Open Resources for Nursing (Open RN)
The cost of health care in the United States is higher than any other country in the world and has a significant financial impact on our economy.[1] U.S. health care spending grew 4.1 percent in 2022, reaching $ 4.5 trillion or $13,493 per person. Health care spending accounts for 17.3 percent of our Gross Domestic Product (GDP), the total value of goods produced and services provided annually.[2] See Figure 8.1[3] for a graph of health care cost as a percentage of GDP in the United States compared to other countries around the world.

Despite spending more money on health care than other high-income countries, the United States has some of the poorest health outcomes, such as the lowest life expectancy, the highest infant mortality rate, and a higher prevalence of chronic diseases.[4] The increasing costs of health care also have several negative impacts on society, employers, and individuals, including the following effects[5]:
- When the government spends more on health care, the national debt increases and funds available for other programs decrease.
- When people spend more on health care, they have less money to spend on other items.
- When health insurance is paid by employers, employees are paid less.
- When employers spend more on health care, the costs of their products and services increase. Jobs may be moved to countries with lower health care costs.
- An increasing number of people cannot afford health care insurance. When people without health care insurance receive health care, they often cannot pay for it. As a result of unpaid bills, this care is indirectly paid for by other people paying increased insurance premiums and taxes.
- People without health care insurance may not seek preventative care and develop a more costly, serious medical disorder that could have been prevented.
- Medical bills that are not covered by health insurance can cause bankruptcy.
There are several national trends affecting the cost of health care and related impacts, including the aging population, increased costs of medical technology, increased prescription medication cost, the Affordable Care Act, social determinants of health, etc. These trends can be further classified as intrinsic or extrinsic factors. Intrinsic factors related to increased health care costs are inherent to the characteristics and needs of the population. One significant intrinsic factor is the demographics of the population, such as age, gender, and overall health status. An aging population, for example, typically requires more medical care due to the prevalence of chronic conditions and the natural decline in health associated with aging. Another intrinsic factor is the demand for health care services. As people become more health-conscious, the demand for preventive care, regular check-ups, and advanced treatments rises, leading to increased overall health care spending. Additionally, the extent and nature of health insurance coverage play a crucial role. Comprehensive insurance plans often lead to higher utilization of health care services, as insured individuals are more likely to seek medical care, knowing that a significant portion of the costs will be covered by their insurance.
Extrinsic factors are external elements that impact health care costs. One of the most prominent extrinsic factors is the availability and adoption of medical technology. Advanced diagnostic tools, treatment methods, and surgical techniques can drive up costs due to their high development, implementation, and maintenance expenses. While these technologies can significantly improve patient outcomes, they also contribute to rising health care expenditures. Another critical extrinsic factor is the cost of prescription drugs. Pharmaceutical pricing strategies, including research and development costs, marketing, and profit margins, often lead to high prices for medications, especially for new and specialized drugs. Workforce costs are also a significant extrinsic factor. The salaries and benefits of health care professionals, including doctors, nurses, and administrative staff, constitute a substantial portion of health care expenses. These costs are influenced by factors such as education and training requirements, labor market conditions, and regulatory policies. Addressing these extrinsic factors requires strategic planning and policy interventions to balance cost containment with the quality and accessibility of health care services.
