Open Resources for Nursing (Open RN)
Skeleton
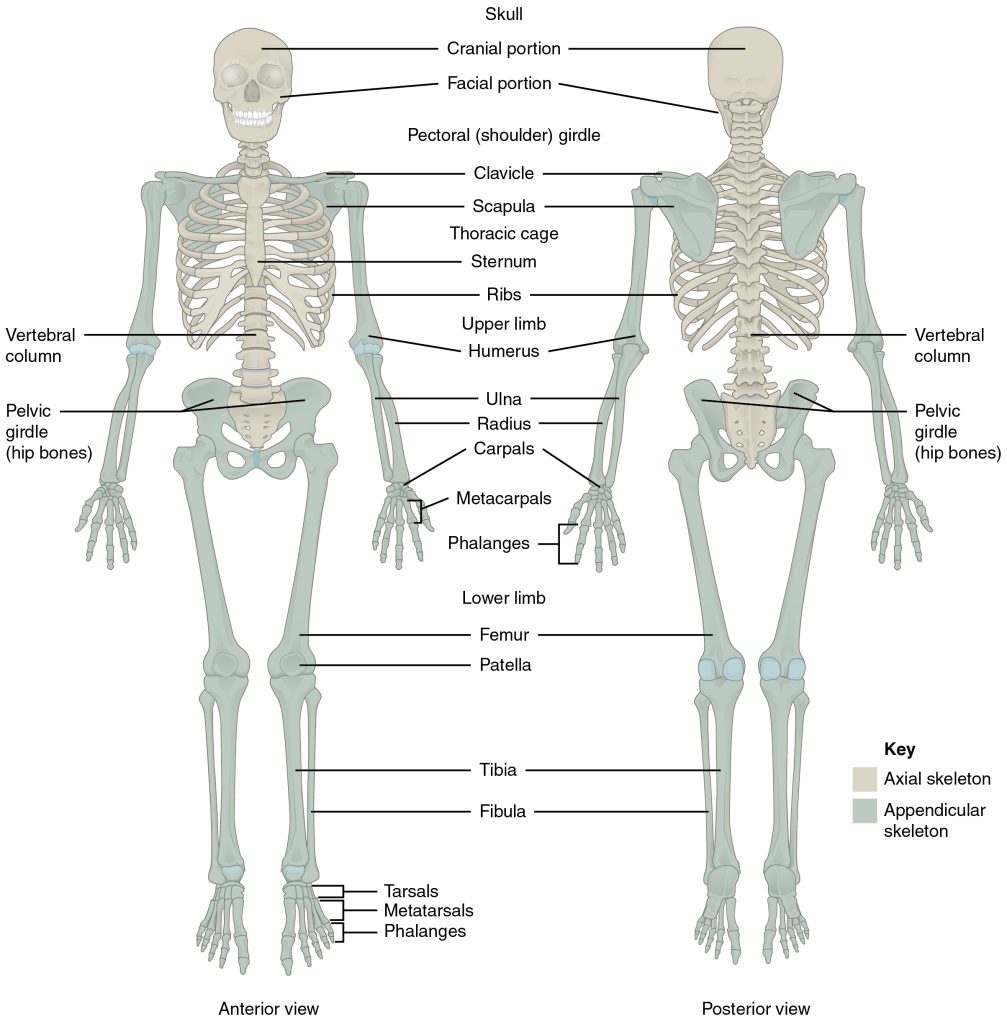
The skeleton is composed of 206 bones that provide the internal supporting structure of the body. See Figure 13.1[1] for an illustration of the major bones in the body. The bones of the lower limbs are adapted for weight-bearing support, stability, and walking. The upper limbs are highly mobile with large range of movements, along with the ability to easily manipulate objects with our hands and opposable thumbs.[2]
For additional information about the bones in the body, visit the OpenStax Anatomy and Physiology book.
Many different bones are connected together by ligaments. Most bones of the skill are held together by sutures, a narrow fibrous joint. Ligaments are strong bands of fibrous connective tissue that strengthen and support the joint by anchoring the bones together and preventing their separation. Ligaments allow for normal movements of a joint while also limiting the range of these motions to prevent excessive or abnormal joint movements.[3]
Muscles
There are three types of muscle tissue: skeletal muscle, cardiac muscle, and smooth muscle. Skeletal muscles are attached to the skeleton and produce movement, assist in maintaining posture, protect internal organs, and generate body heat. Skeletal muscles are voluntary, meaning a person is able to consciously control them, but they also depend on signals from the nervous system to work properly. Other types of muscles are involuntary and are controlled by the autonomic nervous system, such as the smooth muscle within our bronchioles.[4] Cardiac muscles are located only in the heart and are involuntary muscles that the autonomic nervous system controls. Smooth muscle makes up the organs, blood vessels, digestive tract, skin, and other areas and is controlled by the autonomic nervous system.
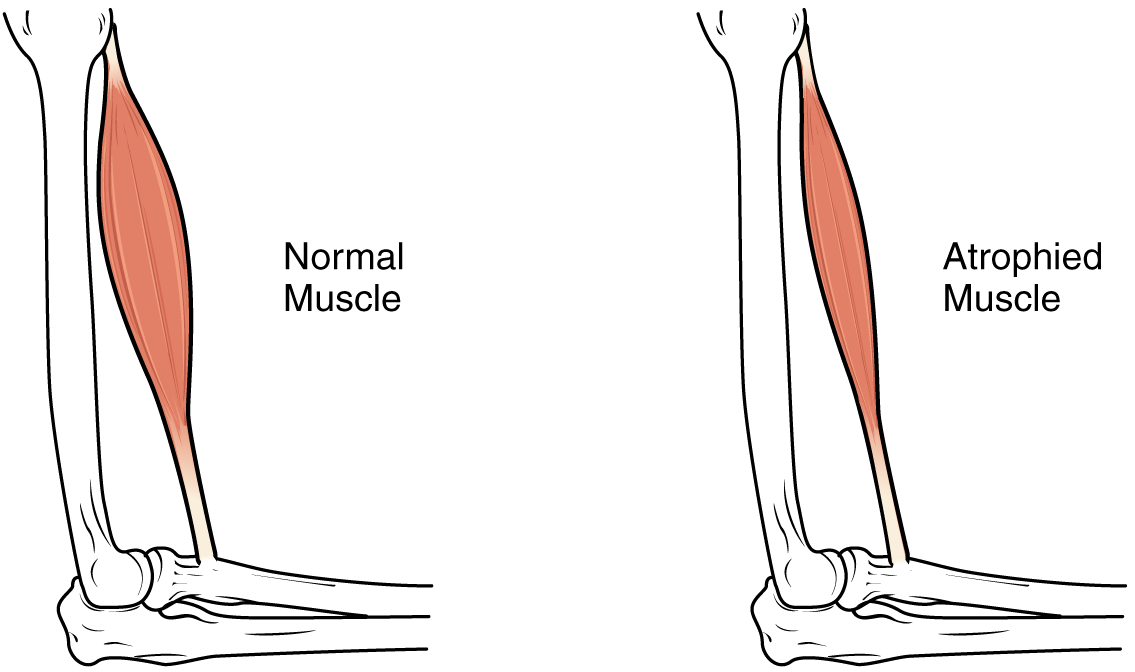
See Figure 13.2[5] for an illustration of skeletal muscle.
