, skin, respiratory, or digestive systems.
Capability of pathogenic microbes to attach to the cells of the body.
Means the spread of a pathogen throughout local tissues or the body.
Infection confined to a small area of the body, typically near the portal of entry, and usually presents with signs of redness, warmth, swelling, warmth, and pain.
A localized pathogen that spreads to a secondary location.
An infection that becomes disseminated throughout the body.
The presence of bacteria in blood.
Bacteria that are both present and multiplying in the blood.
An exaggerated inflammatory response to a noxious stressor (including, but not limited to, infection and acute inflammation) that affects the entire body.
An existing infection that triggers an exaggerated inflammatory reaction called SIRS throughout the body.
Severe sepsis that leads to a life-threatening decrease in blood pressure (systolic pressure <90 mm Hg), preventing cells and other organs from receiving enough oxygen and nutrients. It can cause multi organ failure and death.
The period of a disease after the initial entry of the pathogen into the host but before symptoms develop.
The disease stage after the incubation period when the pathogen continues to multiply and the host begins to experience general signs and symptoms of illness that result from activation of the immune system, such as fever, pain, soreness, swelling, or inflammation.
Drainage from a wound that is clear, thin, watery plasma. It’s normal during the inflammatory stage of wound healing, and small amounts are considered normal wound drainage.
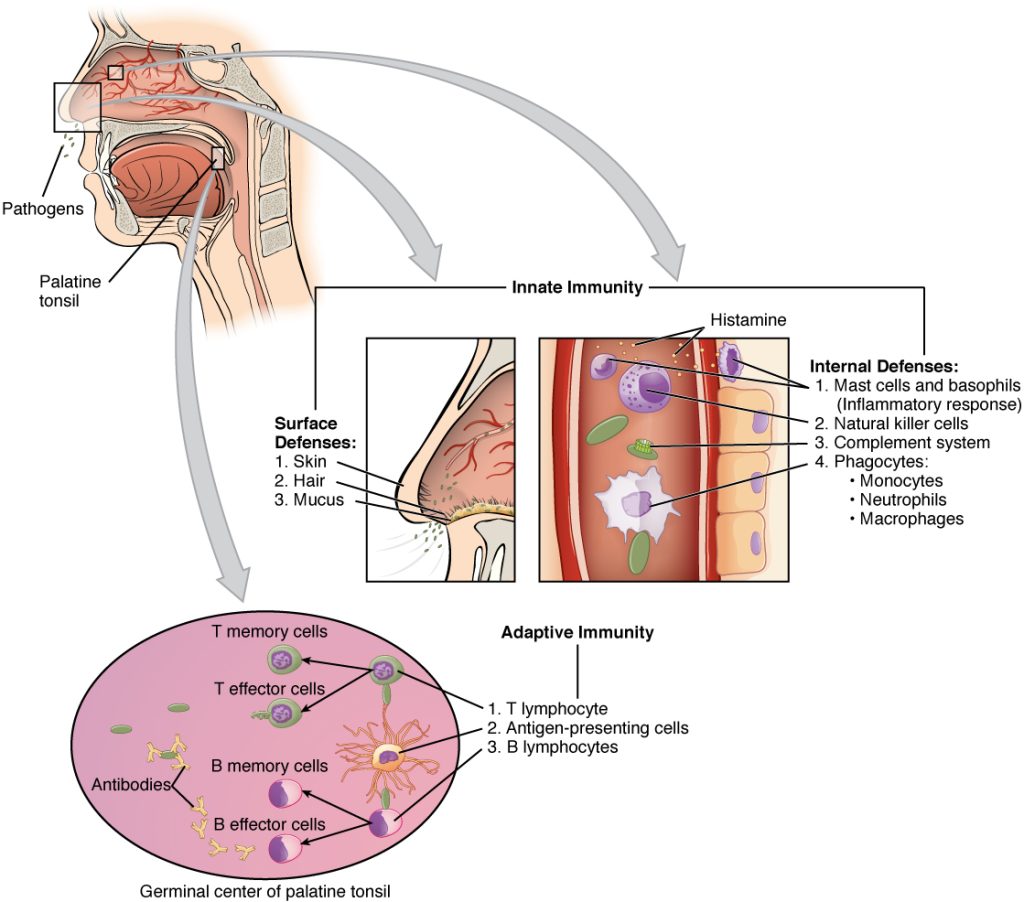
There are two basic ways the body defends against pathogens: nonspecific innate immunity and specific adaptive immunity.
