Open Resources for Nursing (Open RN)
The scope of practice regarding a nurse’s ability to legally dispense and administer medication is based on each state’s Nurse Practice Act. Registered Nurses (RNs) and Licensed Practical Nurses (LPNs/LVNs) may legally administer medications that are prescribed by a health care provider, such as a physician, nurse practitioner, or physician’s assistant. Prescriptions are “orders, interventions, remedies, or treatments ordered or directed by an authorized primary health care provider.”[1]
For more information about the state Nurse Practice Act, visit the “Legal/Ethical” chapter in Open RN Nursing Pharmacology.
Types of Orders
Prescriptions are often referred to as orders in clinical practice. There are several types of orders, such as routine orders, PRN orders, standing orders, one-time orders, STAT orders, and titration orders.
- A routine order is a prescription that is followed until another order cancels it. An example of a routine order is “Lisinopril 10 mg PO daily.”
- A PRN order is a prescription for medication to be administered when it is requested by, or as needed, by the patient. PRN orders are typically administered based on patient symptoms, such as pain, nausea, or itching. An example of a PRN order for pain medication is “Acetaminophen 500 mg PO every 4-6 hours as needed for pain.”
- A standing order is also referred to in practice as an “order set” or a “protocol.” Standing orders are standardized prescriptions for nurses to implement to any patient in clearly defined circumstances without the need to initially notify a provider. An example of a standing order set/protocol for patients visiting an urgent care clinic reporting chest pain is to immediately administer four chewable aspirin, establish intravenous (IV) access, and obtain an electrocardiogram (ECG).
- A one-time order is a prescription for a medication to be administered only once. An example of a one-time order is a prescription for an IV dose of antibiotics to be administered immediately prior to surgery.
- A STAT order is a one-time order that is administered without delay due to the urgency of the circumstances. An example of a STAT order is “Benadryl 50 mg PO stat” for a patient having an allergic reaction.
- A titration order is an order in which the medication dose is either progressively increased or decreased by the nurse in response to the patient’s status. Titration orders are typically used for patients in critical care as defined by agency policy. The Joint Commission requires titration orders to include the medication name, medication route, initial rate of infusion (dose/unit of time), incremental units to which the rate or dose can be increased or decreased, how often the rate or dose can be changed, the maximum rate or dose of infusion, and the objective clinical measure to be used to guide changes. An example of a titration order is “Norepinephrine 2-12 micrograms/min, start at 2 mcg/min and titrate upward by 1 mcg/min every 5 minutes with continual blood pressure monitoring until systolic blood pressure >90 mm Hg.”
Components of a Medication Order
According to the Centers for Medicare & Medicaid Services, all orders for the administration of drugs and biologicals must contain the following information[2]:
- Name of the patient
- Age or date of birth
- Date and time of the order
- Drug name
- Dose, frequency, and route
- Name/Signature of the prescriber
- Weight of the patient to facilitate dose calculation when applicable. (Note that dose calculations are based on metric weight: kilograms for children/adults or grams for newborns)
- Dose calculation requirements, when applicable
- Exact strength or concentration, when applicable
- Quantity and/or duration of the prescription, when applicable
- Specific instructions for use, when applicable
When reviewing a medication order, the nurse must ensure these components are included in the prescription before administering the medication. If a pertinent piece of information is not included, the nurse must contact the prescribing provider to clarify and correct the order.
Drug Name
The name of the drug may be ordered by the generic name or brand name. The generic name is considered the safest method to use and allows for substitution of various brand medications by the pharmacist.
Dose
The dosage of a drug is prescribed using either the metric or the household system. The metric system is the most commonly accepted system internationally. Examples of standard dosage are 5 mL (milliliters) or 1 teaspoon. Standard abbreviations of metric measurement are frequently used regarding the dosage, such as mg (milligram), kg (kilogram), mL (milliliter), mcg (microgram), or L (liter). However, it is considered safe practice to avoid other abbreviations and include the full words in prescriptions to avoid errors. In fact, several abbreviations have been deemed unsafe by the Joint Commission and have been put on a “do not use” list. See the box below to view The Joint Commission’s “Do Not Use List” and the Institute of Safe Medication Practices’ (ISMP) list of abbreviations to avoid. If a dosage is unclear or written in a confusing manner in a prescription, it is always best to clarify the order with the prescribing provider before administering the medication.
Frequency
Frequency in prescriptions is indicated by how many times a day the medication is to be administered or how often it is to be administered in hours or minutes. Examples of frequency include verbiage such as once daily, twice daily, three times daily, four times daily, every 30 minutes, every hour, every four hours, or every eight hours. Medication times are typically indicated using military time (i.e., using a 24-hour clock). For example, 11 p.m. is indicated as “2300.” Read more about military time in the “Math Calculations” chapter.
Some types of medications may be ordered “around the clock (ATC).” An around-the-clock frequency order indicates they should be administered at regular time intervals, such as every six hours, to maintain consistent levels of the drug in the patient’s bloodstream. For example, pain medications administered at end of life are often prescribed ATC instead of PRN (as needed) to maintain optimal pain relief.