To move the skeleton, the tension created by the contraction of the skeletal muscles is transferred to the tendons, strong bands of dense, regular connective tissue that connect muscles to bones.[6]
For additional information about skeletal muscles, visit the OpenStax Anatomy and Physiology book.

Muscle Atrophy
Muscle atrophy is the thinning or loss of muscle tissue. See Figure 13.3[7] for an image of muscle atrophy. There are three types of muscle atrophy: physiologic, pathologic, and neurogenic.
Physiologic atrophy is caused by not using the muscles and can often be reversed with exercise and improved nutrition. People who are most affected by physiologic atrophy are those who:
- Have seated jobs, health problems that limit movement, or decreased activity levels
- Are bedridden
- Cannot move their limbs because of stroke or other brain disease
- Are in a place that lacks gravity, such as during space flights
Pathologic atrophy is seen with aging, starvation, and adverse effects of long-term use of corticosteroids. Neurogenic atrophy is the most severe type of muscle atrophy. It can be from an injured or diseased nerve that connects to the muscle. Examples of neurogenic atrophy are spinal cord injuries and polio.[8]
Although physiologic atrophy due to disuse can often be reversed with exercise, muscle atrophy caused by age is more complex. The effects of age-related atrophy are especially pronounced in people who are sedentary because the loss of muscle results in functional impairments such as trouble with walking, balance, and posture. These functional impairments can cause decreased quality of life and injuries due to falls.[9]
Joints
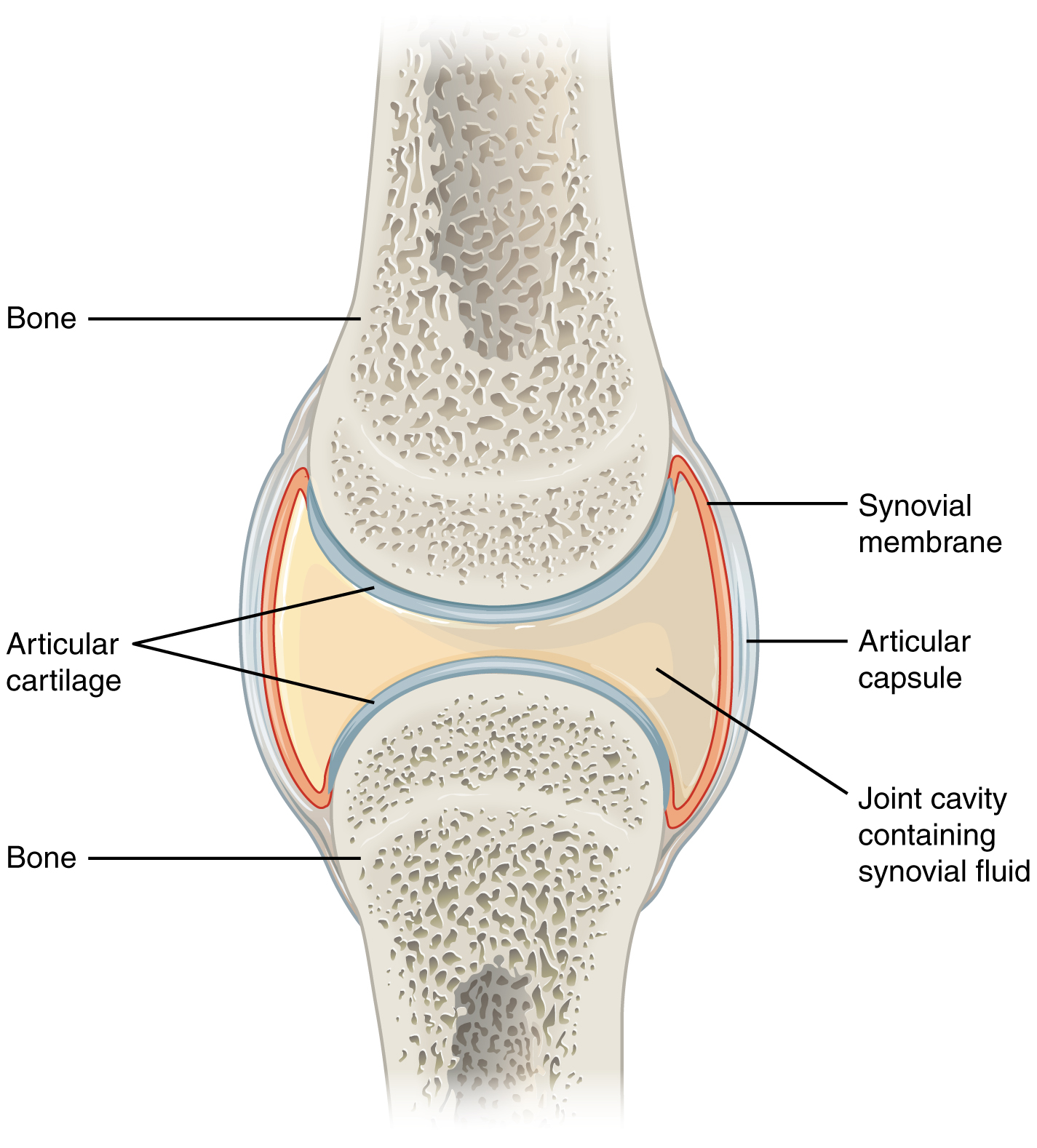
Joints are the location where bones come together. Many joints allow for movement between the bones. Synovial joints are the most common type of joint in the body. Synovial joints have a fluid-filled joint cavity where the articulating surfaces of the bones contact and move smoothly against each other. See Figure 13.4[10] for an illustration of a synovial joint. Articular cartilage is smooth, white tissue that covers the ends of bones where they come together and allows the bones to glide over each other with very little friction. Articular cartilage can be damaged by injury or normal wear and tear. Lining the inner surface of the articular capsule is a thin synovial membrane. The cells of this membrane secrete synovial fluid, a thick, slimy fluid that provides lubrication to further reduce friction between the bones of the joint.[11]
Types of Synovial Joints
There are six types of synovial joints. See Figure 13.5[12] for an illustration of the types of synovial joints. Some joints are relatively immobile but stable. Other joints have more freedom of movement but are at greater risk of injury. For example, the hinge joint of the knee allows flexion and extension, whereas the ball and socket joint of the hip and shoulder allows flexion, extension, abduction, adduction, and rotation. The knee, hip, and shoulder joints are commonly injured and are discussed in more detail in the following subsections.