Aging Population
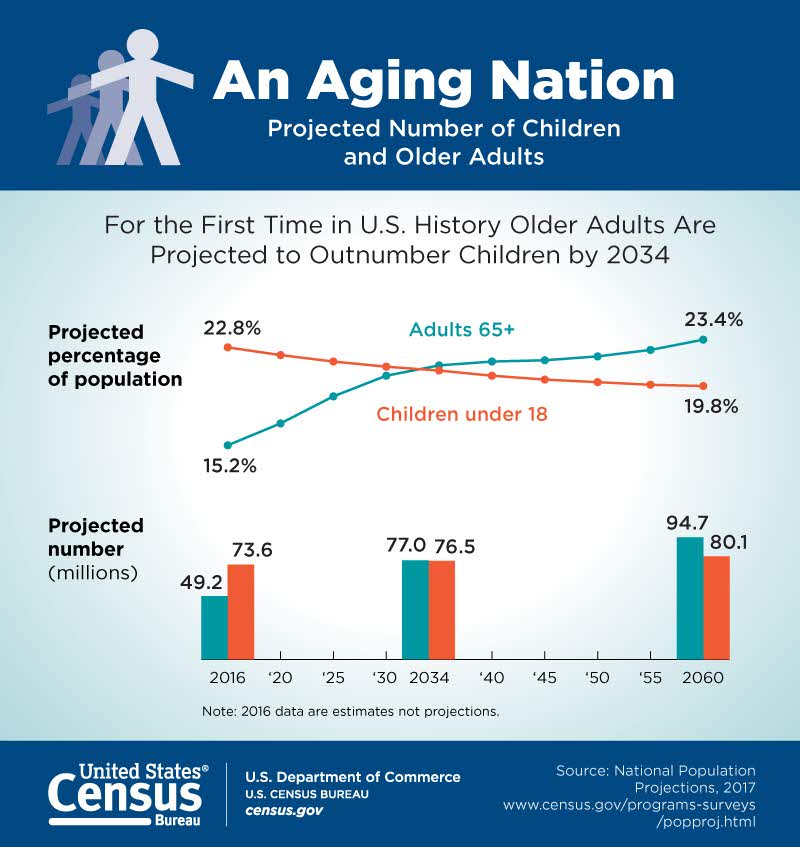
According to the Agency for Healthcare Research and Quality (AHRQ), the United States has a growing number of older adults (age 65 years or older) who are living longer than previous generations. It is anticipated that older adults will make up more than 20 percent of the U.S. population by 2030.[6] See Figure 8.2[7] for an illustration of the aging population from the U.S. Census Bureau. This change in demographics will result in increased national health care costs because older adults typically experience more chronic conditions than younger populations, requiring expensive specialty and long-term care.[8]
Increased Costs of Medical Technology
Highly visible medical technologies, such as organ transplantation, diagnostic imaging systems, and biotechnology products, attract both praise and blame. Evolving medical technologies may save lives and improve a client’s health status, but they are also viewed as a dominant cause of continued escalation of medical costs. Research suggests that medical technology accounts for about 10 to 40 percent of the increase in health care expenditures over time.[9] These costs also lead to further ethical dilemmas as decisions regarding what scarce resources are provided to which patients are made. See Figure 8.3[10] for an image of common technology used in health care.

Medical technologies, especially new ones, must justify their costs in a climate of competing claims on limited resources. Resource allocation follows American society's objective of cost effectiveness: if a new technology improves health outcomes at a lower cost than existing technologies, it should be adopted; otherwise, it should not.[11]
Increased Prescription Medication Costs
Retail prices for commonly-used prescription medications continue to increase twice as much as inflation, contributing to increased health care costs and making these life-sustaining medicines potentially unaffordable to many Americans. According to a recent AARP Rx Price Watch report, in 2020 prices for 260 commonly used medications increased 2.9 percent while the general rate of inflation was 1.3 percent.[12] For example, the cost of Symbicort, a medication used to treat asthma and COPD, increased 46 percent, from $2,940 to $4,282.[13] See Figure 8.4[14] for an illustration related to prescription medication costs.