Nonspecific Innate Immunity
Nonspecific innate immunity is a system of defenses in the body that targets invading pathogens in a nonspecific manner. It is called “innate” because it is present from the moment we are born. Nonspecific innate immunity includes physical defenses, chemical defenses, and cellular defenses.[1]
Physical Defenses
Physical defenses are the body’s most basic form of defense against infection. They include physical barriers to microbes, such as skin and mucous membranes, as well as mechanical defenses that physically remove microbes and debris from areas of the body where they might cause harm or infection. In addition, a person’s microbiome provides physical protection against disease as normal flora compete with pathogens for nutrients and cellular-binding sites.[2]
Skin
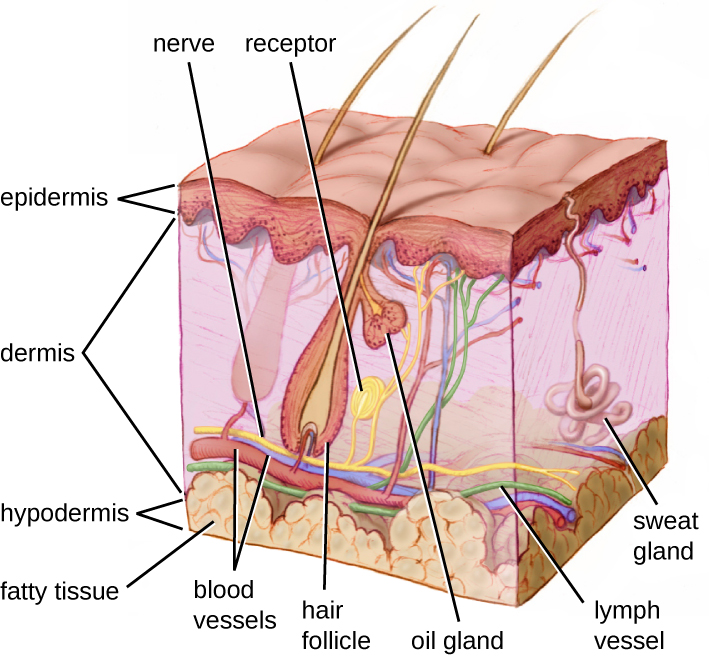
One of the body’s most important physical barriers is the skin barrier, which is composed of three layers of closely packed cells. See Figure 9.5[3] for an illustration of the layers of skin. The topmost layer of skin called the epidermis consists of cells that are packed with keratin. Keratin makes the skin’s surface mechanically tough and resistant to degradation by bacteria. Infections can occur when the skin barrier is broken, allowing the entry of opportunistic pathogens that infect the skin tissue surrounding the wound and possibly spread to deeper tissues.[4]
Mucus Membranes
The mucous membranes lining the nose, mouth, lungs, and urinary and digestive tracts provide another nonspecific barrier against potential pathogens. Mucous membranes consist of a layer of epithelial cells bound by tight junctions. The epithelial cells secrete a moist, sticky substance called mucous. Mucous covers and protects the fragile cell layers beneath it and also traps debris, including microbes. Mucus secretions also contain antimicrobial peptides.[5]
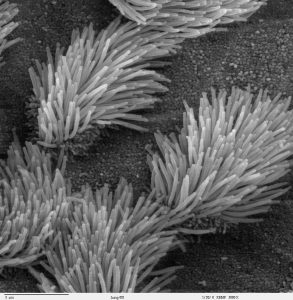
In many regions of the body, mechanical actions flush mucus (along with trapped or dead microbes) out of the body or away from potential sites of infection. For example, in the respiratory system, inhalation can bring microbes, dust, mold spores, and other small airborne debris into the body. This debris becomes trapped in the mucus lining the respiratory tract. The epithelial cells lining the upper parts of the respiratory tract have hair-like appendages known as cilia. Movement of the cilia propels debris-laden mucus out and away from the lungs. The expelled mucus is then swallowed and destroyed in the stomach, coughed up, or sneezed out. This system of removal is often called the mucociliary escalator. Disruption of the mucociliary escalator by the damaging effects of smoking can lead to increased colonization of bacteria in the lower respiratory tract and frequent infections, which highlights the importance of this physical barrier to host defenses.[6] See Figure 9.6[7] for an image of a magnified mucociliary escalator.