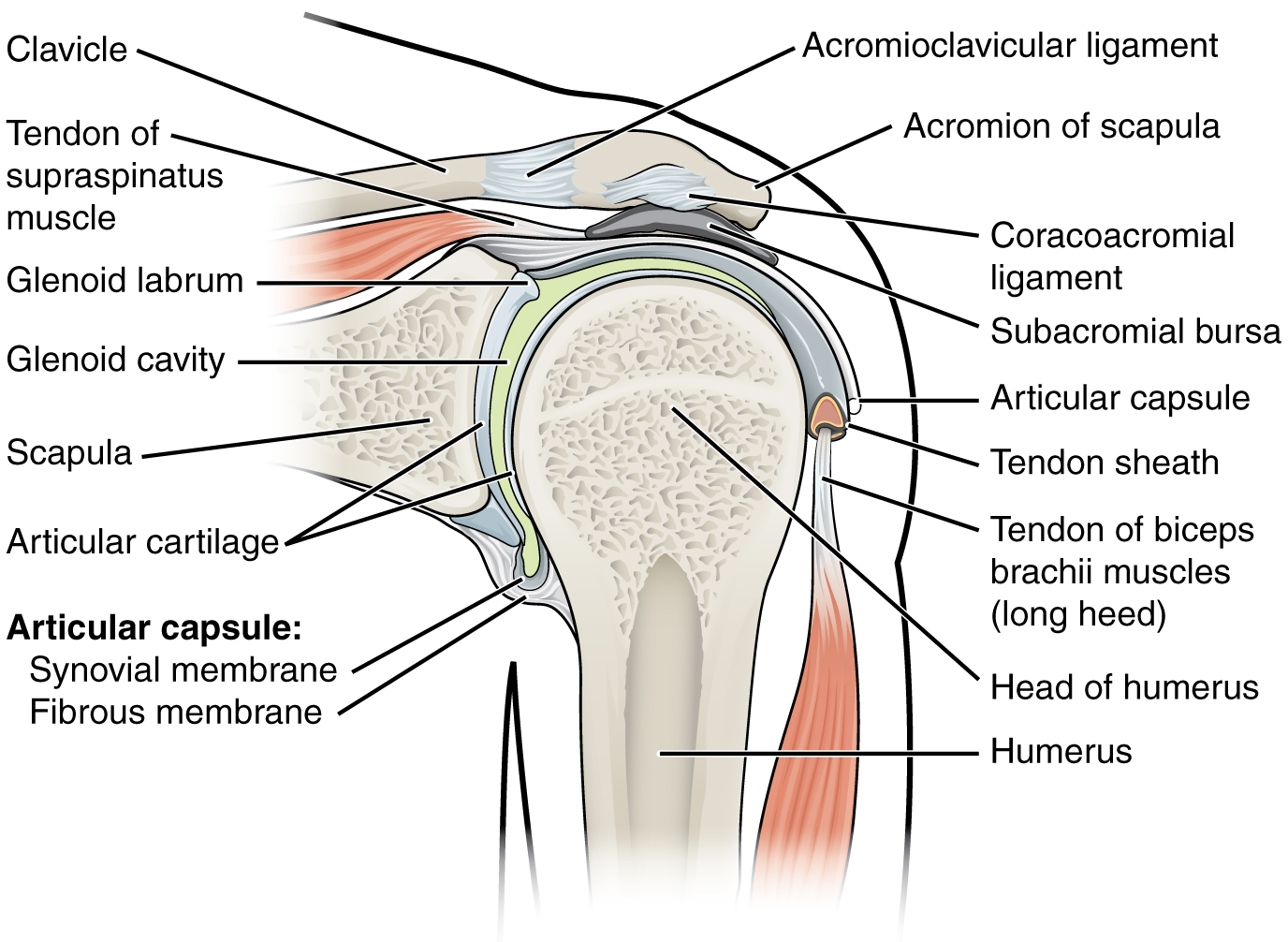
Shoulder Joint
The shoulder joint is a ball-and-socket joint formed by the articulation between the head of the humerus and the glenoid cavity of the scapula. This joint has the largest range of motion of any joint in the body. See Figure 13.6[13] to review the anatomy of the shoulder joint. Injuries to the shoulder joint are common, especially during repetitive abductive use of the upper limb such as during throwing, swimming, or racquet sports.[14]
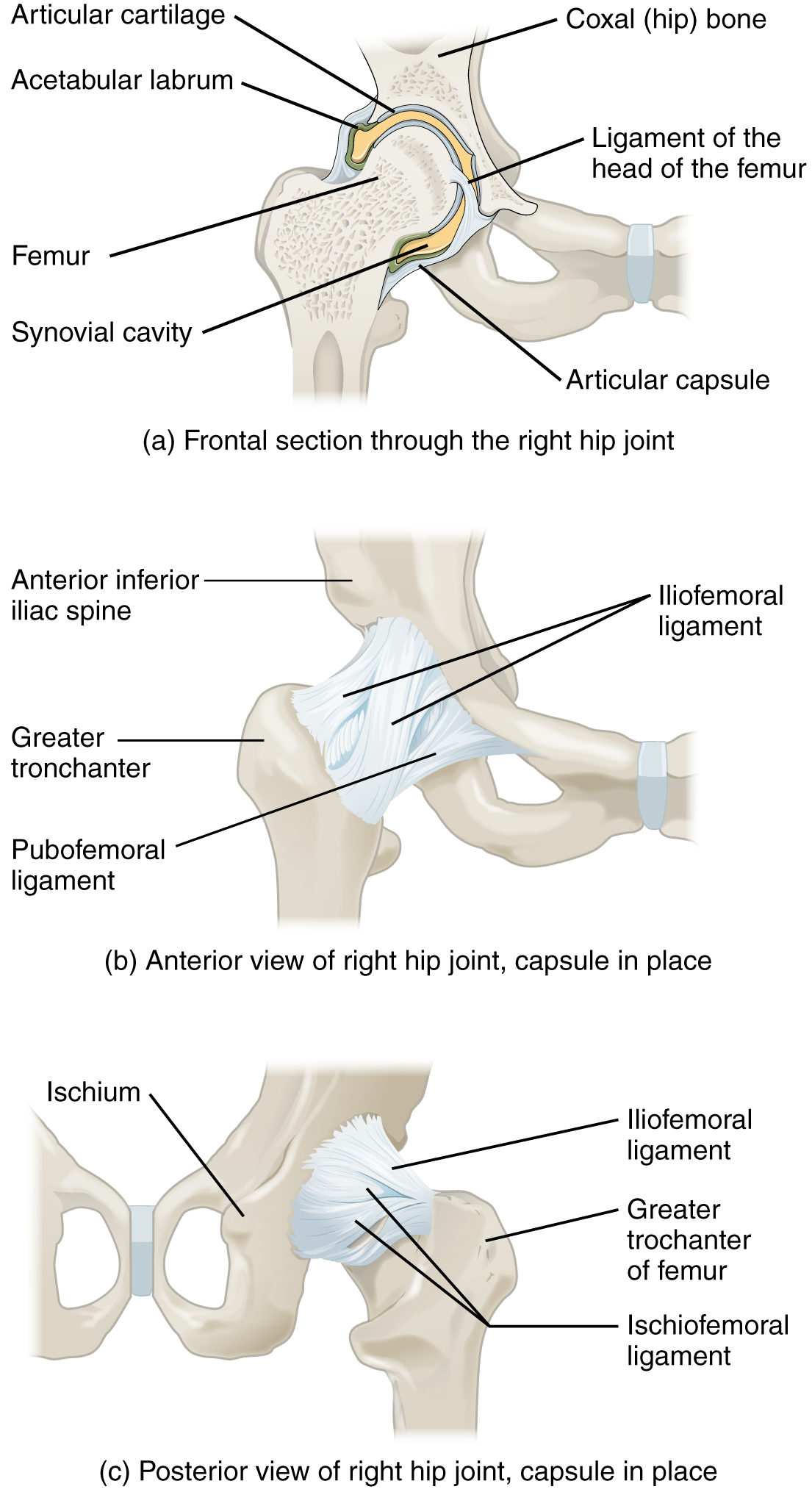
Hip Joint
The hip joint is a ball-and-socket joint between the head of the femur and the acetabulum of the hip bone. The hip carries the weight of the body and thus requires strength and stability during standing and walking.[15]
See Figure 13.7[16] for an illustration of the hip joint.