Route of Administration
Common routes of administration and standard abbreviations include the following:
- Oral (PO) – the patient swallows a tablet or capsule
- Sublingual (SL) – applied under the tongue
- Enteral (NG or PEG) – administered via a tube directly into the GI tract
- Rectal (PR) – administered via rectal suppository
- Inhalation (INH) – the patient breathes in medication from an inhaler
- Intramuscular (IM) – administered via an injection into a muscle
- Subcutaneous – administered via injection into the fat tissue beneath the skin (Note that “subcutaneous” is on ISMP’s recommended list of abbreviations to avoid due to common errors.)
- Transdermal (TD) – administered by applying a patch on the skin
For more information about routes of administration and considerations regarding absorption, visit the “Kinetics and Dynamics” chapter in Open RN Nursing Pharmacology.
Provider Name/Signature
The signature of the prescribing provider is required on the order and can be electronic or handwritten. Verbal orders from a prescriber are not recommended but may be permitted in some agencies for urgent situations. Verbal orders require the nurse to “repeat back” the order to the prescriber for confirmation.
Rights of Medication Administration
Each year in the United States, 7,000 to 9,000 people die as a result of a medication error. Hundreds of thousands of other patients experience adverse reactions or other complications related to a medication. The total cost of caring for patients with medication-associated errors exceeds $40 billion each year. In addition to the monetary cost, patients experience psychological and physical pain and suffering as a result of medication errors.[3] Nurses play a vital role in reducing the number of medication errors that occur by verifying several rights of medication.
The Centers for Medicare & Medicaid Services requires nurses to verify specific information prior to the administration of medication to avoid errors, referred to as verifying the rights of medication administration.[4] These rights of medication administration are the vital last safety check by nurses to prevent errors in the chain of medication administration that includes the prescribing provider, the pharmacist, the nurse, and the patient.
It is important to remember that if a medication error occurs resulting in harm to a patient, a nurse can be held liable even if “just following orders.” It is absolutely vital for nurses to use critical thinking and clinical judgment to ensure each medication is safe for each specific patient before administering it. The consequences of liability resulting from a medication error can range from being charged with negligence in a court of law, to losing one’s job, to losing one’s nursing license.
The six rights of medication administration must be verified by the nurse at least three times before administering a medication to a patient. These six rights include the following:
- Right Patient
- Right Drug
- Right Dose
- Right Time
- Right Route[5]
- Right Documentation
Recent literature indicates that up to ten rights should be completed as part of a safe medication administration process. These additional rights include Right History and Assessment, Right Drug Interactions, Right to Refuse, and Right Education and Information. Information for each of these rights is further described below.[6],[7]
Right Patient
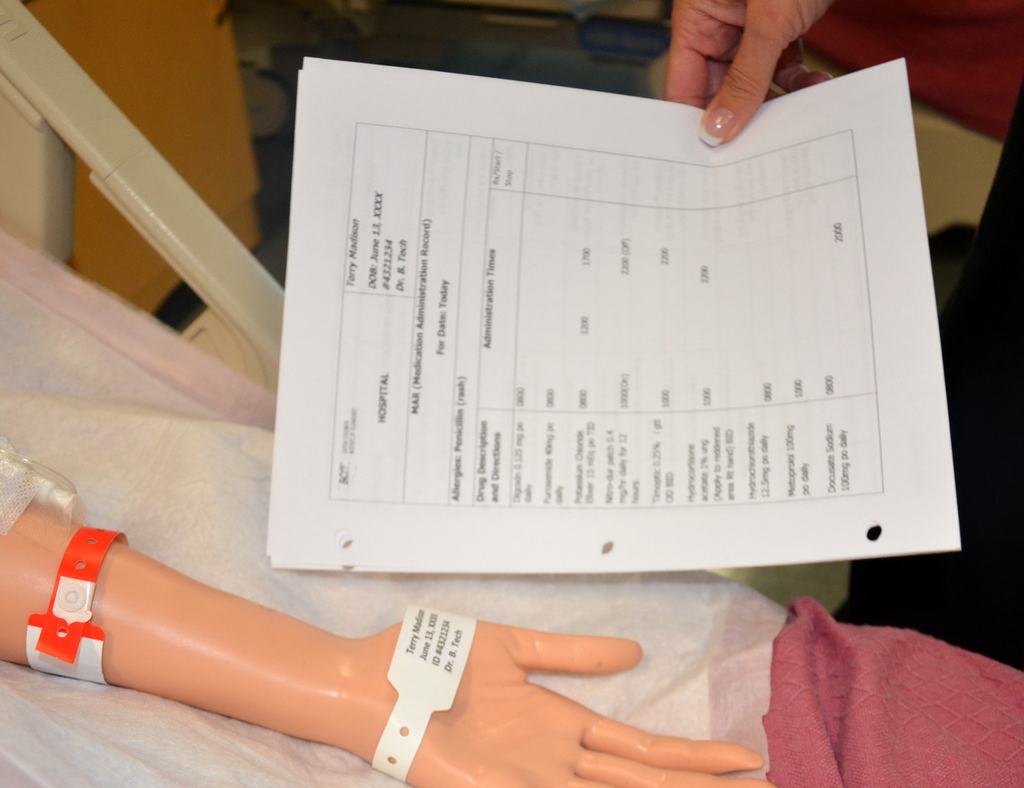
Acceptable patient identifiers include, but are not limited to, the patient’s full name, an identification number assigned by the hospital, or date of birth. A patient’s room number must never be used as an identifier because a patient may change rooms. Identifiers must be confirmed by the patient wristband, patient identification card, patient statement (when possible), or other means outlined in the agency policy such as a patient picture included on the MAR. The nurse must confirm the patient’s identification matches the medication administration record (MAR) and medication label prior to administration to ensure that the medication is being given to the correct patient.[8] See Figure 15.1[9] for an illustration of the nurse verifying the patient’s identify by scanning their identification band and asking for their date of birth. See Figure 15.2[10] for a close-up image of a patient identification wristband.