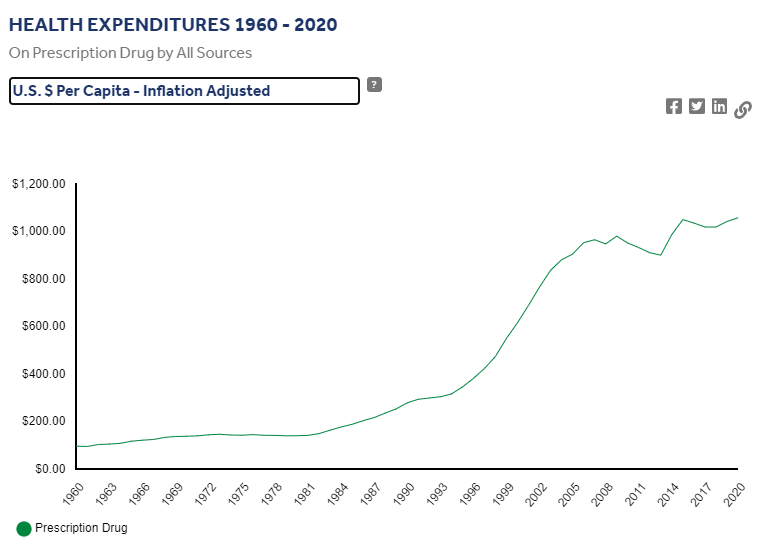
Although the majority of Americans have either public or private insurance that helps them pay for medications, increased medication prices result in higher health insurance premiums and higher taxpayer costs for the Medicare and Medicaid programs. Some insurance companies only cover approved formulary medications. As a result, national organizations like the American Association of Retired Persons (AARP) advocate for national policy changes, such as allowing Medicare to negotiate the prices of prescription medications with drug companies and allowing private insurance plans to have access to those lower prices.[15]
Many consumers find themselves tasked with the difficult decision of purchasing expensive medication or going without prescribed medication and paying for their families' housing and food. Nurses often become involved in case management activities when assisting clients to obtain medications they cannot afford. Nursing case management activities are discussed later in this chapter.
Affordable Care Act
The Patient Protection and Affordable Care Act (PPACA), also known as the Affordable Care Act (ACA) or Obamacare, was signed into law in 2010. The purpose of this legislation was to increase consumers' access to health care coverage and protect them from insurance practices that restricted care or significantly increased the cost of care. The ACA mandated health insurance coverage for employers and individuals. Employers were mandated to provide health care coverage based on the number of their employees, and individuals who were not covered through employer insurance plans were mandated to seek coverage through a newly created Marketplace. The Marketplace provides a central, website that offers three standard health insurance coverage levels to facilitate comparison by consumers. As a result of the ACA and associated Medicaid expansion, 32 million people had health care coverage in 2021.[16]
Key Provisions of the ACA
The ACA includes the following key provisions[17]:
- Insurers can no longer deny coverage or care for preexisting conditions like diabetes, asthma, and cancer.
- Young adults may remain on their parents’ insurance plans until they are 26 (even if they are married, financially independent, or not living with their parents).
- Health insurance plans cannot place annual or lifetime limits on coverage, except for nonessential exceptions, such as cosmetic procedures.
- Many preventive services must be provided, such as:
- Well-child visits, flu shots, and other common vaccines
- Screening tests for blood pressure and diabetes
- Diagnostic screening tests, such mammograms and colonoscopies
- Counseling services related to mental health and substance use
The ACA also provides an avenue for consumers to appeal insurance companies’ denials for care or payment of services and restricts situations in which an insurance carrier may cancel a policy.
Challenges to the ACA
Although the ACA has significantly increased the number of Americans with health insurance coverage, it continues to be debated. Debates focus on increased taxes, increased insurance premiums, and some people’s belief that mandated coverage is governmental intrusion on an individual’s rights. The Affordable Care Act has been challenged three times without success. In 2012 the U. S. Supreme Court upheld mandated coverage as a constitutional exercise of Congress’ taxing powers because it could be interpreted as an individual’s choice to maintain health insurance or pay a tax. However, in 2017 Congress set the penalty for failing to comply with the mandate at zero dollars after multiple attempts to repeal and replace the ACA. In June 2021 the U.S. Supreme Court rejected a third major challenge regarding the constitutionality of the ACA. In a 7-to-2 decision, the U.S. Supreme Court upheld the ACA based on the judgment that the states who brought forth the case did not prove damage to citizens because the fines for not having health coverage had been eliminated since the original legislation was passed.[18]
What to Expect Next
Given the Supreme Court’s recent decision regarding the ACA, it is expected the current administration will continue to advocate for the ACA and work towards making ACA tax credits permanent. Congress is also actively debating other legislative proposals to reduce health care costs, such as medication pricing reform and expanding Medicare eligibility age and benefits.[19]
Social Determinants of Health
Social Determinants of Health (SDOH) are the conditions in the environments where people live, learn, work, and play that affect a wide range of outcomes. SDOH include health care access and quality, neighborhood and environment, social and community context, economic stability, and education access and quality. These conditions have a major impact on people’s health and well-being, ultimately affecting national health care costs.[20]
SDOH directly impact individuals' health behaviors, their access to routine health care, and development of chronic disease. Yet, the United States spends a significantly lower percentage of its gross domestic product (GDP) on social services as compared to similar countries with better health outcomes.[21]
Healthy People 2030, established by the U.S. Department of Health and Human Services, identifies public health priorities to help individuals, organizations, and communities across the United States improve health and well-being over the next decade by addressing SDOH. One of Healthy People 2030’s goals states, “Create social, physical, and economic environments that promote attaining the full potential for health and well-being for all.”[22] Nurses act in many ways to address these priorities as they advocate for individuals, families, and communities.