A common hip injury in older adults, often referred to as a “broken hip,” is actually a fracture of the head of the femur. Hip fractures are commonly caused by falls.[17]
See more information about hip fractures under the “Common Musculoskeletal Conditions” section.
Knee Joint
The knee functions as a hinge joint that allows flexion and extension of the leg. In addition, some rotation of the leg is available. See Figure 13.8[18] for an illustration of the knee joint. The knee is vulnerable to injuries associated with hyperextension, twisting, or blows to the medial or lateral side of the joint, particularly while weight-bearing.[19]
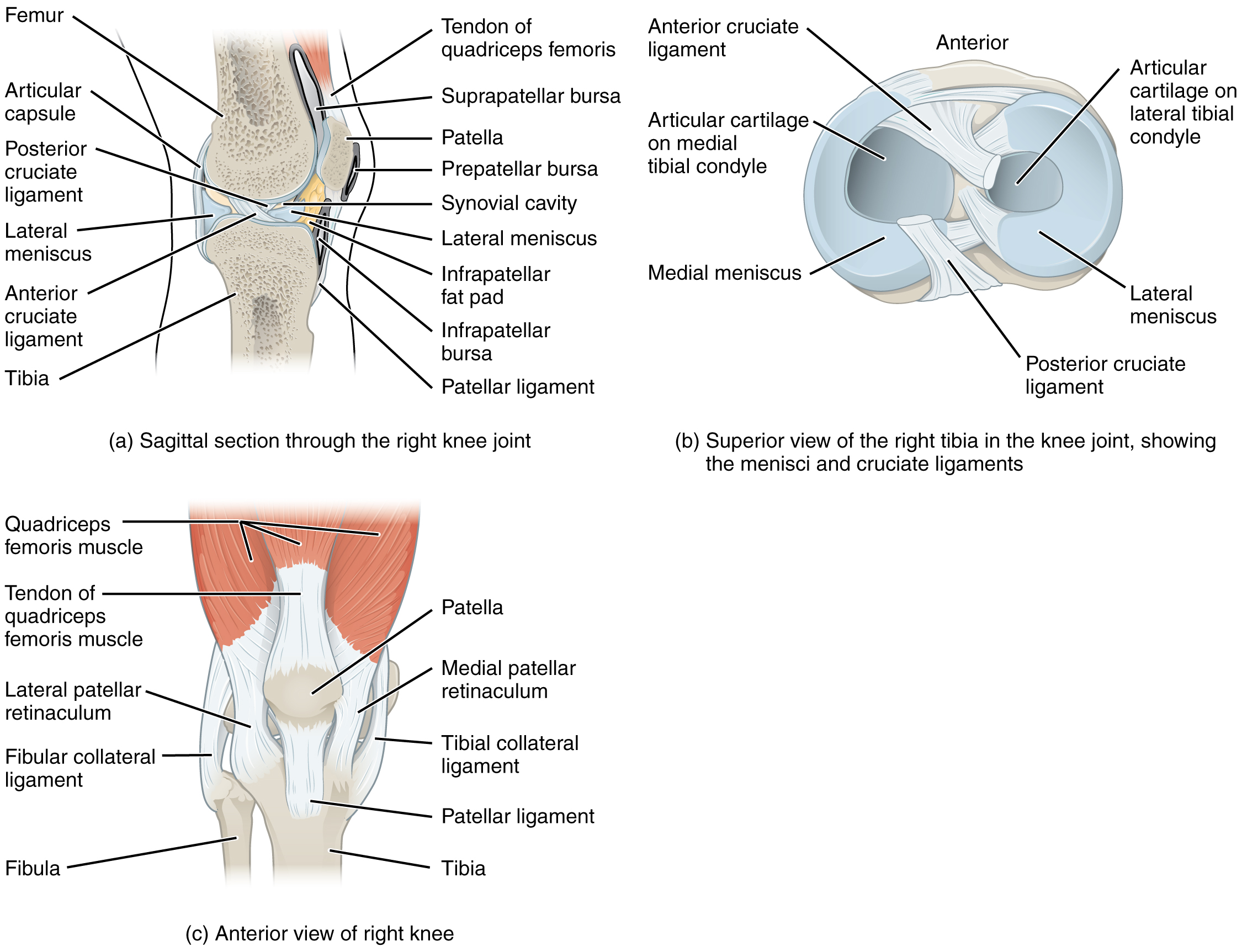
The knee joint has multiple ligaments that provide support, especially in the extended position. On the outside of the knee joint are the lateral collateral, medial collateral, and tibial collateral ligaments. The lateral collateral ligament is on the lateral side of the knee and spans from the lateral side of the femur to the head of the fibula. The medial collateral ligament runs from the medial side of the femur to the medial tibia. The tibial collateral ligament crosses the knee and is attached to the articular capsule and to the medial meniscus. In the fully extended knee position, both collateral ligaments are taut and stabilize the knee by preventing side-to-side or rotational motions between the femur and tibia.[20]
Inside the knee joint are the anterior cruciate ligament and posterior cruciate ligament. These ligaments are anchored inferiorly to the tibia and run diagonally upward to attach to the inner aspect of a femoral condyle. The posterior cruciate ligament supports the knee when it is flexed and weight-bearing such as when walking downhill. The anterior cruciate ligament becomes tight when the knee is extended and resists hyperextension.[21]
The patella is a bone incorporated into the tendon of the quadriceps muscle, the large muscle of the anterior thigh. The patella protects the quadriceps tendon from friction against the distal femur. Continuing from the patella to the anterior tibia just below the knee is the patellar ligament. Acting via the patella and patellar ligament, the quadriceps is a powerful muscle that extends the leg at the knee and provides support and stabilization for the knee joint.
