Open Resources for Nursing (Open RN)
The American Nurses Association (ANA) is a professional organization that represents the interests of the nation’s four million registered nurses and is at the forefront of improving the quality of health care for all.[1] The ANA establishes ethical and professional standards for nurses that also guide safe administration of medications. These code of ethics and professional standards are described in ANA publications titled Code of Ethics for Nurses and Nursing: Scope and Standards of Practice.
Code of Ethics for Nurses
The ANA developed the Code of Ethics for Nurses as a guide for carrying out nursing responsibilities in a manner consistent with quality in nursing care and the ethical obligations of the profession.[2] Several provisions from the Code of Ethics impact how nurses should administer medication in an ethical manner. A summary of each provision from the Code of Ethics and how it pertains to medication administration is outlined below:
- Provision 1 focuses on respect for human dignity and the right for self-determination: “The nurse practices with compassion and respect for the inherent dignity, worth, and unique attributes of every person.”
- Provision 2 states, “The nurse’s primary commitment is to the client…”[3] In health care settings, nurses often experience several competing loyalties, such as to their employer, to the doctor(s), to their supervisor, or to others on the health care team. However, the client should always receive the primary commitment of the nurse. Additionally, the client has the right to accept, refuse, or terminate any treatment, including medications.
- Provision 3 states, “The nurse promotes, advocates for, and protects the rights, health, and safety of the patient…”[4] This provision includes a nurse’s responsibility to promote a culture of safety for clients. If errors occur, they must be reported, and nurses should ensure responsible disclosure of errors to clients. This also includes proper disclosure of questionable practices, such as drug diversion or impaired practice by any professional.
- Provision 4 involves authority, accountability, and responsibility by a nurse to follow legal requirements, such as state practice acts and professional standards of care.
- Provision 5 includes the responsibility of the nurse to promote health and safety.
- Provision 6 focuses on virtues that make a nurse a morally good person. For example, nurses are held accountable to use their clinical judgment to avoid causing harm to clients (maleficence) and to do good (beneficence). When administering medications, nurses should validate the medication is doing more “good” than “harm” (adverse or side effects).
- Provision 7 focuses on a nurse practicing within the professional standards set forth by their state nurse practice act, as well as standards established by professional nursing organizations.
- Provision 8 explains that a nurse must address the social determinants of health, such as poverty, education, safe medication, and health care disparities.[5]
Whenever a nurse provides client care, the ANA’s Code of Ethics should be used as a guide for professional ethical behavior.
View the ANA’s Code of Ethics for Nurses.
Critical Thinking Activity 2.2a
A nurse is preparing to administer medications to a client. While reviewing the chart, the nurse notices two medications with similar mechanisms of action have been prescribed by two different providers.
What is the nurse’s best response?
Note: Answers to the Critical Thinking activities can be found in the “Answer Key” sections at the end of the book.
Standards and Scope of Practice
The ANA publishes Nursing: Scope and Standards of Practice. This resource establishes national standards for nurses and is updated regularly.[6]
The ANA defines the scope of nursing as “the protection, promotion, and optimization of health and abilities, prevention of illness and injury, facilitation of healing, alleviation of suffering through the diagnosis and treatment of human response, and advocacy in the care of individuals, families, groups, communities, and populations.” A registered nurse (RN) is defined as an individual who is educationally prepared and licensed by a state to practice as a registered nurse. Nursing practice is characterized by the following tenets[7]:
- Caring and health are central to the practice of the registered nurse.
- Nursing practice is individualized to the unique needs of the health care consumer.
- Registered nurses use the nursing process to plan and provide individualized care for health care consumers.
- Nurses coordinate care by establishing partnerships to reach a shared goal of delivering safe, quality health care.
The ANA establishes Standards of Practice and Standards of Professional Performance in the Nursing: Scope and Standards of Practice publication. State nurse practice acts further define the scope of practice of RNs and Licensed Practical Nurses/Vocational Nurses (LPNs/VNs) within each state. Nurse practice acts are further discussed in the “Legal Foundations and National Guidelines for Safe Medication Administration” section of this chapter.
The ANA’s Nursing: Scope and Standards of Practice publication can be purchased on the nursingworld.org website or borrowed from many libraries.
Standards of Practice
The ANA’s Standards of Practice are authoritative statements of duties that all registered nurses, regardless of role, population, or specialty, are expected to perform competently. Standards of Practice include assessment, diagnosis, outcome identification, planning, implementation, and evaluation (ADOPIE) components of providing client care, also known as the “nursing process.” When nurses safely administer medication, all components of ADOPIE are addressed.
Assessment
The “Assessment” Standard of Practice is defined as, “The registered nurse collects pertinent data and information relative to the health care consumer’s health or the situation.”[8] A registered nurse uses a systematic method to collect and analyze client data. Assessment includes physiological data, as well as psychological, sociocultural, spiritual, economic, and lifestyle data. For example, when a nurse assesses multiple pieces of data for a hospitalized client with pain, this is considered part of a comprehensive pain assessment.
Diagnosis
The “Diagnosis” Standard of Practice is defined as, “The registered nurse analyzes the assessment data to determine actual or potential diagnoses, problems, and issues.”[9] A nursing diagnosis is the nurse’s clinical judgment about the client’s response to actual or potential health conditions or needs. Nursing diagnoses are used to create the nursing care plan and are different than medical diagnoses.[10]
Outcomes Identification
The “Outcomes Identification” Standard of Practice is defined as, “The registered nurse identifies expected outcomes for a plan individualized to the health care consumer or the situation.”[11] The nurse sets measurable and achievable short- and long-term goals and specific outcomes in collaboration with the client based on their assessment data and nursing diagnoses.