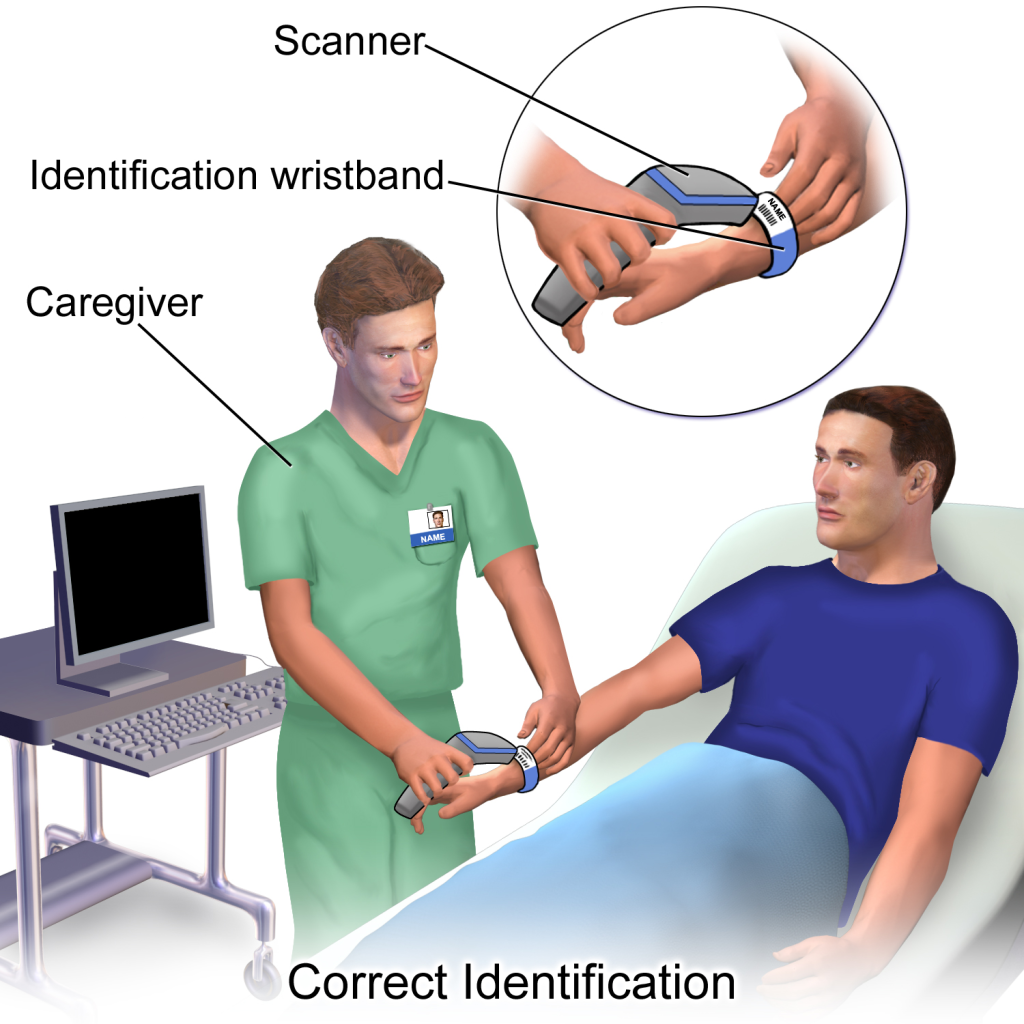

If barcode scanning is used in an agency, this scanning is not intended to take the place of confirming two patient identifiers but is intended to add another layer of safety to the medication administration process. The National Patient Safety Goals established by The Joint Commission state that whenever administering patient medications, at least two patient identifiers should be used.[11]
Right Drug
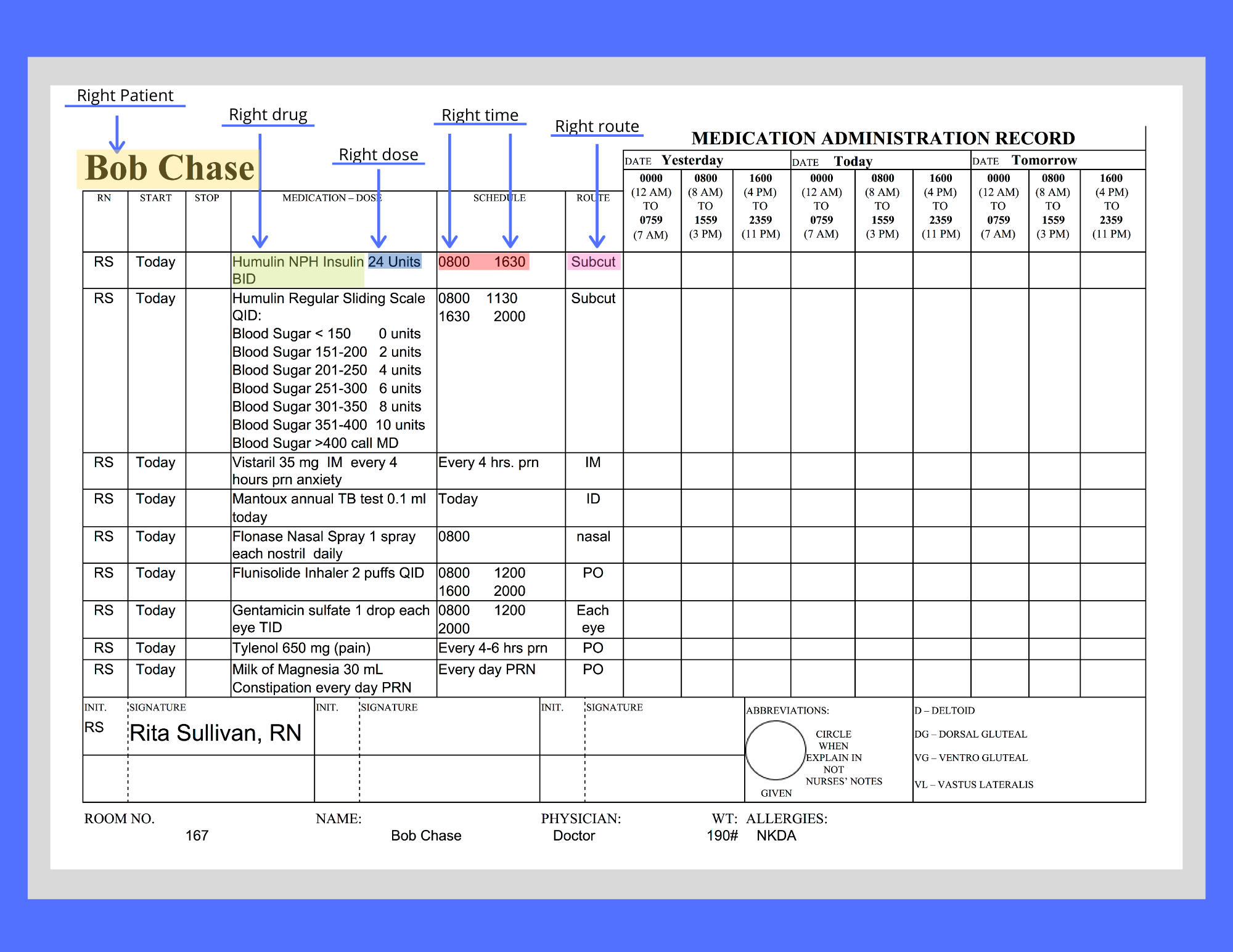
During this step, the nurse ensures the medication to be administered to the patient matches the order or Medication Administration Record (MAR) and that the patient does not have a documented allergy to it. Also, check the expiration date of the medication.[12] The Medication Administration Record (MAR), or eMAR, an electronic medical record, is a specific type of documentation found in a patient’s chart. See Figure 15.3[13] for an image of an MAR and its components. Beware of look-alike and sound-alike medication names, as well as high-alert medications that bear a heightened risk of causing significant patient harm if they are used in error. The nurse should also be aware of what medication can be crushed and those that cannot be crushed. Read more information about these concerns using the box below.
View the ISMP Frequently Confused Medication List.
View a PDF of the ISMP High-Alert Medications List.
View the ISMP Do Not Crush List.
Right Dose
During this step, the nurse ensures the dosage of the medication matches the prescribed dose, verifies the correct dosage range for the age and medical status of the patient, and also confirms that the prescription itself does not reflect an unsafe dosage level (i.e., a dose that is too high or too low).[14] For example, medication errors commonly occur in children, who typically receive a lower dose of medication than an adult. Medication errors also commonly occur in older patients who have existing kidney or liver disease and are unable to metabolize or excrete typical doses of medications.
Right Time and Frequency
During this step, the nurse verifies adherence to the prescribed frequency and scheduled time of administration of the medication.[15] This step is especially important when PRN medications are administered because it is up to the nurse to verify the time of the previous dose and compare it to the ordered frequency.