Located between the articulating surfaces of the femur and tibia are two articular discs, the medial meniscus and lateral meniscus. Each meniscus is a C-shaped fibrocartilage that provides padding between the bones.[22]
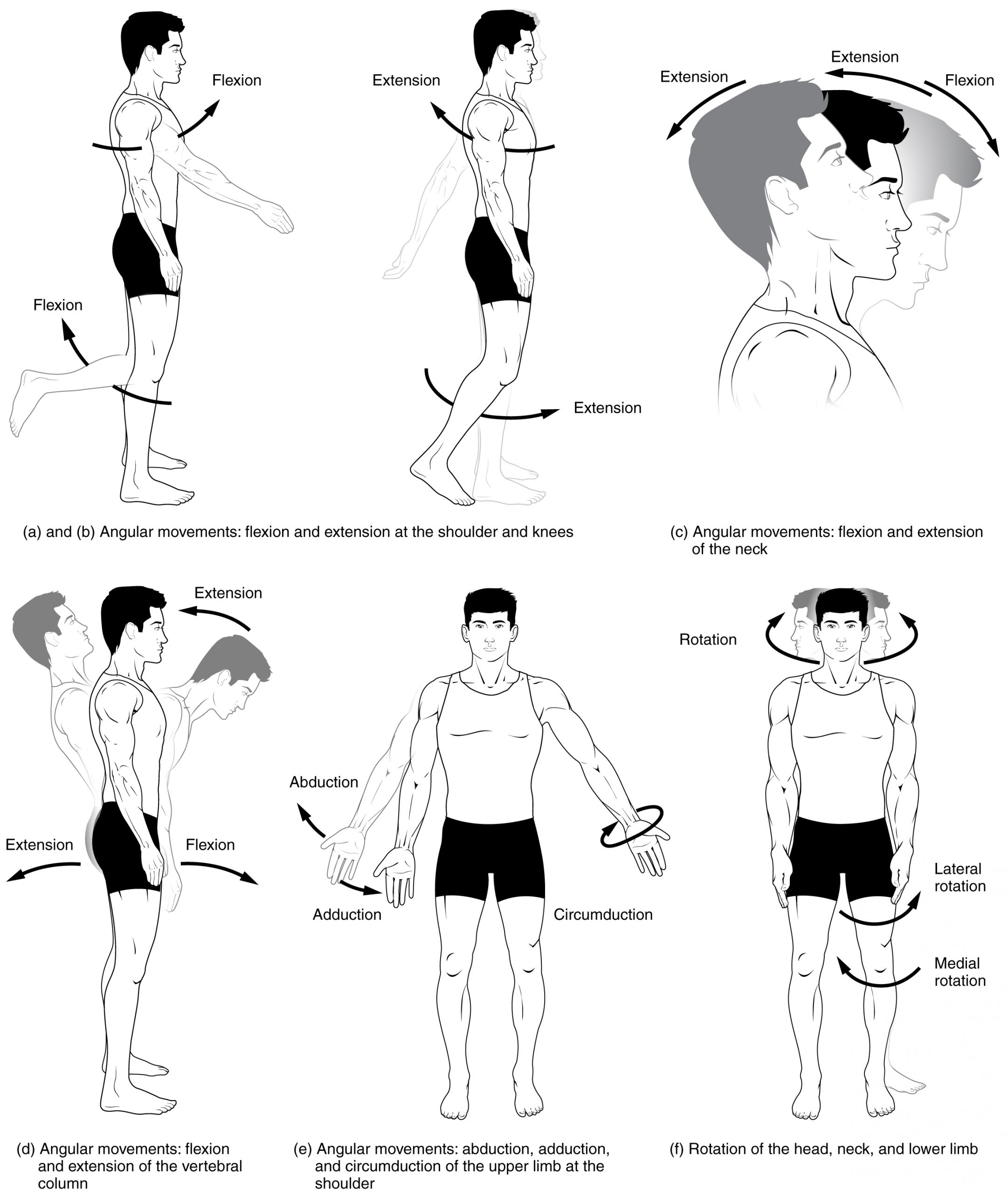
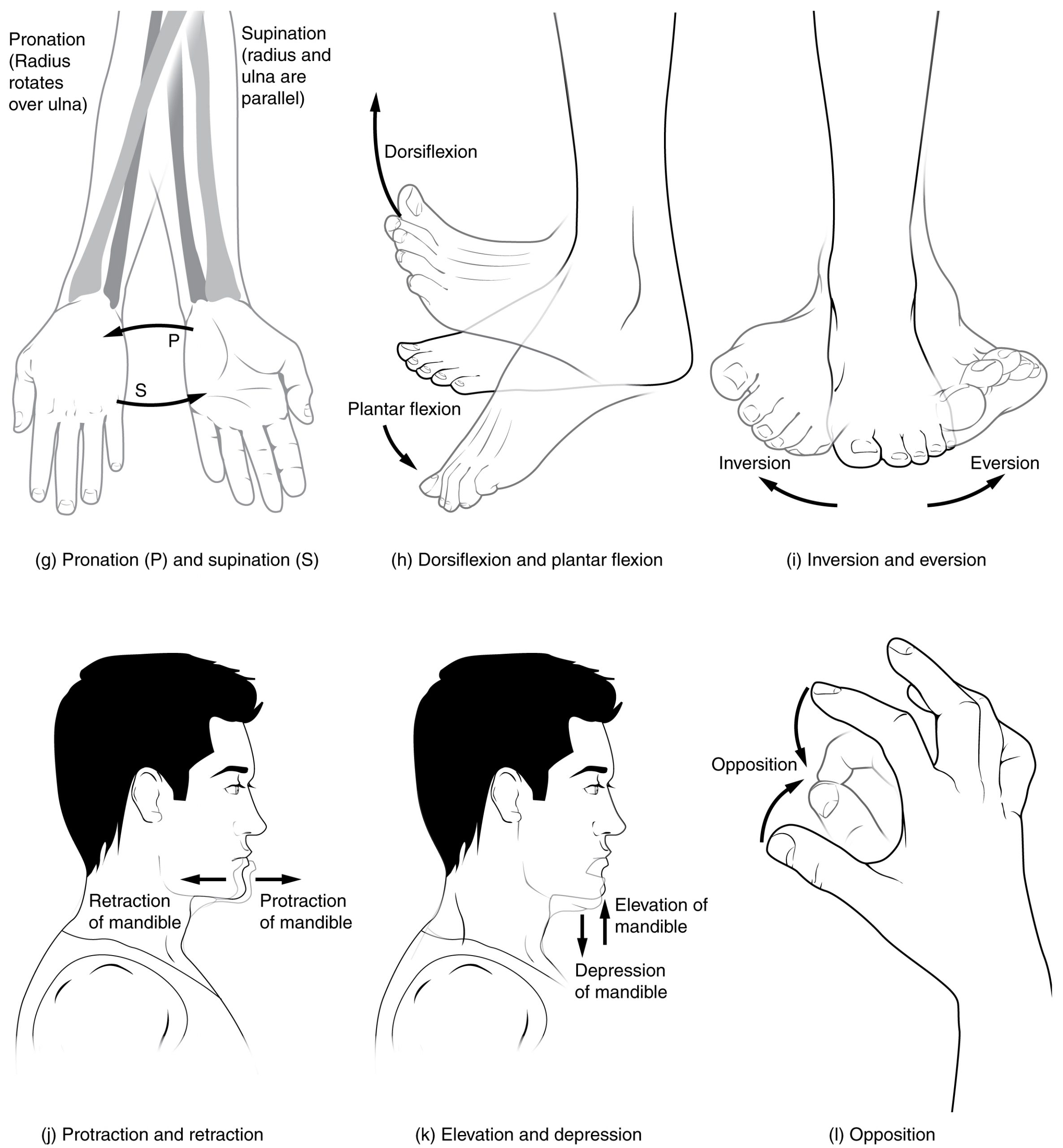
Joint Movements
Several movements may be performed by synovial joints. Abduction is the movement away from the midline of the body. Adduction is the movement toward the middle line of the body. Extension is the straightening of limbs (increase in angle) at a joint. Flexion is bending the limbs (reduction of angle) at a joint. Rotation is a circular movement around a fixed point. See Figures 13.9[23] and 13.10[24] for images of the types of movements of different joints in the body.