Planning
The “Planning” Standard of Practice is defined as, “The registered nurse develops a collaborative plan encompassing strategies to achieve expected outcomes.”[12] Assessment data, diagnoses, and goals are used to select evidence-based nursing interventions customized to each client’s needs and concerns. Goals, expected outcomes, and nursing interventions are documented in the client’s nursing care plan so that nurses, as well as other health professionals, have access to it for continuity of care.[13]
Implementation
The “Implementation” Standard of Practice is defined as, “The nurse implements the identified plan.”[14] Nursing interventions are implemented or delegated to licensed practical nurses/vocational nurses (LPNs/VNs) or unlicensed assistive personnel (UAP) with supervision. Interventions are also documented in the client’s electronic medical record as they are completed.[15]
The “Implementation” Standard of Professional Practice also includes the subcategories “Coordination of Care” and “Health Teaching and Health Promotion” to promote health and a safe environment.[16]
Coordination of Care
The ANA standard for coordination of care states, “The registered nurse coordinates care delivery.”[17] When ensuring medications are administered safely, the nurse collaborates with the client and the interprofessional health care team to meet mutually agreed upon outcomes. The nurse also engages the client in self-care to achieve their preferred goals for quality of life. For example, one client with chronic pain may have a pain management goal of “5” with their quality of life preference of having the ability to participate in social activities with friends but not experiencing burdensome side effect of medication. Another client with chronic pain may have a pain management goal of “0” with a quality of life preference of having no pain no matter what the side effects. The nurse advocates for these clients’ goals and preferences with the interprofessional team.
Nurses also serve vital roles in ensuring safe transitions and continuity of care regarding clients’ use of medications. Additional information about safe medication use and transitions of care is discussed in the “Preventing Medication Errors” section of this chapter.
Health Teaching and Health Promotion
When administering medications, nurses teach clients about the medications and potential side effects to promote optimal health. The ANA standard for health teaching and health promotion states, “The registered nurse employs strategies to teach and promote health and wellness.”[18] Specific behaviors related to teaching about medication are as follows[19]:
- Use health teaching and health promotion methods in collaboration with the client’s values, beliefs, health practices, developmental level, learning needs, readiness and ability to learn, language preference, spirituality, culture, and socioeconomic status.
- Provide clients with information and education about intended effects and potential adverse effects of the plan of care.
- Provide anticipatory guidance to clients to promote health and prevent or reduce risk.
In the book Preventing Medication Errors by the Institute of Medicine (2007), the following are additional key national guidelines when teaching clients about safe use of their medications:
- Clients should maintain an active list of all prescription drugs, over-the-counter (OTC) drugs, and dietary supplements they are taking, the reasons for taking them, and any known drug allergies. Every provider involved in the medication-use process for a client should have access to this list.
- Clients should be provided information about side effects, contraindications, methods for handling adverse reactions, and sources for obtaining additional objective, high-quality information.[20]
Evaluation
The “Evaluation” Standard of Practice is defined as, “The registered nurse evaluates progress toward attainment of goals and outcomes.”[21] During evaluation, nurses assess the client and compare the findings against the initial assessment to determine the effectiveness of the interventions and overall nursing care plan. Both the client’s status and the effectiveness of the nursing care must be continuously evaluated and modified as needed.[22]
Read additional information about the nursing process in the “Nursing Process” chapter of Open RN Nursing Fundamentals.
Standards of Professional Performance
ANA’s Standards of Professional Performance describe a competent level of behavior for nurses, including activities related to ethics, culturally congruent practice, communication, collaboration, leadership, education, evidence-based practice, and quality of practice.[23]
The ANA defines culturally congruent practice as the application of evidence-based nursing that is in agreement with the preferred cultural values, beliefs, worldview, and practices of the health care consumer and other stakeholders. Cultural competence represents the process by which nurses demonstrate culturally congruent practice. Nurses must assess the cultural beliefs and practices of their clients and implement culturally congruent interventions when administering medications and teaching about them. Additional information about cultural implications for medication administration is further discussed in the “Cultural and Social Determinants Related to Medication Administration” section later in this chapter.
Critical Thinking Activity 2.2b
A nurse is preparing to administer metoprolol, a cardiac medication, to a client and implements the nursing process:
ASSESSES the vital signs prior to administration and discovers the heart rate is 48.
DIAGNOSES that the heart rate is too low to safely administer the medication per the parameters provided. Establishes the OUTCOME to keep the client’s heart rate within normal range of 60-100.
PLANS to call the provider, as well as report this incident in the shift handoff report.
Implements INTERVENTIONS by withholding the metoprolol at this time, documenting the incident that the medication is withheld, and notifying the provider.
Continues to EVALUATE the client status throughout the shift after not receiving the metoprolol.
The nurse is providing health teaching to a client about the medication before discharge. The nurse provides a handout with instructions, as well as a list of the current medications.
What other information should be provided to the client?
Note: Answers to the Critical Thinking activities can be found in the “Answer Key” sections at the end of the book.
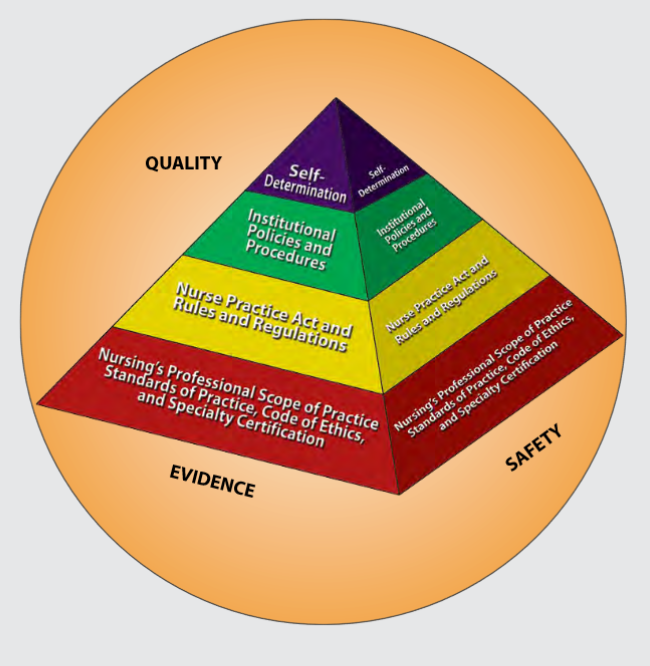
Figure 2.1 is an image from Nursing: Scope and Standards of Practice by the ANA that illustrates how the scope of practice, standards of practice, and code of ethics form the “base” of nursing practice.[24] Nursing practice is further guided by the Nurse Practice Act in the state in which a nurse works, federal and state rules and regulations, institutional policies and procedures, and self-determination by the individual nurse. All these components are required to provide quality, safe client care that is evidence-based. These components will be further discussed in the remaining sections of this chapter.
