Open Resources for Nursing (Open RN)
Learning Objectives
- Perform a general survey assessment, including vital signs, ability to communicate, appropriateness of behaviors and responses, general mobility, and basic nutritional and fluid status
- Modify assessment techniques to reflect variations across the life span, cultural values and beliefs, and gender expression
- Document actions and observations
- Recognize and report significant deviations from norms
“Learn to see, learn to hear, learn to feel, learn to smell, and know that by practice alone can you become expert.”[1]
This quote provides a good description of learning how to perform a general survey assessment. A general survey assessment is a component of a patient assessment that observes the entire patient as a whole. General surveys begin with the initial patient contact and continue throughout the helping relationship. In this instance, observation includes using all five senses to gather cues. Nurses begin assessing patients from the moment they meet them, noting their appearance, posture, gait, verbal communication, nonverbal communication, and behaviors. Cues obtained during a general survey assessment are used to guide additional focused assessments in areas of concern.
Introduction to the Nursing Process
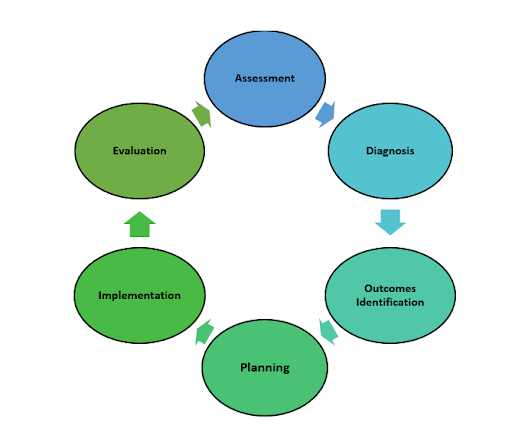
Before discussing the components of a general survey, it is important to understand how assessment fits under the standards for professional nursing practice established by the American Nurses Association (ANA). These standards are the foundation of the nursing profession and include duties that all registered nurses, regardless of role or specialty, are expected to perform competently.[2] There are six components of the nursing process: Assessment, Diagnosis, Outcomes Identification, Planning, Implementation, and Evaluation. See Figure 1.1[3] for an illustration of the nursing process. The mnemonic ADOPIE is an easy way to remember the ANA Standards and the nursing process. The nursing process is a continuous, cyclic process that is constantly adapting to the patient’s current health status. This textbook contains several chapters pertaining to techniques used during the assessment phase of the nursing process.
Read more about the “Nursing Process” in the Open RN Nursing Fundamentals textbook.
Assessment
According to the ANA, assessment includes collecting “pertinent data, including but not limited to, demographics, social determinants of health, health disparities, and physical, functional, psychosocial, emotional, cognitive, sexual, cultural, age-related, environmental, spiritual/transpersonal, and economic assessments in a systematic, ongoing process with compassion and respect for the inherent dignity, worth, and unique attributes of every person.”[4]
Patient data is considered either subjective or objective, and it can be collected from multiple sources.
Subjective Assessment Data
Subjective data is information obtained from the patient and/or family members and offers important cues from their perspectives. When documenting subjective data, it should be in quotation marks and start with verbiage such as, “The patient reports…” or “The patient’s wife states…” It is vital for the nurse to establish rapport with a patient to obtain accurate, valuable subjective data regarding the mental, emotional, and spiritual aspects of their condition.
Example. An example of documented subjective data obtained from a patient assessment is, “The patient reports pain severity of 2 on a 0-10 scale.” Additionally, if you create an inference, then that data is considered subjective. For example, documenting an inference, such as “The patient appears anxious,” is subjective data.
There are two types of subjective information, primary and secondary. Primary data is information provided directly by the patient. Patients are the best source of information about their bodies and feelings, and the nurse who actively listens to a patient will often learn valuable information while also promoting a sense of well-being. Information collected from a family member, chart, or other sources is known as secondary data. Family members can provide important information, especially for infants and children or when the patient is unable to speak for themselves.