Medications should be administered on time whenever possible. However, when multiple patients are scheduled to receive multiple medications at the same time, this goal of timeliness can be challenging. Most facilities have a policy that medications can be given within a range of 30 minutes before or 30 minutes after the medication is scheduled. For example, a medication ordered for 0800 could be administered anytime between 0730 and 0830. However, some medications must be given at their specific ordered time due to pharmacokinetics of the drug. For example, if an antibiotic is scheduled every eight hours, this time frame must be upheld to maintain effective bioavailability of the drug, but a medication scheduled daily has more flexibility with time of actual administration.
Right Route
During this step, the nurse ensures the route of administration is appropriate for the specific medication and also for the patient.[16] Many medications can potentially be administered via multiple routes, whereas other medications can only be given safely via one route. Nurses must administer medications via the route indicated in the order. If a nurse discovers an error in the order or believes the route is unsafe for a particular patient, the route must be clarified with the prescribing provider before administration. For example, a patient may have a PEG tube in place, but the nurse notices the medication order indicates the route of administration as PO. If the nurse believes this medication should be administered via the PEG tube and the route indicated in the order is an error, the prescribing provider must be notified, and the order must be revised indicating via PEG tube before the medication is administered.
Right Documentation
After administering medication, it is important to immediately document the administration to avoid potential errors from an unintended repeat dose.
In addition to checking the basic rights of medication administration and documenting the administration, it is also important for nurses to verify the following information to prevent medication errors.
Right History and Assessment
The nurse should be aware of the patient’s allergies, as well as any history of any drug interactions. Additionally, nurses collect appropriate assessment data regarding the patient’s history, current status, and recent lab results to identify any contraindications for the patients to receive the prescribed medication.[17]
Right Drug Interactions
The patient’s history should be reviewed for any potential interactions with medications previously given or with the patient’s diet. It is also important to verify the medication’s expiration date before administration.
Right Education and Information
Information should be provided to the patient about the medication, including the expected therapeutic effects, as well as the potential adverse effects. The patient should be encouraged to report suspected side effects to the nurse and/or prescribing provider. If the patient is a minor, the parent may also have a right to know about the medication in many states, depending upon the circumstances.
Right of Refusal
After providing education about the medication, the patient has the right to refuse to take medication in accordance with the nursing Code of Ethics and respect for individual patient autonomy. If a patient refuses to take the medication after proper education has been performed, the event should be documented in the patient chart and the prescribing provider notified.
Medication Dispensing
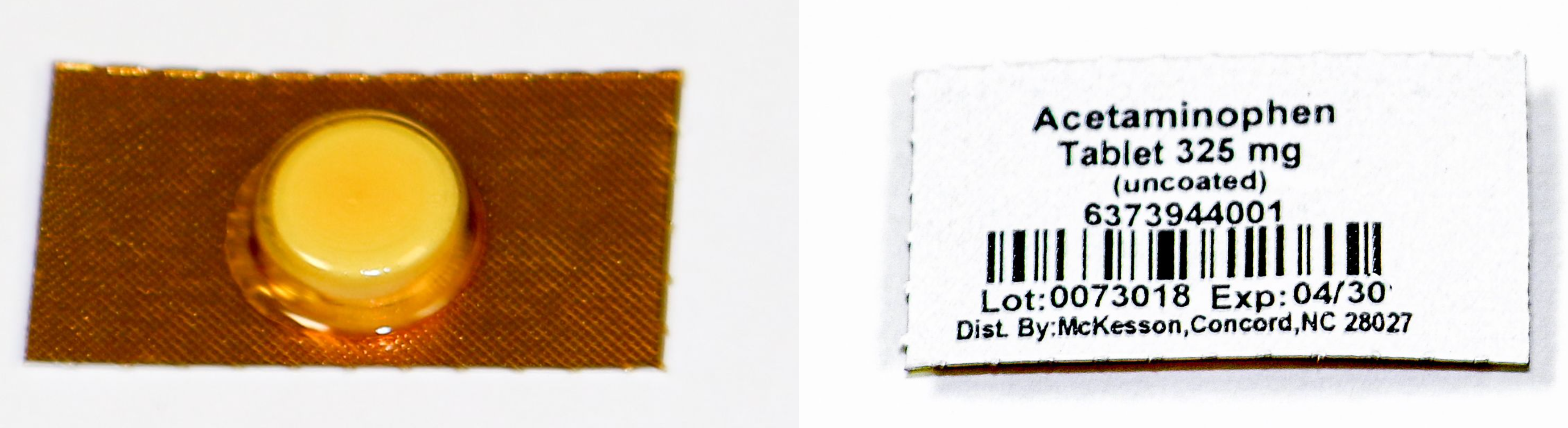
Medications are dispensed for patients in a variety of methods. During inpatient care, unit dose packaging is a common method for dispensing medications. See Figure 15.4[18] for an image of unit dose packaging.
Unit dose dispensing is typically used in association with a medication dispensing system, sometimes referred to in practice with brand names such as “Pyxis” or “Omnicell.” Medication dispensing systems help keep medications secure by requiring a user sign-in and password. They also reduce medication errors by only allowing medications prescribed for a specific patient to be removed unless additional actions are taken. However, it is important to remember that medication errors can still occur when using a medication dispensing system if the incorrect medication is erroneously stocked in a compartment. See Figure 15.5[19] for an image of a medication dispensing system.