Joint Sounds
Sounds that occur as joints are moving are often referred to as crepitus. There are many different types of sounds that can occur as a joint moves, and patients may describe these sounds as popping, snapping, catching, clicking, crunching, cracking, crackling, creaking, grinding, grating, and clunking. There are several potential causes of these noises such as bursting of tiny bubbles in the synovial fluid, snapping of ligaments, or a disease condition. While assessing joints, be aware that joint noises are common during activity and are usually painless and harmless, but if they are associated with an injury or are accompanied by pain or swelling, they should be reported to the health care provider for follow-up.[25]
View a supplementary video from Physitutors called Why Your Knees Crack | Joint Crepitations.[26]
- “701 Axial Skeleton-01.jpg” by OpenStax is licensed under CC BY 3.0 ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/preface ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- “1105 Anterior and Posterior Views of Muscles.jpg” by OpenStax is licensed under CC BY-SA 4.0 ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- “1025 Atrophy.png” by OpenStax is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/10-6-exercise-and-muscle-performance ↵
- A.D.A.M. Medical Encyclopedia [Internet]. Atlanta (GA): A.D.A.M., Inc.; c1997-2020. Muscle atrophy; [updated 2020, Sep 16; cited 2020, Sep 18]. https://medlineplus.gov/ency/article/003188.htm ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- “907_Synovial_Joints.jpg” by OpenStax is licensed under CC BY-SA 3.0 ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- “909 Types of Synovial Joints.jpg” by OpenStax is licensed under CC BY 3.0 ↵
- “914 Shoulder Joint.jpg” by OpenStax is licensed under CC BY 3.0 ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- “916 Hip Joint.jpg” by OpenStax is licensed under CC BY 3.0 ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- “917 Knee Joint.jpg” by OpenStax is licensed under CC BY 3.0 ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- “Body Movements I.jpg” by Tonye Ogele CNX is licensed under CC BY-SA 3.0 ↵
- “Body Movements II.jpg” by Tonye Ogele CNX is licensed under CC BY-SA 3.0 ↵
- Song, S. J., Park, C. H., Liang, H., & Kim, S. J. (2018). Noise around the knee. Clinics in Orthopedic Surgery, 10(1), 1-8. https://dx.doi.org/10.4055%2Fcios.2018.10.1.1 ↵
- Physitutors. (2017, March 25). Why your knees crack | Joint crepitations [Video]. YouTube. All rights reserved. https://youtu.be/NQOZZgh5z8I ↵
Drain management systems are commonly used during postoperative surgical management to remove drainage, prevent infection, and enhance wound healing. A drain may be superficial in the skin or deep in an organ, duct, or cavity, such as a hematoma. A patient may have several drains depending on the extent and type of surgery. A closed system uses a vacuum system to withdraw fluids and collect them in a reservoir. Closed systems must be emptied and drainage measured routinely according to agency policy.
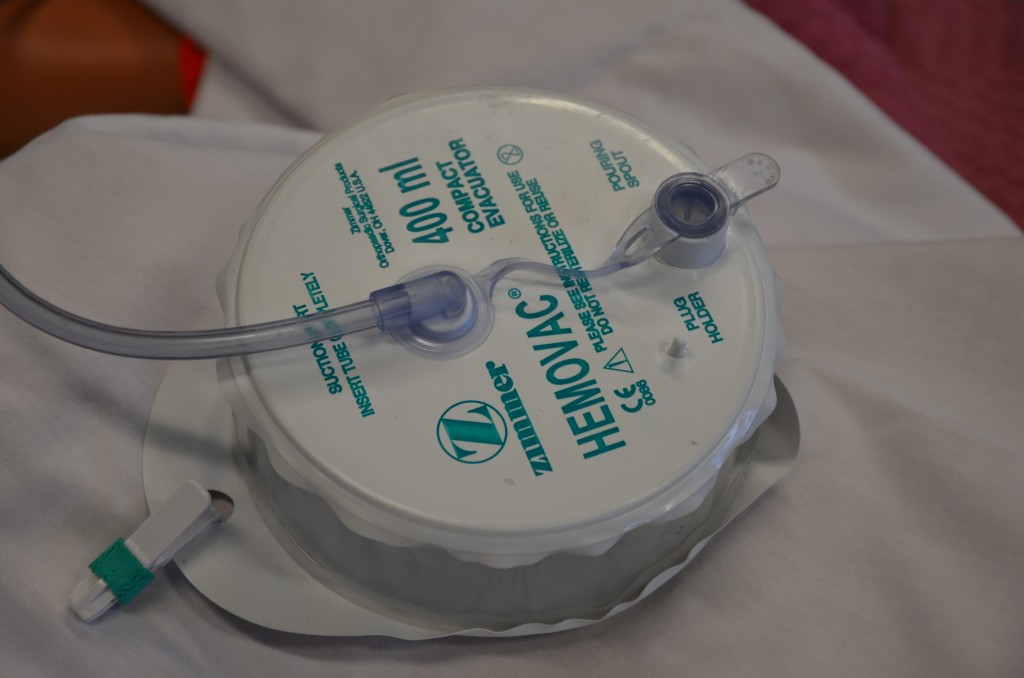
Drainage tubes contain perforations to allow fluid to drain from the surgical wound site. The drainage is collected in a closed sterile collection system/reservoir, such as a Hemovac or Jackson-Pratt. The amount of drainage varies depending on location and type of surgery. A Hemovac drain (see Figure 20.38[1]) can hold up to 500 mL of drainage. A Jackson-Pratt (JP) drain (see Figure 20.39[2]) is used for smaller amounts of drainage, usually ranging from 25 to 50 mL. Drains are usually sutured to the skin to prevent accidental removal, and the drainage site is covered with a sterile dressing. The site and drain should be checked periodically throughout the shift to ensure the drain is functioning effectively and that no leaking is occurring.

Checklist for Drain Management
Use the checklist below to review the steps for completion of “Drain Management."
Steps
Disclaimer: Always review and follow agency policy regarding this specific skill.
- Gather supplies: drainage measurement container, nonsterile gloves, waterproof pad, and alcohol swab.
- Perform safety steps:
- Perform hand hygiene.
- Check the room for transmission-based precautions.
- Introduce yourself, your role, the purpose of your visit, and an estimate of the time it will take.
- Confirm patient ID using two patient identifiers (e.g., name and date of birth).
- Explain the process to the patient and ask if they have any questions.
- Be organized and systematic.
- Use appropriate listening and questioning skills.
- Listen and attend to patient cues.
- Ensure the patient’s privacy and dignity.
- Assess ABCs.
- Apply nonsterile gloves and goggles or face shield according to agency policy to reduce the transmission of microorganisms and protect against an accidental body fluid exposure.