Objective Assessment Data
Objective data is anything that you can observe through your senses of hearing, sight, smell, and touch while assessing the patient. Objective data is reproducible, meaning another person can easily obtain the same data. Examples of objective data are vital signs, physical examination findings, and laboratory results.
Example. An example of documented objective data is, “The patient’s radial pulse is 58 and regular, and their skin feels warm and dry.”
Sources of Assessment Data
Assessment data is collected in three ways: during a focused interview, during physical examination, or while reviewing laboratory and diagnostic test results.
Interviewing
Interviewing includes asking the patient questions, listening, and observing verbal and nonverbal communication. Reviewing the chart prior to interviewing the patient eliminates redundancy in the interview process and allows the nurse to hone in on the most significant areas of concern or need for clarification. However, if information in the chart does not make sense or is incomplete, the nurse should use the interview process to verify data with the patient.
When beginning an interview, it may be helpful to start with questions related to the patient’s medical diagnoses to gather information about how they have affected the patient’s functioning, relationships, and lifestyle. Listen carefully and ask for clarification when something isn’t clear to you. Patients may not volunteer important information because they don’t realize it is important for their care. By using critical thinking and active listening, you may discover valuable cues that are important to provide safe, quality nursing care. Sometimes nursing students can feel uncomfortable with having difficult conversations or asking personal questions because of generational or other differences. Don’t shy away from asking about information that is important to know for safe patient care. Most patients will be grateful that you cared enough to ask and listen.
Be alert and attentive to how the patient answers questions, as well as when they do not answer a question. Nonverbal communication and body language can be cues to important information that requires further investigation. A keen sense of observation is important. To avoid making inappropriate inferences, the nurse should validate any cues. For example, a nurse may make an inference that a patient is depressed when the patient avoids making eye contact during an interview. However, upon further questioning, the nurse may discover that the patient’s cultural background believes direct eye contact to be disrespectful and this is why they are avoiding eye contact.
Read more information about communicating with patients in the “Communication” chapter of the Open RN Nursing Fundamentals book.
Physical Examination
Physical examination is a systematic data collection method of the body that uses the techniques of inspection, auscultation, palpation, and percussion. Inspection is the observation of a patient’s anatomical structures. Auscultation is listening to sounds, such as heart, lung, and bowel sounds, created by organs using a stethoscope. Palpation is the use of touch to evaluate organs for size, location, or tenderness. Percussion is an advanced physical examination technique where body parts are tapped with fingers to determine their size and if fluid is present. See Figure 1.2[5] for an image of a nurse performing a physical examination.

Registered Nurses (RNs) complete a physical examination and analyze the findings as part of the nursing process. Collection of physical examination data can be delegated to Licensed Practical Nurses/Licensed Vocational Nurses (LPNs/LVNs), or measurements such as vital signs and weight may be delegated to Unlicensed Assistive Personnel (UAP) when it is appropriate to do so. However, the RN remains responsible for analyzing the findings.
Assessment data is documented in the patient’s electronic medical record (EMR), an electronic version of the patient’s paper medical chart.
Reviewing Laboratory and Diagnostic Test Results
Reviewing laboratory and diagnostic test results is an important component of the assessment phase of the nursing process and provides relevant and useful information related to the needs of the patient. Understanding how normal and abnormal results affect patient care is important when implementing the nursing care plan and administering prescriptions.
Read more about interpreting laboratory and diagnostic testing results based on nursing concepts in the Open RN Nursing Fundamentals textbook.
- Dallas Hall, W. (1990). Chapter 209: An overview of the general examination. In Walker, H. K., Hall, W. D., Hurst, J. W. (Eds.), Clinical methods: The history, physical, and laboratory examinations (3rd ed.). Butterworths. https://www.ncbi.nlm.nih.gov/books/NBK706/ ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- "The Nursing Process” by Kim Ernstmeyer at Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- “13394660711603.jpg” by CDC/Amanda Mills is in the Public Domain. ↵
Fluids found outside cells in the intravascular or interstitial spaces.
A localized pathogen that spreads to a secondary location.
An infection that becomes disseminated throughout the body.