NCLEX and the Clinical Judgment Model
The National Council Licensure Examination (NCLEX) is the national exam that graduates must pass successfully to obtain their nursing license after graduating from a nursing program of study. The NCLEX-PN is taken to become a licensed practical/vocational nurse (LPN/VN), and the NCLEX-RN is taken to become a licensed registered nurse (RN). The purpose of the NCLEX is to evaluate if a nursing graduate demonstrates the ability to provide safe, competent, entry-level nursing care. The NCLEX is developed by the National Council of State Boards of Nursing (NCSBN), an independent, nonprofit organization composed of the 50 state boards of nursing and other regulatory agencies.[25]
A new edition of the NCLEX was launched in April 2023 that contains “Next Generation” questions. The Next Generation NCLEX (NGN) assesses how well the candidate can think critically and use clinical judgment. The NCSBN defines clinical judgment as “the observed outcome of critical thinking and decision-making. It is an iterative process with multiple steps that uses nursing knowledge to observe and assess presenting situations, identify a prioritized client concern and generate the best possible evidence-based solutions in order to deliver safe client care.”
The NCLEX uses the NCSBN’s Clinical Judgment Measurement Model (NCJMM) to assess the candidate’s ability to use safe clinical judgment when providing nursing care. Exam questions used to assess clinical judgment may be contained in a case study or as individual stand-alone items. A case study contains six questions that are associated with the same client scenario and addresses the following steps in clinical judgment[26]:
- Recognize cues: Identify relevant and important information from different sources (e.g., medical history, vital signs).
- Analyze cues: Organize and connect the recognized cues to the client’s clinical presentation.
- Prioritize hypotheses: Evaluate and prioritize hypotheses (based on urgency, likelihood, risk, difficulty, time constraints, etc.).
- Generate solutions: Identify expected outcomes and use hypotheses to define a set of interventions for the expected outcomes.
- Take action: Implement the solution(s) that address the highest priority.
- Evaluate outcomes: Compare observed outcomes to expected outcomes.
Throughout this book, learning activities are provided to assist students in learning how to apply the nursing process (i.e., ANA’s Standards of Care) to answer NGN-style questions that evaluate clinical judgment. Some of these activities are written, with answers in the Answer Key at the end of the book, and others are interactive and require use of the online book.
- American Nurses Association. (2019). About ANA. https://www.nursingworld.org/ana/about-ana/ ↵
- American Nurses Association. (2015). Code of ethics for nurses with interpretive statements. https://www.nursingworld.org/coe-view-only ↵
- American Nurses Association. (2015). Code of ethics for nurses with interpretive statements. https://www.nursingworld.org/coe-view-only ↵
- American Nurses Association. (2015). Code of ethics for nurses with interpretive statements. https://www.nursingworld.org/coe-view-only ↵
- American Nurses Association. (2015). Code of ethics for nurses with interpretive statements. https://www.nursingworld.org/coe-view-only ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- American Nurses Association. (n.d.). The nursing process. https://www.nursingworld.org/practice-policy/workforce/what-is-nursing/the-nursing-process/ ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- American Nurses Association. (n.d.). The nursing process. https://www.nursingworld.org/practice-policy/workforce/what-is-nursing/the-nursing-process/ ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (3rd ed.). American Nurses Association. ↵
- American Nurses Association. (n.d.) The nursing process. https://www.nursingworld.org/practice-policy/workforce/what-is-nursing/the-nursing-process/ ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- Institute of Medicine. (2007). Preventing medication errors. The National Academies Press. https://doi.org/10.17226/11623 ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- American Nurses Association. (n.d.). The nursing process. https://www.nursingworld.org/practice-policy/workforce/what-is-nursing/the-nursing-process/ ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- American Nurses Association. (2015). Nursing: Scope and standards of practice (3rd ed.). American Nurses Association. ↵
- NCSBN. https://www.ncsbn.org/nclex.htm ↵
- NCSBN. (n.d.). 2023 NCLEX-RN test plan. https://www.ncsbn.org/exams/testplans.page ↵
Since the days of Florence Nightingale, sleep has been recognized as beneficial to health and of great importance during nursing care due to its restorative function. It is common for sleep disturbances and changes in sleep pattern to occur in connection with hospitalization, especially among surgical clients. Clients in medical and surgical units often report disrupted sleep, not feeling refreshed by sleep, wakeful periods during the night, and increased sleepiness during the day. Illness and the stress of being hospitalized are causative factors, but other reasons for insufficient sleep in hospitals may be due to an uncomfortable bed, being too warm or too cold, environmental noise such as IV pump alarms, disturbance from health care personnel and other clients, and pain. The presence of intravenous catheters, a urinary catheter, and drainage tubes can also impair sleep. Increased daytime sleepiness, a consequence of poor-quality sleep at night, can cause decreased mobility and slower recovery from surgery. Research indicates that postoperative sleep disturbances can last for months. Therefore, it is important to provide effective nursing interventions to promote sleep.[1]
Assessment
Begin a focused assessment on a client’s sleep patterns by asking an open-ended question such as, “Do you feel rested upon awakening?” From there, five key sleep characteristics should be assessed: sleep duration, sleep quality, sleep timing, daytime alertness, and the presence of a sleep disorder. Examples of focused interview questions are included in Table 12.3a. These questions have been selected from sleep health questionnaires from the National Sleep Foundation's Sleep Health Index and the National Healthy Sleep Awareness Project.[2]
Table 12.3a Focused Interview Questions Regarding Sleep[3]
| Questions | Normal Findings |
|---|---|
| How many hours do you sleep on an average night? | 7-8 hours for adults (See Table 12.3b for recommended sleep by age range.) |
| During the past month, how would you rate your sleep quality overall? | Very good or fairly good |
| Do you go to bed and wake up at the same time every day, even on weekends? | Yes, they generally maintain a consistent sleep schedule |
| How likely is it for you to fall asleep during the daytime without intending to? Do you struggle to stay awake while you are doing things? | Unlikely |
| How often do you have trouble going to sleep or staying asleep? | Never, rarely, or sometimes |
| During the past two weeks, how many times did you have loud snoring while sleeping?