Like the respiratory tract, the digestive tract is a portal of entry through which microbes enter the body, and the mucous membranes lining the digestive tract provide a nonspecific physical barrier against ingested microbes. The intestinal tract is lined with epithelial cells, interspersed with mucus-secreting goblet cells. This mucus mixes with material received from the stomach, trapping foodborne microbes and debris, and is moved forward through the digestive tract via the mechanical action of peristalsis. Peristalsis refers to involuntary contraction and relaxation of the muscles of the intestine, creating wave-like movements that push digested content forward in the digestive tract.[8] For this reason, feces can contain microorganisms that can cause the spread of infection, making it essential to perform good hand hygiene to prevent transmission of disease through the fecal-oral route.
Endothelia
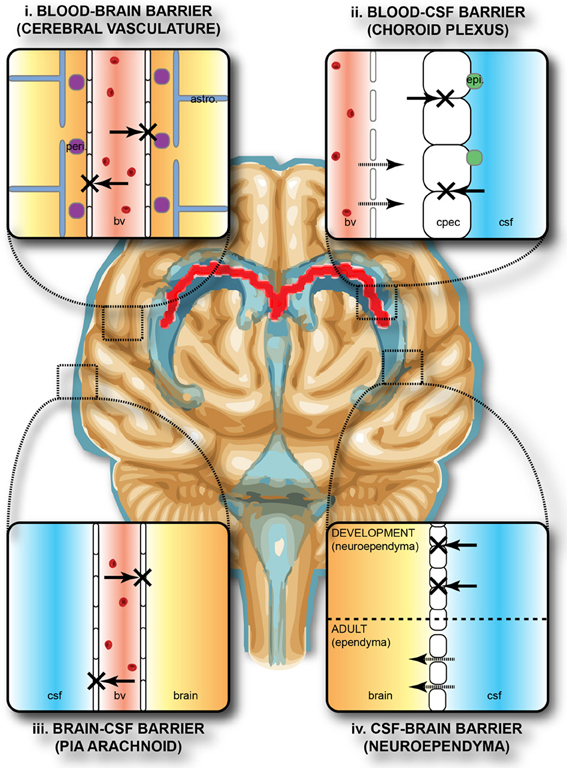
The epithelial cells lining the urogenital tract, blood vessels, lymphatic vessels, and other tissues are known as endothelia. These tightly packed cells provide an effective frontline barrier against invaders. The endothelia of the blood-brain barrier, for example, protects the central nervous system (CNS) from microorganisms. Infection of the CNS can quickly lead to serious and often fatal inflammation. The protection of the blood-brain barrier keeps the cerebrospinal fluid that surrounds the brain and spinal cord sterile.[9] See Figure 9.7[10] for an illustration of the blood-brain barrier.
Mechanical Defenses
In addition to physical barriers that keep microbes out, the body has several mechanical defenses that physically remove pathogens from the body and prevent them from taking up residence. For example, the flushing action of urine and tears serves to carry microbes away from the body. The flushing action of urine is responsible for the normally sterile environment of the urinary tract. The eyes have additional physical barriers and mechanical mechanisms for preventing infections. The eyelashes and eyelids prevent dust and airborne microorganisms from reaching the surface of the eye. Any microbes or debris that make it past these physical barriers is flushed out by the mechanical action of blinking, which bathes the eye in tears, washing debris away.[11] See Figure 9.8[12] for an image of an infant’s eyelashes that prevent dust from reaching the surface of the eye.