Maria's Journey Through the Health Care System
Maria, a 45-year-old woman, lives in a low-income neighborhood in a large urban area. She works two part-time jobs to support her family of four and has limited access to health care due to financial constraints and transportation issues. Maria has been diagnosed with type 2 diabetes, and her health care outcomes are significantly influenced by various Social Determinants of Health (SDOH).
Maria's low income and unstable employment contribute to her inability to afford healthy food, medications, and regular medical check-ups. This economic instability exacerbates her diabetes, as she often skips doses of her medication to save money and cannot afford nutritious meals that would help manage her condition. The constant stress of making ends meet and providing for her family leads to increased cortisol levels, which can negatively impact her blood sugar control.
- How can Maria's financial stress impact her ability to manage her diabetes effectively?
2. What programs or policies could be implemented to assist individuals like Maria in managing their health care costs?
Maria has limited knowledge about diabetes management due to a lack of education and access to health information. This impacts her ability to understand and implement lifestyle changes or adhere to treatment plans. With limited education, Maria struggles to find better-paying jobs that could provide health insurance and more financial stability.
3. In what ways can improved health literacy impact Maria's diabetes management?
4. What community resources could be made available to enhance health education for individuals in Maria's situation?
The availability of health care services in Maria’s neighborhood is limited, with long wait times and fewer specialists. This results in delayed diagnoses and treatments for her diabetes-related complications. Maria lacks comprehensive health insurance, making it difficult for her to access primary and specialist care. High out-of-pocket costs deter her from seeking regular medical attention.
5. How does the lack of accessible health care services affect Maria's long-term health outcomes?
6. What are some potential solutions to improve health care access in underserved areas?
Maria lives in a food desert with limited access to fresh fruits and vegetables. She often relies on inexpensive, processed foods that worsen her diabetes. Public transportation in Maria’s area is unreliable, making it challenging for her to attend medical appointments. This lack of transportation contributes to missed check-ups and unmanaged diabetes.
7. How does living in a food desert affect Maria's ability to manage her diabetes?
8. What transportation initiatives could help individuals like Maria access healthcare services more easily?
Maria has a limited social network and lacks support from friends and family, which is crucial for managing a chronic condition like diabetes. This isolation can lead to depression and further neglect of her health. Living in a high-crime area, Maria feels unsafe walking outside for exercise, which is essential for diabetes management. This sedentary lifestyle negatively affects her health outcomes.
9. How does a lack of social support contribute to Maria's health challenges?
10. What community programs or interventions could be implemented to enhance social support and safety in high-crime areas?