Note: It is helpful to ask the client’s sleep partner this question. |
Never |
It is also helpful to determine the effects of caffeine intake and medications on a client’s sleep pattern. If a client provides information causing a concern for impaired sleep patterns or a sleep disorder, it is helpful to encourage them to create a sleep diary to share with a health care provider. Use the following information to view a sample sleep diary.
Download a Sleep Diary from the National Heart, Lung, and Blood Institute.
Additional subjective assessment questions can be used to gather information about a clients typical sleep routine so that it can be mirrored during inpatient care, when feasible.
Nurses also perform objective assessments of a client’s sleep patterns during inpatient care. The number of hours slept, wakefulness during the night, and episodes of loud snoring or apnea should be documented. Note physical (e.g., sleep apnea, pain, and urinary frequency) or psychological (e.g., fear or anxiety) circumstances that interrupt sleep, as well as sleepiness and napping during the day.[4],[5]
Concerns about signs of sleep disorders should be communicated to the health care provider for follow-up.
Life Span Considerations
The amount of sleep needed changes over the course of a person’s lifetime. Although sleep needs vary from person to person, Table 12.3b shows general recommendations for different age groups based on recommendations from the American Academy of Sleep Medicine (AASM) and the American Academy of Pediatrics (AAP).[6]
Table 12.3b Recommended Amounts of Sleep by Age Group[7]
| Age | Recommended Amount of Sleep |
|---|---|
| Infants aged 4-12 months | 12-16 hours a day (including naps) |
| Children aged 1-2 years | 11-14 hours a day (including naps) |
| Children aged 3-5 years | 10-13 hours a day (including naps) |
| Children aged 6-12 years | 9-12 hours a day |
| Teens aged 13-18 years | 8-10 hours a day |
| Adults aged 18 years or older | 7–8 hours a day |
If an older adult has Alzheimer’s disease, it often changes their sleeping habits. Some people with Alzheimer’s disease sleep too much; others don’t sleep enough. Some people wake up many times during the night; others wander or yell at night. The person with Alzheimer’s disease isn’t the only one who loses sleep. Caregivers may have sleepless nights, leaving them tired for the challenges they face. Educate caregivers about these steps to promote safety for their loved one and help them and the client sleep better at night:
- Make sure the floor is clear of objects.
- Lock up any medications.
- Attach grab bars in the bathroom.
- Place a gate across the stairs.[8]
Diagnostic Tests
A sleep study may be ordered for a client suspected of having a sleep disorder. A sleep study monitors and records data during a client’s full night of sleep. A sleep study may be performed at a sleep center or at home with a portable diagnostic device. If done at a sleep center, the client will sleep in a bed at the sleep center for the duration of the study. Removable sensors are placed on the person’s scalp, face, eyelids, chest, limbs, and a finger to record brain waves, heart rate, breathing effort and rate, oxygen levels, and muscle movements before, during, and after sleep. There is a small risk of irritation from the sensors, but this will resolve after they are removed.[9] See Figure 12.10[10] of an image of a client with sensors in place for a sleep study.

Diagnoses
NANDA-I nursing diagnoses related to sleep include Disturbed Sleep Pattern, Insomnia, Readiness for Enhanced Sleep, and Sleep Deprivation.[11] When creating a nursing care plan for a client, review a nursing care planning source for current NANDA-I approved nursing diagnoses and interventions related to sleep. See Table 12.3c for the definition and selected defining characteristics of Sleep Deprivation.[12]
Table 12.3c Sample NANDA-I Nursing Diagnosis Related to Sleep Deprivation[13]
| NANDA-I Diagnosis | Definition | Selected Defining Characteristics |
|---|---|---|
| Sleep Deprivation | Prolonged periods of time without sustained natural, periodic suspension of relative consciousness that provides rest. | Agitation
Alteration in concentration Anxiety Apathy Combativeness Decrease in functional ability Decrease in reaction time Drowsiness Fatigue Hallucinations Heightened sensitivity to pain Irritability Restlessness |
A sample nursing diagnostic statement is, “Sleep Deprivation related to an overstimulating environment as evidenced by irritability, difficulty concentrating, and drowsiness.”
Outcome Identification
An overall goal related to sleep is, “The client will awaken refreshed once adequate time is spent sleeping.”[14]
A sample SMART outcome is, “The client will identify preferred actions to ensure adequate sleep by discharge.”[15]
Planning Interventions
Evidence-based nursing interventions to enhance sleep are summarized in the following box.