- Maintaining a sterile technique, remove the plug from the pouring spout as indicated on the drain:
- Open the plug pointing away from your face to avoid an accidental splash of contaminated fluid.
- Maintain the plug’s sterility.
- Notice that the vacuum will be broken, and the reservoir (drainage collection system) will expand.
- Gently tilt the opening of the reservoir toward the measuring container and pour out the drainage away from you to prevent exposure to body fluids. Do not touch the measuring container with the reservoir opening.
- Place the drainage container on the bed or hard surface, tilt it away from your face, and compress the drain to flatten it with one hand to remove all the air before closing the spout to establish the vacuum system.
- Cleanse the plug with the alcohol swab per agency policy. Maintaining sterility, place the plug back into the pour spout of the drainage system to establish the vacuum system of the drainage system.
- Secure the device onto the patient's gown using a safety pin; check patency and placement of tube. Ensure that enough slack is present in tubing and that the reservoir hangs lower than the wound. Proper placement of the reservoir allows gravity to facilitate wound drainage. Providing enough slack to accommodate patient movement prevents tension of the drainage system and pulling on the tubing and insertion site.
- Note the characteristics of the drainage: color, consistency, odor, and amount. Drainage counts as patient fluid output and must be documented on the patient chart per agency policy.
- Monitor and empty drains frequently in the postoperative period to reduce the weight of the reservoir and to assess drainage.
- Remove gloves and perform hand hygiene.
- Assist the patient to a comfortable position, ask if they have any questions, and thank them for their time.
- Ensure safety measures when leaving the room:
- CALL LIGHT: Within reach
- BED: Low and locked (in lowest position and brakes on)
- SIDE RAILS: Secured
- TABLE: Within reach
- ROOM: Risk-free for falls (scan room and clear any obstacles)
- Document the procedure and assessment findings according to agency policy. Report any unusual findings or concerns to the health care provider. If the amount of drainage increases or changes, notify the appropriate health care provider according to agency policy.
- If the amount of drainage significantly decreases, the drain may be ready to be assessed and removed.
- Notify required health care provider if the wound appears infected.
- Record the number of drains if there is more than one and record each one separately.
Learning Activities
(Answers to "Learning Activities" can be found in the "Answer Key" at the end of the book. Answers to interactive activity elements will be provided within the element as immediate feedback.)
Mr. Jones is a 76-year-old patient admitted to the medical surgical floor with complications of a nonhealing foot ulcer. Mr. Jones has a history of diabetes, hypertension, and COPD. He has a BMI of 29. His daily medications include metformin, Lisinopril, and prednisone. His wife has recently passed away and he lives alone.
- Based upon what is known about Mr. Jones, what factors might be contributing to his nonhealing wound?
- What other factors that influence wound healing might be important to assess with Mr. Jones?
Test your clinical judgment with an NCLEX Next Generation-style question: Chapter 20, Assignment 1.
Test your clinical judgment with an NCLEX Next Generation-style question: Chapter 20, Assignment 2.
Test your clinical judgment with an NCLEX Next Generation-style question: Chapter 20, Assignment 3.
Learning Activities
(Answers to "Learning Activities" can be found in the "Answer Key" at the end of the book. Answers to interactive activity elements will be provided within the element as immediate feedback.)
Mr. Jones is a 76-year-old patient admitted to the medical surgical floor with complications of a nonhealing foot ulcer. Mr. Jones has a history of diabetes, hypertension, and COPD. He has a BMI of 29. His daily medications include metformin, Lisinopril, and prednisone. His wife has recently passed away and he lives alone.
- Based upon what is known about Mr. Jones, what factors might be contributing to his nonhealing wound?
- What other factors that influence wound healing might be important to assess with Mr. Jones?
Test your clinical judgment with an NCLEX Next Generation-style question: Chapter 20, Assignment 1.
Test your clinical judgment with an NCLEX Next Generation-style question: Chapter 20, Assignment 2.
Test your clinical judgment with an NCLEX Next Generation-style question: Chapter 20, Assignment 3.
Angiogenesis: The development of new capillaries in a wound base.
Arterial ulcers: Ulcers caused by lack of blood flow and oxygenation to tissues and typically occur in the distal areas of the body such as the feet, heels, and toes.
Debridement: The removal of nonviable tissue in a wound.
Dehiscence: The separation of the edges of a surgical wound.
Diabetic ulcers: Ulcers that typically develop on the plantar aspect of the feet and toes of patients with diabetes due to lack of sensation of pressure or injury.
Ecchymosis: Bruising that occurs when small veins and capillaries under the skin break.
Edema: Swelling.
Epithelialization: The development of new epidermis and granulation tissue.
Erythema: Redness.
Eschar: Dark brown/black, dry, thick, and leathery dead tissue in a wound base that must be removed for healing to occur.
Exudate: Fluid that oozes out of a wound; also commonly called pus.
Granulation tissue: New connective tissue in a wound base with fragile, thin-walled capillaries that must be protected.
Hematoma: An area of blood that collects outside of larger blood vessels.
Hemosiderin staining: Dark-colored discoloration of the lower legs due to blood pooling.
Hemostasis phase: The first phase of wound healing that occurs immediately after skin injury. Blood vessels constrict and clotting factors are activated.
Induration: Area of hardened tissue.
Inflammatory phase: The second phase of wound healing when vasodilation occurs so that white blood cells in the bloodstream can move into the wound to start cleaning the wound bed.
Maceration: The softening and wasting away of skin due to excess fluid.
Maturation phase: The final phase of wound healing as collagen continues to be created to strengthen the wound, causing scar tissue.
Necrotic: Black tissue color due to tissue death from lack of oxygenation to the area.
Nonblanchable erythema: Skin redness that does not turn white when pressure is applied.
Osteomyelitis: Bone infection.
Peripheral neuropathy: A condition that causes decreased sensation of pain and pressure, typically in the lower extremities.
Periwound: The skin around the outer edges of a wound.
Pressure injuries: Localized damage to the skin or underlying soft tissue, usually over a bony prominence, as a result of intense and prolonged pressure in combination with shear.[3]
Primary intention: Wound healing that occurs with surgical incisions or clean-edged lacerations that are closed with sutures, staples, or surgical glue.
Proliferative phase: The third phase of wound healing that includes epithelialization, angiogenesis, collagen formation, and contraction.
Purulent drainage: Wound exudate that is thick and opaque and can be tan, yellow, green, or brown in color. It is never considered normal in a wound, and new purulent drainage should always be reported to the health care provider.
Sanguineous drainage: Wound drainage that is fresh bleeding.
Secondary intention: Wound healing that occurs when the edges of a wound cannot be approximated (brought together), so the wound fills in from the bottom up by the production of granulation tissue. Examples of wounds that heal by secondary intention are pressure injuries and chainsaw injuries.
Serosanguinous drainage: Wound exudate contains serous drainage with small amounts of blood present.
Serous drainage: Wound drainage that is clear, thin, watery plasma. It is considered normal in minimal amounts during the inflammatory stage of wound healing.
Shear: A mechanical force that occurs when tissue layers move over the top of each other, causing blood vessels to stretch and break as they pass through the subcutaneous tissue.