Microbiome
Normal flora that contributes to an individual’s microbiome serve as an important first-line defense against invading pathogens. Through their occupation of cellular binding sites and competition for available nutrients, normal flora prevents the early steps of pathogen attachment and proliferation required for the establishment of an infection. For example, in the vagina, normal flora competes with opportunistic pathogens like Candida albicans. This competition prevents yeast infection by limiting the availability of nutrients and inhibiting the growth of Candida, keeping its population in check. Similar competitions occur between normal flora and potential pathogens on the skin, in the upper respiratory tract, and in the gastrointestinal tract.[13]
The importance of the normal flora in host defenses is highlighted by a person’s increased susceptibility to infectious diseases when their microbiome is disrupted or eliminated. For example, treatment with antibiotics can significantly deplete the normal flora of the gastrointestinal tract, providing an advantage for pathogenic bacteria such as Clostridium difficile (C-diff) to colonize and cause diarrheal infection. Diarrhea caused by C-diff can be severe and potentially lethal. In fact, a recent strategy for treating recurrent C-diff infections is fecal transplantation that involves the transfer of fecal material from a donor into the intestines of the client as a method of restoring their normal flora.[14]
Chemical Defenses
In addition to physical defenses, our nonspecific innate immune system uses several chemical mediators that inhibit microbial invaders. The term chemical mediators encompass a wide array of substances found in various fluids and tissues throughout the body. For example, sebaceous glands in the dermis secrete an oil called sebum that is released onto the skin surface through hair follicles. Sebum provides an additional layer of defense by helping seal off the pore of the hair follicle and preventing bacteria on the skin’s surface from invading sweat glands and surrounding tissue. Environmental factors can affect these chemical defenses of the skin. For example, low humidity in the winter makes the skin drier and more susceptible to pathogens normally inhibited by the skin’s low pH. Application of skin moisturizer restores moisture and essential oils to the skin and helps prevent dry skin from becoming infected.[15]
Examples of other chemical defenses are enzymes, pH level, and chemical mediators. Enzymes in saliva and the digestive tract eliminate most pathogens that manage to survive the acidic environment of the stomach. In the urinary tract, the slight acidity of urine inhibits the growth of potential pathogens in the urinary tract. The respiratory tract also uses various chemical mediators in the nasal passages, trachea, and lungs that have antibacterial properties.[16]
Plasma Protein Mediators
In addition to physical, mechanical, and chemical defenses, there are also nonspecific innate immune factors in plasma, the fluid portion of blood, such as acute-phase proteins, complement proteins, and cytokines. These plasma protein mediators contribute to the inflammatory response.[17]
An example of an acute-phase protein is C-reactive protein. High levels of C-reactive protein indicate inflammation caused by a serious infection or other medical condition.[18]
Complement proteins are always present in the blood and tissue fluids, allowing them to be activated quickly. They aid in the destruction of pathogens by piercing their outer membranes (cell lysis) or by making them more attractive to phagocytic cells such as macrophages.[19]
Cytokines are proteins that affect interaction and communication between cells. When a pathogen enters the body, the first immune cell to notice the pathogen is like the conductor of an orchestra. That cell directs all the other immune cells by creating and sending out messages (cytokines) to the rest of the organs or cells in the body to respond to and initiate inflammation. Too many cytokines can have a negative effect and result in what's known as a cytokine storm.[20],[21] A cytokine storm is a severe immune reaction in which the body releases too many cytokines into the blood too quickly. A cytokine storm can occur as a result of an infection, autoimmune condition, or other disease. Signs and symptoms include high fever, inflammation, severe fatigue, and nausea. A cytokine storm can be severe or life-threatening and lead to multiple organ failure. For example, many COVID-19 complications and deaths were caused by a cytokine storm.[22],[23]
Inflammation
Inflammation is a response triggered by a cascade of chemical mediators and occurs when pathogens successfully breach the nonspecific innate immune system or when an injury occurs. Although inflammation is often perceived as a negative consequence of injury or disease, it is a necessary process that recruits cellular defenses needed to eliminate pathogens, remove damaged and dead cells, and initiate repair mechanisms. Excessive inflammation, however, can result in local tissue damage, and in severe cases, such as sepsis, it can become deadly.[24]
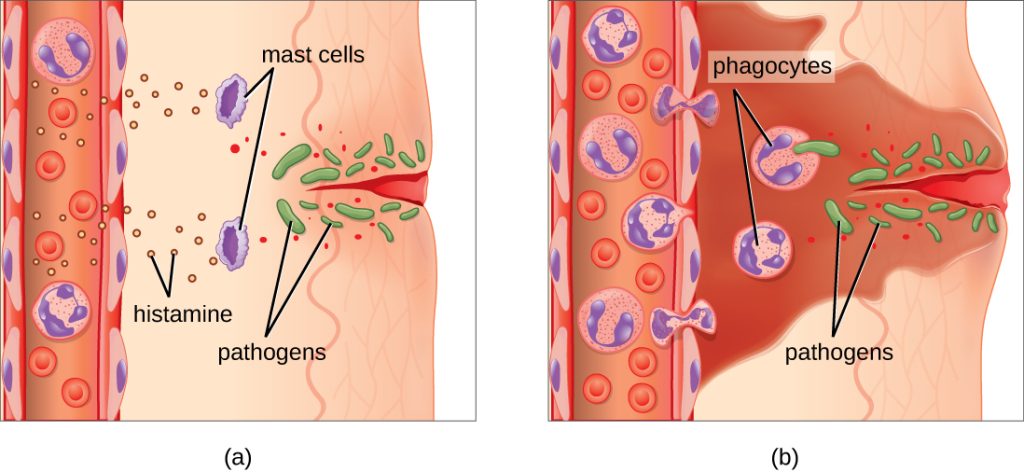