Sleep Enhancement Interventions[16],[17]
- Adjust the environment (e.g., light, noise, temperature, mattress, and bed) to promote sleep
- Encourage the client to establish a bedtime routine to facilitate wakefulness to sleep
- Facilitate maintenance of the client’s usual bedtime routines during inpatient care
- Encourage elimination of stressful situations before bedtime
- Instruct the client to avoid bedtime foods and beverages that interfere with sleep
- Encourage the client to limit daytime sleep and participate in activity, as appropriate
- Bundle care activities to minimize the number of awakenings by staff to allow for sleep cycles of at least 90 minutes
- Consider sleep apnea as a possible cause and notify the provider for a possible referral for a sleep study when daytime drowsiness occurs despite adequate periods of undisturbed night sleep
- Educate the client regarding sleep-enhancing techniques
Transforming Hospitals Into Restful Environments to Promote Healing
Nurses nationwide have been researching innovative ways to transform hospitals into more restful environments that promote healing. As reported in the American Nurse, strategies include using red lights at night to reduce light exposure, reducing environmental noise, bundling care, offering sleep aids, and providing clienteducation[18]:
- Switching to Red Lights: Nurses can use red lights when providing care at night. Adult and pediatric clients were found to sleep better with reduced white lights.
- Reduce Environmental Noise: Clients were surveyed regarding factors that affected their ability to sleep, and results indicated bed noises, alarms, squeaking equipment, and sounds from other clients. Noise can be reduced by replacing the wheels on the trash cans and squeaky wheels on chairs, repairing malfunctioning motors on beds, switching automatic paper towel machines in the hallways with manual ones, and altering the times floors are buffed. Visitor rules can be implemented, such as no overnight stays in semiprivate rooms and overnight visitors in private rooms were asked to not use their cell phones, turn on the TV, or use bright lights at night.
- Bundling Care: Nurses reinforce bundling care by interdisciplinary team members to reduce sleep interruptions. For example, a “Quiet Time” policy can be set from midnight to 5 a.m. Quiet Time includes dimming lights, closing client room doors, and talking in lower voices.
- Offering Sleep Aids: Nurses can ask clients about what aids they use at home to help them sleep, such as extra pillows or listening to music. On admission, sleep kits can be provided with ear plugs and eye masks and at bedtime, warm washcloths can be offered to clients for comfort.
- Client Education: Clients and families can be provided with printed materials on the benefits of sleep and rest for optimal healing, participating in rehabilitative therapies, and prevention of delirium.
Pharmacological Interventions
See specific information about medications used to facilitate sleep in the previous “Sleep Disorders” section of this chapter.
Implementing Interventions
When implementing interventions to promote sleep, it is important to customize them according to the specific client’s needs and concerns. If medications are administered to promote sleep, fall precautions should be implemented, and the nurse should monitor for potential side effects, such as dizziness, drowsiness, worsening of depression or suicidal thoughts, or unintentionally walking or eating while asleep.
Evaluation
When evaluating the effectiveness of interventions, start by asking the client how rested they feel upon awakening. Determine the effectiveness of interventions based on the established SMART outcomes customized for each client situation.
Since the days of Florence Nightingale, sleep has been recognized as beneficial to health and of great importance during nursing care due to its restorative function. It is common for sleep disturbances and changes in sleep pattern to occur in connection with hospitalization, especially among surgical clients. Clients in medical and surgical units often report disrupted sleep, not feeling refreshed by sleep, wakeful periods during the night, and increased sleepiness during the day. Illness and the stress of being hospitalized are causative factors, but other reasons for insufficient sleep in hospitals may be due to an uncomfortable bed, being too warm or too cold, environmental noise such as IV pump alarms, disturbance from health care personnel and other clients, and pain. The presence of intravenous catheters, a urinary catheter, and drainage tubes can also impair sleep. Increased daytime sleepiness, a consequence of poor-quality sleep at night, can cause decreased mobility and slower recovery from surgery. Research indicates that postoperative sleep disturbances can last for months. Therefore, it is important to provide effective nursing interventions to promote sleep.[19]
Assessment
Begin a focused assessment on a client’s sleep patterns by asking an open-ended question such as, “Do you feel rested upon awakening?” From there, five key sleep characteristics should be assessed: sleep duration, sleep quality, sleep timing, daytime alertness, and the presence of a sleep disorder. Examples of focused interview questions are included in Table 12.3a. These questions have been selected from sleep health questionnaires from the National Sleep Foundation's Sleep Health Index and the National Healthy Sleep Awareness Project.[20]
Table 12.3a Focused Interview Questions Regarding Sleep[21]
| Questions | Normal Findings |
|---|---|
| How many hours do you sleep on an average night? | 7-8 hours for adults (See Table 12.3b for recommended sleep by age range.) |
| During the past month, how would you rate your sleep quality overall? | Very good or fairly good |
| Do you go to bed and wake up at the same time every day, even on weekends? | Yes, they generally maintain a consistent sleep schedule |
| How likely is it for you to fall asleep during the daytime without intending to? Do you struggle to stay awake while you are doing things? | Unlikely |
| How often do you have trouble going to sleep or staying asleep? | Never, rarely, or sometimes |
| During the past two weeks, how many times did you have loud snoring while sleeping?
Note: It is helpful to ask the client’s sleep partner this question. |
Never |
It is also helpful to determine the effects of caffeine intake and medications on a client’s sleep pattern. If a client provides information causing a concern for impaired sleep patterns or a sleep disorder, it is helpful to encourage them to create a sleep diary to share with a health care provider. Use the following information to view a sample sleep diary.
Download a Sleep Diary from the National Heart, Lung, and Blood Institute.
Additional subjective assessment questions can be used to gather information about a clients typical sleep routine so that it can be mirrored during inpatient care, when feasible.
Nurses also perform objective assessments of a client’s sleep patterns during inpatient care. The number of hours slept, wakefulness during the night, and episodes of loud snoring or apnea should be documented. Note physical (e.g., sleep apnea, pain, and urinary frequency) or psychological (e.g., fear or anxiety) circumstances that interrupt sleep, as well as sleepiness and napping during the day.[22],[23]
Concerns about signs of sleep disorders should be communicated to the health care provider for follow-up.