- CMS.gov. (2020, December 16). National health expenditure data - historical. Centers for Medicare & Medicaid Services. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/NationalHealthAccountsHistorical ↵
- CMS.gov. (2020, December 16). National health expenditure data - historical. Centers for Medicare & Medicaid Services. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/NationalHealthAccountsHistorical ↵
- “Health_Care_Cost_as_Percentage_of_GDP.png” by Delphi234 is licensed under CC0 1.0 ↵
- Bush, M. (2018). Addressing the root cause: Rising health care costs and social determinants of health. North Carolina Medical Journal, 79(1), 26-29. https://doi.org/10.18043/ncm.79.1.26 ↵
- Schreck, R. I. (2020, March). Overview of health care financing. Merck Manual Consumer Version. https://www.merckmanuals.com/home/fundamentals/financial-issues-in-health-care/overview-of-health-care-financing ↵
- Agency for Healthcare Research and Quality. (n.d.). Elderly. https://www.ahrq.gov/topics/elderly.html ↵
- “graying-america-aging-nation.jpg” by U.S. Census Bureau is in the Public Domain ↵
- Agency for Healthcare Research and Quality. (n.d.). Elderly. https://www.ahrq.gov/topics/elderly.html ↵
- Neumann, P. J., & Weinstein, M. C. (1991). The diffusion of new technology: Costs and benefits to health care. In Institute of Medicine (US) Committee on Technological Innovation in Medicine, Gelijns, A. C., & Halm, E. A. (Eds.). The changing economics of medical technology. National Academies Press. https://www.ncbi.nlm.nih.gov/books/NBK234309/ ↵
- “49458105981_fe87fd521c_o.jpg” by Wonderlane is licensed under CC BY 2.0 ↵
- Neumann, P. J., & Weinstein, M. C. (1991). The diffusion of new technology: Costs and benefits to health care. In Institute of Medicine (US) Committee on Technological Innovation in Medicine, Gelijns, A. C., & Halm, E. A. (Eds.). The changing economics of medical technology. National Academies Press. https://www.ncbi.nlm.nih.gov/books/NBK234309/ ↵
- Bunis, D. (2021, June 7). Prescription drug price increases continue to outpace inflation. AARP. https://www.aarp.org/politics-society/advocacy/info-2021/prescription-price-increase-report.html ↵
- Bunis, D. (2021, June 7). Prescription drug price increases continue to outpace inflation. AARP. https://www.aarp.org/politics-society/advocacy/info-2021/prescription-price-increase-report.html ↵
- Peterson_KFF Health Systems Tracker. (n.d.). Health expenditures 1960-2020. https://www.healthsystemtracker.org/health-spending-explorer/?outputType=%24pop-adjusted&serviceType%5B0%5D=prescriptionDrug&serviceType%5B1%5D=hospitals&serviceType%5B2%5D=allTypes&sourceOfFunds%5B0%5D=allSources&tab=0&yearCompare%5B0%5D=%2A&yearCompare%5B1%5D=%2A&yearRange%5B0%5D=%2A&yearRange%5B1%5D=%2A&yearSingle=%2A&yearType=range ↵
- Bunis, D. (2021, June 7). Prescription drug price increases continue to outpace inflation. AARP. https://www.aarp.org/politics-society/advocacy/info-2021/prescription-price-increase-report.html ↵
- HealthCare.gov. Insurance marketplace. https://www.healthcare.gov/subscribe/? gclid=Cj0KCQjwiqWHBhD2ARIsAPCDzamNRkS3URx_uUvJGdpX15DrZnVbBadXbPmOjBBlLyjtZBn7cLei6WEaAl8GEALw_wcB&gclsrc=aw.ds ↵
- HHS.gov. About the Affordable Care Act. U.S. Department of Health & Human Services. https://www.hhs.gov/healthcare/about-the-aca/index.html ↵
- K&L Gates LLP, Carnevale, A., Hamscho, V., Lawless, T., & Sha Page, K. (2021, June 21). The Affordable Care Act survives Supreme Court challenge: What happens next? JD Supra. https://www.jdsupra.com/legalnews/the-affordable-care-act-survives-3115372/ ↵
- K&L Gates LLP, Carnevale, A., Hamscho, V., Lawless, T., & Sha Page, K. (2021, June 21). The Affordable Care Act survives Supreme Court challenge: What happens next? JD Supra. https://www.jdsupra.com/legalnews/the-affordable-care-act-survives-3115372/ ↵
- Healthy People 2030. (n.d.). Social determinants of health. U.S. Department of Health and Human Services. https://health.gov/healthypeople/objectives-and-data/social-determinants-health ↵
- Bush, M. (2018). Addressing the root cause: Rising health care costs and social determinants of health. North Carolina Medical Journal. 79(1), 26-29. https://www.ncmedicaljournal.com/content/79/1/26 ↵
- Healthy People 2030. (n.d.). Social determinants of health. U.S. Department of Health and Human Services. https://health.gov/healthypeople/objectives-and-data/social-determinants-health ↵
Factors that are inherent to the characteristics and needs of the population
External elements that impact healthcare costs.
Legislation enacted in 2010 to increase consumers' access to health care coverage and protect them from insurance practices that restricted care or significantly increased the cost of care.