Skin tears: Wounds caused by mechanical forces, typically in the nonelastic skin of older adults.
Slough: Inflammatory exudate that is light yellow, soft, and moist and must be removed for wound healing to occur.
Tertiary intention: Wound healing that occurs when a wound must remain open or has been reopened, often due to severe infection.
Tunneling: Passageways underneath the surface of the skin that extend from a wound and can take twists and turns.
Undermining: A condition that occurs in wounds when the tissue under the wound edges becomes eroded, resulting in a pocket beneath the skin at the wound's edge.
Unstageable: Occurs when slough or eschar obscures the wound so that tissue loss cannot be assessed.
Venous insufficiency: A medical condition where the veins in the legs do not adequately send blood back to the heart, resulting in a pooling of fluids in the legs that can cause venous ulcers.
Venous ulcers: Ulcers caused by the pooling of fluid in the veins of the lower legs when the valves are not working properly, causing fluid to seep out, macerate the skin, and cause an ulcer.
Wound vac: A device used with special foam dressings and suctioning to remove fluid and decrease air pressure around a wound to assist in healing.
Angiogenesis: The development of new capillaries in a wound base.
Arterial ulcers: Ulcers caused by lack of blood flow and oxygenation to tissues and typically occur in the distal areas of the body such as the feet, heels, and toes.
Debridement: The removal of nonviable tissue in a wound.
Dehiscence: The separation of the edges of a surgical wound.
Diabetic ulcers: Ulcers that typically develop on the plantar aspect of the feet and toes of patients with diabetes due to lack of sensation of pressure or injury.
Ecchymosis: Bruising that occurs when small veins and capillaries under the skin break.
Edema: Swelling.
Epithelialization: The development of new epidermis and granulation tissue.
Erythema: Redness.
Eschar: Dark brown/black, dry, thick, and leathery dead tissue in a wound base that must be removed for healing to occur.
Exudate: Fluid that oozes out of a wound; also commonly called pus.
Granulation tissue: New connective tissue in a wound base with fragile, thin-walled capillaries that must be protected.
Hematoma: An area of blood that collects outside of larger blood vessels.
Hemosiderin staining: Dark-colored discoloration of the lower legs due to blood pooling.
Hemostasis phase: The first phase of wound healing that occurs immediately after skin injury. Blood vessels constrict and clotting factors are activated.
Induration: Area of hardened tissue.
Inflammatory phase: The second phase of wound healing when vasodilation occurs so that white blood cells in the bloodstream can move into the wound to start cleaning the wound bed.
Maceration: The softening and wasting away of skin due to excess fluid.
Maturation phase: The final phase of wound healing as collagen continues to be created to strengthen the wound, causing scar tissue.
Necrotic: Black tissue color due to tissue death from lack of oxygenation to the area.
Nonblanchable erythema: Skin redness that does not turn white when pressure is applied.
Osteomyelitis: Bone infection.
Peripheral neuropathy: A condition that causes decreased sensation of pain and pressure, typically in the lower extremities.
Periwound: The skin around the outer edges of a wound.
Pressure injuries: Localized damage to the skin or underlying soft tissue, usually over a bony prominence, as a result of intense and prolonged pressure in combination with shear.[4]
Primary intention: Wound healing that occurs with surgical incisions or clean-edged lacerations that are closed with sutures, staples, or surgical glue.
Proliferative phase: The third phase of wound healing that includes epithelialization, angiogenesis, collagen formation, and contraction.
Purulent drainage: Wound exudate that is thick and opaque and can be tan, yellow, green, or brown in color. It is never considered normal in a wound, and new purulent drainage should always be reported to the health care provider.
Sanguineous drainage: Wound drainage that is fresh bleeding.
Secondary intention: Wound healing that occurs when the edges of a wound cannot be approximated (brought together), so the wound fills in from the bottom up by the production of granulation tissue. Examples of wounds that heal by secondary intention are pressure injuries and chainsaw injuries.
Serosanguinous drainage: Wound exudate contains serous drainage with small amounts of blood present.
Serous drainage: Wound drainage that is clear, thin, watery plasma. It is considered normal in minimal amounts during the inflammatory stage of wound healing.
Shear: A mechanical force that occurs when tissue layers move over the top of each other, causing blood vessels to stretch and break as they pass through the subcutaneous tissue.
Skin tears: Wounds caused by mechanical forces, typically in the nonelastic skin of older adults.
Slough: Inflammatory exudate that is light yellow, soft, and moist and must be removed for wound healing to occur.
Tertiary intention: Wound healing that occurs when a wound must remain open or has been reopened, often due to severe infection.
Tunneling: Passageways underneath the surface of the skin that extend from a wound and can take twists and turns.
Undermining: A condition that occurs in wounds when the tissue under the wound edges becomes eroded, resulting in a pocket beneath the skin at the wound's edge.
Unstageable: Occurs when slough or eschar obscures the wound so that tissue loss cannot be assessed.
Venous insufficiency: A medical condition where the veins in the legs do not adequately send blood back to the heart, resulting in a pooling of fluids in the legs that can cause venous ulcers.
Venous ulcers: Ulcers caused by the pooling of fluid in the veins of the lower legs when the valves are not working properly, causing fluid to seep out, macerate the skin, and cause an ulcer.
Wound vac: A device used with special foam dressings and suctioning to remove fluid and decrease air pressure around a wound to assist in healing.
Learning Objectives
- Perform urinary catheterization, ostomy care, and urine specimen collection
- Manage urinary catheters to prevent complications
- Maintain aseptic or sterile technique
- Explain procedure to patient
- Modify assessment techniques to reflect variations across the life span
- Document actions and observations
- Recognize and report significant deviations from norms
Elimination is a basic human function of excreting waste through the bowel and urinary system. The process of elimination depends on many variables and intricate processes that occur within the body. Many medical conditions and surgeries can adversely affect the processes of elimination, so nurses must facilitate their patients’ bowel and urinary elimination as needed. Common nursing interventions related to facilitating elimination include inserting and managing urinary catheters, obtaining urine specimens, caring for ostomies, providing patient education to promote healthy elimination, and preventing complications. In this chapter, we will discuss the technical skills used to support bowel and bladder function, as well as the application of the nursing process while doing so.
Learning Objectives
- Perform urinary catheterization, ostomy care, and urine specimen collection
- Manage urinary catheters to prevent complications
- Maintain aseptic or sterile technique
- Explain procedure to patient
- Modify assessment techniques to reflect variations across the life span
- Document actions and observations
- Recognize and report significant deviations from norms
Elimination is a basic human function of excreting waste through the bowel and urinary system. The process of elimination depends on many variables and intricate processes that occur within the body. Many medical conditions and surgeries can adversely affect the processes of elimination, so nurses must facilitate their patients’ bowel and urinary elimination as needed. Common nursing interventions related to facilitating elimination include inserting and managing urinary catheters, obtaining urine specimens, caring for ostomies, providing patient education to promote healthy elimination, and preventing complications. In this chapter, we will discuss the technical skills used to support bowel and bladder function, as well as the application of the nursing process while doing so.
Blood-tinged mucus secretions from the lungs.
The first stage of wound healing when clotting factors are released to form clots to stop the bleeding.