Life Span Considerations
The amount of sleep needed changes over the course of a person’s lifetime. Although sleep needs vary from person to person, Table 12.3b shows general recommendations for different age groups based on recommendations from the American Academy of Sleep Medicine (AASM) and the American Academy of Pediatrics (AAP).[24]
Table 12.3b Recommended Amounts of Sleep by Age Group[25]
| Age | Recommended Amount of Sleep |
|---|---|
| Infants aged 4-12 months | 12-16 hours a day (including naps) |
| Children aged 1-2 years | 11-14 hours a day (including naps) |
| Children aged 3-5 years | 10-13 hours a day (including naps) |
| Children aged 6-12 years | 9-12 hours a day |
| Teens aged 13-18 years | 8-10 hours a day |
| Adults aged 18 years or older | 7–8 hours a day |
If an older adult has Alzheimer’s disease, it often changes their sleeping habits. Some people with Alzheimer’s disease sleep too much; others don’t sleep enough. Some people wake up many times during the night; others wander or yell at night. The person with Alzheimer’s disease isn’t the only one who loses sleep. Caregivers may have sleepless nights, leaving them tired for the challenges they face. Educate caregivers about these steps to promote safety for their loved one and help them and the client sleep better at night:
- Make sure the floor is clear of objects.
- Lock up any medications.
- Attach grab bars in the bathroom.
- Place a gate across the stairs.[26]
Diagnostic Tests
A sleep study may be ordered for a client suspected of having a sleep disorder. A sleep study monitors and records data during a client’s full night of sleep. A sleep study may be performed at a sleep center or at home with a portable diagnostic device. If done at a sleep center, the client will sleep in a bed at the sleep center for the duration of the study. Removable sensors are placed on the person’s scalp, face, eyelids, chest, limbs, and a finger to record brain waves, heart rate, breathing effort and rate, oxygen levels, and muscle movements before, during, and after sleep. There is a small risk of irritation from the sensors, but this will resolve after they are removed.[27] See Figure 12.10[28] of an image of a client with sensors in place for a sleep study.

Diagnoses
NANDA-I nursing diagnoses related to sleep include Disturbed Sleep Pattern, Insomnia, Readiness for Enhanced Sleep, and Sleep Deprivation.[29] When creating a nursing care plan for a client, review a nursing care planning source for current NANDA-I approved nursing diagnoses and interventions related to sleep. See Table 12.3c for the definition and selected defining characteristics of Sleep Deprivation.[30]
Table 12.3c Sample NANDA-I Nursing Diagnosis Related to Sleep Deprivation[31]
| NANDA-I Diagnosis | Definition | Selected Defining Characteristics |
|---|---|---|
| Sleep Deprivation | Prolonged periods of time without sustained natural, periodic suspension of relative consciousness that provides rest. | Agitation
Alteration in concentration Anxiety Apathy Combativeness Decrease in functional ability Decrease in reaction time Drowsiness Fatigue Hallucinations Heightened sensitivity to pain Irritability Restlessness |
A sample nursing diagnostic statement is, “Sleep Deprivation related to an overstimulating environment as evidenced by irritability, difficulty concentrating, and drowsiness.”
Outcome Identification
An overall goal related to sleep is, “The client will awaken refreshed once adequate time is spent sleeping.”[32]
A sample SMART outcome is, “The client will identify preferred actions to ensure adequate sleep by discharge.”[33]
Planning Interventions
Evidence-based nursing interventions to enhance sleep are summarized in the following box.
Sleep Enhancement Interventions[34],[35]
- Adjust the environment (e.g., light, noise, temperature, mattress, and bed) to promote sleep
- Encourage the client to establish a bedtime routine to facilitate wakefulness to sleep
- Facilitate maintenance of the client’s usual bedtime routines during inpatient care
- Encourage elimination of stressful situations before bedtime
- Instruct the client to avoid bedtime foods and beverages that interfere with sleep
- Encourage the client to limit daytime sleep and participate in activity, as appropriate
- Bundle care activities to minimize the number of awakenings by staff to allow for sleep cycles of at least 90 minutes
- Consider sleep apnea as a possible cause and notify the provider for a possible referral for a sleep study when daytime drowsiness occurs despite adequate periods of undisturbed night sleep
- Educate the client regarding sleep-enhancing techniques
Transforming Hospitals Into Restful Environments to Promote Healing
Nurses nationwide have been researching innovative ways to transform hospitals into more restful environments that promote healing. As reported in the American Nurse, strategies include using red lights at night to reduce light exposure, reducing environmental noise, bundling care, offering sleep aids, and providing clienteducation[36]:
- Switching to Red Lights: Nurses can use red lights when providing care at night. Adult and pediatric clients were found to sleep better with reduced white lights.
- Reduce Environmental Noise: Clients were surveyed regarding factors that affected their ability to sleep, and results indicated bed noises, alarms, squeaking equipment, and sounds from other clients. Noise can be reduced by replacing the wheels on the trash cans and squeaky wheels on chairs, repairing malfunctioning motors on beds, switching automatic paper towel machines in the hallways with manual ones, and altering the times floors are buffed. Visitor rules can be implemented, such as no overnight stays in semiprivate rooms and overnight visitors in private rooms were asked to not use their cell phones, turn on the TV, or use bright lights at night.
- Bundling Care: Nurses reinforce bundling care by interdisciplinary team members to reduce sleep interruptions. For example, a “Quiet Time” policy can be set from midnight to 5 a.m. Quiet Time includes dimming lights, closing client room doors, and talking in lower voices.
- Offering Sleep Aids: Nurses can ask clients about what aids they use at home to help them sleep, such as extra pillows or listening to music. On admission, sleep kits can be provided with ear plugs and eye masks and at bedtime, warm washcloths can be offered to clients for comfort.
- Client Education: Clients and families can be provided with printed materials on the benefits of sleep and rest for optimal healing, participating in rehabilitative therapies, and prevention of delirium.