Barcodes are often incorporated with unit dose medication dispensing as an additional layer of safety to prevent medication errors. Each patient and medication is identified with a unique bar code. The nurse scans the patient’s identification wristband with a bedside portable device and then scans each medication to be administered. The portable device will display error messages if an incorrect medication is scanned or if medication is scanned at an incorrect time. It is vital for nurses to stop and investigate the medication administration process when an error is received. The scanning device is typically linked to an electronic MAR and the medication administered is documented immediately in the patient’s chart.
In long-term care agencies, weekly blister cards may be used that contain a specific patient’s medications for each day of the week. See Figure 15.6[20] for an image of a blister pack.

Agencies using blister cards or pill bags typically store medications in a locked medication cart to keep them secure. Supplies used to administer medications are also stored on the cart. The MAR is available in printed format or electronically with a laptop computer. See Figure 15.7[21] for an image of a medication cart.

Process of Medication Administration
No matter what method of medication storage and dispensing is used in a facility, the nurse must continue to verify the rights of medication administration to perform an accurate and safe medication pass. Using a medication dispensing system or barcoding does not substitute for verifying the rights but is used to add an additional layer of safety to medication administration. Nurses can also avoid medication errors by creating a habitual process of performing medication checks when administering medication. The rights of medication administration should be done in the following order:
- Perform the first check as the unit dose package, blister pack, or pill bag is removed from the dispensing machine or medication cart. Also, check the expiration date of the medication.
- A second check should be performed after the medication is removed from the dispensing machine or medication cart. This step should be performed prior to pouring or removing from a multidose container. Note: Some high-alert medications, such as insulin, require a second nurse to perform a medication check at this step due to potentially life-threatening adverse effects that can occur if an error is made.
- The third check should be performed immediately before administering the medication to the patient at the bedside or when replacing the multidose container back into the drawer.
See Figure 15.8[22] for an image of a nurse comparing medication information on the medication packet to information on the patient’s MAR.
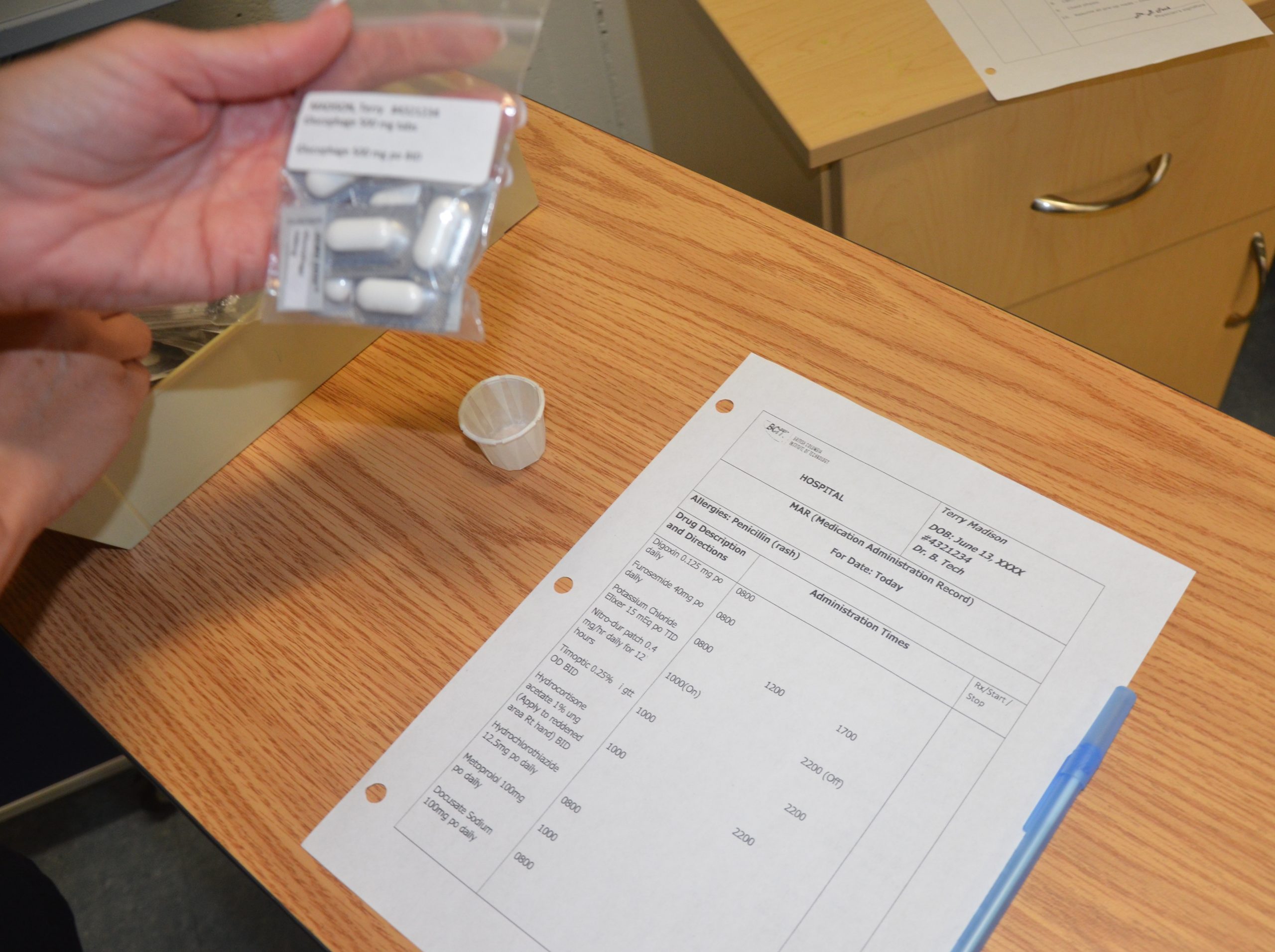
When performing these three checks, the nurse should ensure this is the right medication, right patient, right dosage, right route, and right time. See Figure 15.9[23] for an image of the nurse performing patient identification prior to administering the medication. The sixth right, correct documentation, should be done immediately after the medication is administered to the patient to avoid an error from another nurse inadvertently administering the dose a second time. These six rights completed three times have greatly reduced medication errors.