An immediate response to tissue injury is acute inflammation. Vasoconstriction occurs to minimize blood loss if injury has occurred. Vasoconstriction is followed by vasodilation with increased permeability of the blood vessels due to the release of histamine by mast cells. Histamine contributes to the five observable signs of the inflammatory response: erythema (redness), edema (swelling), heat, pain, and altered function. It is also associated with an influx of phagocytes at the site of injury and/or infection. See Figure 9.9[25] for an illustration of the inflammatory response, with (a) demonstrating when mast cells detect injury to nearby cells and release histamine, initiating an inflammatory response and (b) illustrating where histamine increases blood flow to the wound site and the associated increased vascular permeability allows fluid, proteins, phagocytes, and other immune cells to enter infected tissue. These events result in the swelling and reddening of the injured site. The increased blood flow to the injured site causes it to feel warm. Inflammation is also associated with pain due to these events stimulating nerve pain receptors in the tissue. Increasing numbers of neutrophils are then recruited to the area to fight pathogens. As the fight rages on, white blood cells are recruited to the area, and pus forms from the accumulation of neutrophils, dead cells, tissue fluids, and lymph. Typically, after a few days, macrophages clear out this pus.[26] During injury, if this nonspecific inflammatory process does not successfully kill the pathogens, infection occurs.
Fever
A fever is part of the inflammatory response that extends beyond the site of infection and affects the entire body, resulting in an overall increase in body temperature. Like other forms of inflammation, a fever enhances the nonspecific innate immune defenses by stimulating white blood cells to kill pathogens. The rise in body temperature also inhibits the growth of many pathogens. During fever, the client’s skin may appear pale due to vasoconstriction of the blood vessels in the skin to divert blood flow away from extremities, minimize the loss of heat, and raise the body’s core temperature. The hypothalamus also stimulates the shivering of muscles to generate heat and raise the core temperature.[27]
A low-level fever is thought to help an individual overcome an illness. However, in some instances, this immune response can be too strong, causing tissue and organ damage and, in severe cases, even death. For example, Staphylococcus aureus and Streptococcus pyogenes are capable of producing superantigens that cause toxic shock syndrome and scarlet fever, respectively. Both of these conditions are associated with extremely high fevers in excess of 42 °C (108 °F) that must be managed to prevent tissue injury and death.[28]
When a fever breaks, the hypothalamus stimulates vasodilation, resulting in a return of blood flow to the skin and a subsequent release of heat from the body. The hypothalamus also stimulates sweating, which cools the skin as the sweat evaporates.[29]
Specific Adaptive Immunity
Now that we have discussed several nonspecific innate defenses against a pathogen, let’s discuss specific adaptive immunity. Specific adaptive immunity is the immune response that is activated when the nonspecific innate immune response is insufficient to control an infection. There are two types of adaptive responses: the cell-mediated immune response, which is carried out by T cells, and the humoral immune response, which is controlled by activated B cells and antibodies.[30]
B cells mature in the bone marrow. B cells make Y-shaped proteins called antibodies that are specific to each pathogen and lock onto its surface and mark it for destruction by other immune cells. The five classes of antibodies are IgG, IgM, IgA, IgD, and IgE. They also turn into memory B cells. Memory B cells are stored and released in the event a specific antigen reappears in the future. This allows the immune system to mount a quick defense because of the previously created memory B cells.[31]
T cells mature in the thymus. T cells are categorized into three classes: helper T cells, regulatory T cells, and cytotoxic T cells. Helper T cells stimulate B cells to make antibodies and help killer cells develop. Killer T cells directly kill cells that have already been infected by a pathogen. T cells also use cytokines as messenger molecules to send chemical instructions to the rest of the immune system to ramp up its response.[32]
Specific adaptive immunity also creates memory cells for each specific pathogen that provides the host with long-term protection from reinfection with that pathogen. On reexposure, these memory cells facilitate an efficient and quick immune response. For example, when an individual recovers from chicken pox, the body develops a memory of the varicella-zoster virus that will specifically protect it from reinfection if it is exposed to the virus again. Vaccines are administered with the purpose of enhancing a person's specific adaptive immunity.[33]
See Figure 9.10[34] for an illustration of innate immunity and specific adaptive immunity that occur in response to a pathogen entering the body through the nose.