Pharmacological Interventions
See specific information about medications used to facilitate sleep in the previous “Sleep Disorders” section of this chapter.
Implementing Interventions
When implementing interventions to promote sleep, it is important to customize them according to the specific client’s needs and concerns. If medications are administered to promote sleep, fall precautions should be implemented, and the nurse should monitor for potential side effects, such as dizziness, drowsiness, worsening of depression or suicidal thoughts, or unintentionally walking or eating while asleep.
Evaluation
When evaluating the effectiveness of interventions, start by asking the client how rested they feel upon awakening. Determine the effectiveness of interventions based on the established SMART outcomes customized for each client situation.
Client Scenario
Mrs. Salvo is a 65-year-old woman admitted to the hospital for a gastrointestinal (GI) bleed. She has been hospitalized for three days on the medical-surgical floor. During this time, she has received four units of PRBCs, has undergone a colonoscopy and an upper GI series, and had hemoglobin levels drawn every four hours. The nurse reports to the client’s room to conduct an assessment prior to beginning the 11 p.m.-7 a.m. shift.
Although Mrs. Salvo’s hemoglobin has stabilized for the last 24 hours, Mrs. Salvo appears fatigued with bags under her eyes. In conversation with her, she yawns frequently and wanders off in her train of thought. She reports, “You can’t get any rest in here. I am poked and prodded at least once an hour.”
Applying the Nursing Process
Assessment: The nurse notes that Mrs. Salvo has bags under her eyes, is yawning frequently, reports difficulty achieving rest, and seems to have difficulty following the conversation.
Based on the assessment information that has been gathered, the following nursing care plan is created for Mrs. Salvo:
Nursing Diagnosis: Disturbed Sleep Pattern related to interruptions for therapeutic monitoring as evidenced by reports of difficulty achieving rest, bags under eyes, frequent yawning, and difficulty following conversation.
Overall Goal: The client will demonstrate improvement in sleeping pattern.
SMART Expected Outcome: Mrs. Salvo will report feeling more rested on awakening within 24 hours.
Planning and Implementing Nursing Interventions:
The nurse will assess the client’s sleep pattern and therapeutic monitoring disturbances. The nurse will group lab draws, vital signs, assessments, and other care tasks to decrease sleep disruption. The nurse will ensure the client’s door is closed and lighting is turned down to create a restful environment. The nurse will complete as many tasks as possible when Mrs. Salvo is awake and advocate with the interprofessional team for uninterrupted periods of rest during the night.
Sample Documentation:
Mrs. Salvo has a disturbed sleep pattern due to frequent therapeutic monitoring. Mrs. Salvo reports difficulty achieving rest, and despite stabilization in hemoglobin level, continues to demonstrate signs of fatigue. Interventions have been implemented to group therapeutic care to minimize disruption to the client’s sleep.
Evaluation:
The following morning, Mrs. Salvo reports improved sleep and feeling more rested with fewer awakenings throughout the night. SMART outcome "met."
Client Scenario
Mrs. Salvo is a 65-year-old woman admitted to the hospital for a gastrointestinal (GI) bleed. She has been hospitalized for three days on the medical-surgical floor. During this time, she has received four units of PRBCs, has undergone a colonoscopy and an upper GI series, and had hemoglobin levels drawn every four hours. The nurse reports to the client’s room to conduct an assessment prior to beginning the 11 p.m.-7 a.m. shift.
Although Mrs. Salvo’s hemoglobin has stabilized for the last 24 hours, Mrs. Salvo appears fatigued with bags under her eyes. In conversation with her, she yawns frequently and wanders off in her train of thought. She reports, “You can’t get any rest in here. I am poked and prodded at least once an hour.”
Applying the Nursing Process
Assessment: The nurse notes that Mrs. Salvo has bags under her eyes, is yawning frequently, reports difficulty achieving rest, and seems to have difficulty following the conversation.
Based on the assessment information that has been gathered, the following nursing care plan is created for Mrs. Salvo:
Nursing Diagnosis: Disturbed Sleep Pattern related to interruptions for therapeutic monitoring as evidenced by reports of difficulty achieving rest, bags under eyes, frequent yawning, and difficulty following conversation.
Overall Goal: The client will demonstrate improvement in sleeping pattern.
SMART Expected Outcome: Mrs. Salvo will report feeling more rested on awakening within 24 hours.
Planning and Implementing Nursing Interventions:
The nurse will assess the client’s sleep pattern and therapeutic monitoring disturbances. The nurse will group lab draws, vital signs, assessments, and other care tasks to decrease sleep disruption. The nurse will ensure the client’s door is closed and lighting is turned down to create a restful environment. The nurse will complete as many tasks as possible when Mrs. Salvo is awake and advocate with the interprofessional team for uninterrupted periods of rest during the night.
Sample Documentation:
Mrs. Salvo has a disturbed sleep pattern due to frequent therapeutic monitoring. Mrs. Salvo reports difficulty achieving rest, and despite stabilization in hemoglobin level, continues to demonstrate signs of fatigue. Interventions have been implemented to group therapeutic care to minimize disruption to the client’s sleep.
Evaluation:
The following morning, Mrs. Salvo reports improved sleep and feeling more rested with fewer awakenings throughout the night. SMART outcome "met."
Learning Activities
(Answers to “Learning Activities” can be found in the “Answer Key” at the end of the book. Answers to interactive activity elements will be provided within the element as immediate feedback.)
Scenario A
A nurse is caring for a client who has been hospitalized after undergoing hip-replacement surgery. The client complains of not sleeping well and feels very drowsy during the day.
- What factors are affecting the client’s sleep pattern?
- What assessments should the nurse perform?
- What SMART outcome can be established for this client?
- Outline interventions the nurse can implement to enhance sleep for this client.
- How will the nurse evaluate if the interventions are effective?
Scenario B
A nurse is assigned to work rotating shifts and develops difficulty sleeping.
- Why do rotating shifts affect a person’s sleep pattern?