As discussed earlier, other rights to consider during this process are as follows:
- Is the patient receiving this medication for the right reason?
- Have the right assessments been performed prior to giving the medication?
- Has the patient also received the right education regarding the medications?
- Is the patient exhibiting the right response to the medication?
- Is the patient refusing to take the medication? Patients have the right to refuse medication. The patient’s refusal and any education or explanation provided related to the attempt to administer the medication should be documented by the nurse and the prescribing provider should be notified.
![]()
- Listen to the patient if they verbalize any concerns about medications. Explore their concerns, verify the order, and/or discuss their concerns with the prescribing provider before administering the medication to avoid a potential medication error.
- If a pill falls on the floor, it is contaminated and should not be administered. Dispose the medication according to agency policy.
- Be aware of absorption considerations of the medications you are administering. For example, certain medications such as levothyroxine should be administered on an empty stomach because food and other medications will affect its absorption.
- Nurses are often the first to notice when a patient has difficulty swallowing. If you notice a patient coughs immediately after swallowing water or has a “gurgling” sound to their voice, do not administer any medications, food, or fluid until you have reported your concerns to the heath care provider. A swallow evaluation may be needed, and the route of medication may need to be changed from oral to another route to avoid aspiration.
- If your patient has a nothing by mouth (NPO) order, verify if this includes all medications. This information may be included on the MAR or the orders, and if not, verify this information with the provider. Some medications, such as diabetes medication, may be given with a sip of water in some situations where the patient has NPO status.
- If the route of administration is not accurately listed on the MAR, contact the prescribing provider before administering the medication. For example, a patient may have a PEG tube, but the medication is erroneously listed as “PO” on the order.
For more information regarding classes of medications, administration considerations, and adverse effects to monitor, visit Open RN Nursing Pharmacology.
For information about specific medications, visit DailyMed, a current, evidence-based medication reference.
Special Considerations for Administering Controlled Substances
Controlled substances, also called Scheduled Medications, are kept in a locked system and accounted for using a checks and balance system. Removal of a controlled substance from a medication dispensing system must be verified and documented by a second nurse witness. Removal of a controlled substance from a medication cart needs to be documented on an additional controlled substance record with the patient’s name, the actual amount of substance given, the time it was given, associated pre-assessment data, and the name of the nurse administering the controlled substance.
Controlled substances stored in locked areas of medication carts must also be counted at every shift change by two nurses and then compared to the controlled substance administration record. If the count does not match the documentation record, the discrepancy must be reported immediately according to agency policy.
Additionally, if a partial dose of a controlled substance is administered, the remainder of the substance must be discarded in front of another nurse witness to document the event. This process is called “wasting.” Follow agency policy regarding wasting of controlled substances.
These additional safety measures help to prevent drug diversion, the use of a prescription medication for other than its intended purpose.
For more information about scheduled medications, drug diversion, and substance abuse in health care personnel, visit the “Legal/Ethical” chapter in Open RN Nursing Pharmacology.
Oral Medication Administration
Most medications are administered orally because it is the most convenient and least invasive route for the patient. Medication given orally has a slower onset, typically about 30-60 minutes. Prior to oral administration of medications, ensure the patient has no contraindications to receiving oral medication, is able to swallow, and is not on gastric suction. If the patient has difficulty swallowing (dysphagia), tablets are typically crushed and placed in a substance like applesauce or pudding for easier swallowing (based on the patient’s prescribed diet). However, it is important to verify that a tablet may be crushed by consulting a drug reference or a pharmacist. For example, medications such as enteric-coated tablets, capsules, and sustained-release or long-acting drugs should never be crushed because doing so will affect the intended action of the medication. In this event, the provider must be contacted for a change in route.[24]
View the ISMP Do Not Crush List.