- What are the symptoms of insomnia?
- Describe healthy sleep habits the nurse can adopt for more restful sleep.

Test your knowledge using this NCLEX Next Generation-style bowtie question. You may reset and resubmit your answers to this question an unlimited number of times.[37]
Learning Activities
(Answers to “Learning Activities” can be found in the “Answer Key” at the end of the book. Answers to interactive activity elements will be provided within the element as immediate feedback.)
Scenario A
A nurse is caring for a client who has been hospitalized after undergoing hip-replacement surgery. The client complains of not sleeping well and feels very drowsy during the day.
- What factors are affecting the client’s sleep pattern?
- What assessments should the nurse perform?
- What SMART outcome can be established for this client?
- Outline interventions the nurse can implement to enhance sleep for this client.
- How will the nurse evaluate if the interventions are effective?
Scenario B
A nurse is assigned to work rotating shifts and develops difficulty sleeping.
- Why do rotating shifts affect a person’s sleep pattern?
- What are the symptoms of insomnia?
- Describe healthy sleep habits the nurse can adopt for more restful sleep.

Test your knowledge using this NCLEX Next Generation-style bowtie question. You may reset and resubmit your answers to this question an unlimited number of times.[38]
Circadian rhythms: Body rhythms that direct a wide variety of functions, including wakefulness, body temperature, metabolism, and the release of hormones. They control the timing of sleep, causing individuals to feel sleepy at night and creating a tendency to wake in the morning without an alarm. (Chapter 12.2)
Insomnia: A common sleep disorder that causes trouble falling asleep, staying asleep, or getting good quality sleep. Insomnia interferes with daily activities and causes the person to feel unrested or sleepy during the day. Short-term insomnia may be caused by stress or changes in one’s schedule or environment, lasting a few days or weeks. Chronic insomnia occurs three or more nights a week, lasts more than three months, and cannot be fully explained by another health problem or a medicine. Chronic insomnia raises the risk of high blood pressure, coronary heart disease, diabetes, and cancer. (Chapter 12.2)
Microsleep: Brief moments of sleep that occur when a person is awake. A person can't control microsleep and might not be aware of it. (Chapter 12.2)
Narcolepsy: An uncommon sleep disorder that causes periods of extreme daytime sleepiness and sudden, brief episodes of deep sleep during the day. (Chapter 12.2)
Non-REM sleep: Slow-wave sleep when restoration takes place and the body’s temperature, heart rate, and oxygen consumption decrease. (Chapter 12.2)
Obstructive sleep apnea (OSA): A common sleep condition that occurs when the upper airway becomes repeatedly blocked during sleep, reducing or completely stopping airflow. If the brain does not send the signals needed to breathe, the condition may be called central sleep apnea. (Chapter 12.2)
REM sleep: Rapid eye movement (REM) sleep when heart rate and respiratory rate increase, eyes twitch, and brain activity increases. Dreaming occurs during REM sleep, and muscles become limp to prevent acting out one’s dreams. (Chapter 12.2)
Sleep diary: A record of the time a person goes to sleep, wakes up, and takes naps each day for 1-2 weeks. Timing of activities such as exercising and drinking caffeine or alcohol are also recorded, as well as feelings of sleepiness throughout the day. (Chapter 12.2)
Sleep study: A diagnostic test that monitors and records data during a client’s full night of sleep. A sleep study may be performed at a sleep center or at home with a portable diagnostic device. (Chapter 12.2)
Sleep-wake homeostasis: The homeostatic sleep drive keeps track of the need for sleep, reminds the body to sleep after a certain time, and regulates sleep intensity. This sleep drive gets stronger every hour a person is awake and causes individuals to sleep longer and more deeply after a period of sleep deprivation. (Chapter 12.2)
Learning Objectives
- Reflect upon personal and cultural values, beliefs, biases, and heritage[39]
- Embrace diversity, equity, inclusivity, health promotion, and health care for individuals of diverse geographic, cultural, ethnic, racial, gender, and spiritual backgrounds across the life span[40]
- Demonstrate respect, equity, and empathy in actions and interactions with all health care consumers[41]
- Participate in life-long learning to understand cultural preferences, worldviews, choices, and decision-making processes of diverse clients[42]
- Adapt care considering all aspects of diversity
- Identify principles of protecting client dignity
- Identify principles of holistic, client-centered care
- Identify strategies to advocate for clients
- Identify principles of religion and spirituality
No matter who we are or where we come from, every person was raised with cultural values and beliefs. The impact of culture on a person’s health is profound because it affects many health beliefs, such as perceived causes of illness, ways to prevent illness, and acceptance of medical treatments. Culturally responsive care integrates these cultural beliefs into an individual's health care. Culturally responsive care is intentional and promotes trust and rapport with clients. At its heart, culturally responsive care is client-centered care. The American Nurses Association (ANA) states, "The art of nursing is demonstrated by unconditionally accepting the humanity of others, respecting their need for dignity and worth, while providing compassionate, comforting care."[43]
Nurses provide holistic care when incorporating their clients’ physical, mental, spiritual, cultural, and social needs into their health care (referred to as holism). As a nursing student, you are undertaking a journey of developing cultural competency with an attitude of cultural humility as you learn how to provide holistic care to your clients. Cultural competence is a lifelong process of applying evidence-based nursing in agreement with the cultural values, beliefs, worldview, and practices of clients to produce improved client outcomes.[44],[45],[46]
Cultural humility is defined by the American Nurses Association as, "A humble and respectful attitude toward individuals of other cultures that pushes one to challenge their own cultural biases, realize they cannot know everything about other cultures, and approach learning about other cultures as a life-long goal and process."[47] Nurses improve the quality of health care by understanding, respecting, and incorporating their clients' cultural values, beliefs, and preferences, which can ultimately help reduce health disparities.[48]
This chapter will introduce concepts related to adapting nursing care that considers all aspects of diversity.