Position the patient receiving oral medication in an upright position to decrease the risk of aspiration. Patients should remain in this position for 30 minutes after medication administration, if possible. If a patient is unable to sit, assist them into a side-lying position. See Figure 15.10[25] for an image of a nurse positioning the patient in an upright position prior to medication administration. Offer a glass of water or other oral fluid (that is not contraindicated with the medication) to ease swallowing and improve absorption and dissolution of the medication, taking any fluid restrictions into account.[26]
Remain with the patient until all medication has been swallowed before documenting to verify the medication has been administered.[27]
If any post-assessments are required, follow up in the appropriate time frame. For example, when administering oral pain medication, follow up approximately 30 minutes to an hour after medication is given to ensure effective pain relief.
If medication is given sublingual (under the tongue) or buccal (between the cheek and gum), the mouth should be moist. Offering the patient a drink of water prior to giving the medication can help with absorption. Instruct the patient to allow the medication to completely dissolve and reinforce the importance of not swallowing or chewing the medication.
Liquid medications are available in multidose vials or single-dose containers. It may be necessary to shake liquid medications if they are suspensions prior to pouring. Make sure the label is clearly written and easy to read. When pouring a liquid medication, it is ideal to place the label in the palm of your hand so if any liquid medication runs down the outside of the bottle it does not blur the writing and make the label unidentifiable. When pouring liquid medication, read the dose at eye level measuring at the meniscus of the poured fluid. Always follow specific agency policy and procedure when administering oral medications.

Rectal Medication Administration
Drugs administered rectally have a faster action than the oral route and a higher bioavailability, meaning a higher amount of effective drug in the bloodstream because it has not been influenced by upper gastrointestinal tract digestive processes. Rectal administration also reduces side effects of some drugs, such as gastric irritation, nausea, and vomiting. Rectal medications may also be prescribed for their local effects in the gastrointestinal system (e.g., laxatives) or their systemic effects (e.g., analgesics when oral route is contraindicated). Rectal medications are contraindicated after rectal or bowel surgery, with rectal bleeding or prolapse, and with low platelet counts.[28]
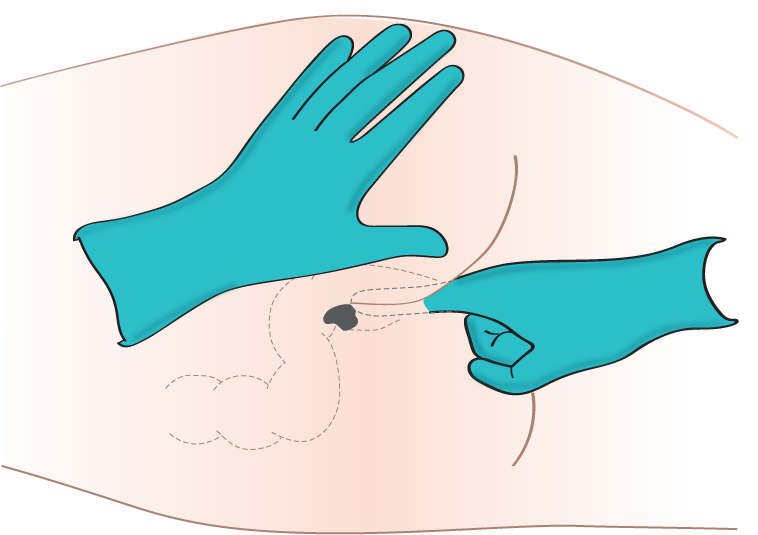
Rectal medications are often formulated as suppositories. Suppositories are small, cone-shaped objects that melt inside the body and release medication. When administering rectal suppositories, the patient should be placed on their left side in the Sims position. See Figure 15.11[29] for an image of patient positioning during rectal medication administration. The suppository and gloved index finger placing the suppository should be lubricated for ease of placement. Suppositories are conical and should be placed into the rectum rounded side first. The suppository should be inserted past the sphincter along the wall of the rectum. After placement, the patient should remain on their side while the medication takes effect. This time period is specific to each medication, but typically is at least 5 minutes. Make sure to avoid placing the suppository into stool. It is also important to monitor for a vasovagal response when placing medications rectally. A vasovagal response can occur when the vagus nerve is stimulated, causing the patient’s blood pressure and heart rate to drop, and creating symptoms of dizziness and perspiration. Sometimes the patient can faint or even have a seizure. Patients with a history of cardiac arrhythmias should not be administered rectal suppositories due to the potential for a vasovagal response. Always follow agency policy and procedure when administering rectal medications.[30],[31]
Another type of rectal medication is an enema. An enema is the administration of a substance in liquid form into the rectum. Many enemas are formulated in disposable plastic containers. Warming the solution to body temperature prior to administration may be beneficial because cold solution can cause cramping. It is also helpful to encourage the patient to empty their bladder prior to administration to reduce feelings of discomfort. Place an incontinence pad under the patient and position them on their left side in the Sims position. Lubricate the nozzle of the container and expel air. Insert the lubricated nozzle into the rectum slowly and gently expel the contents into the rectum. Ask the patient to retain the enema based on manufacturer’s recommendations.
Enteral Tube Medication Administration
Medication is administered via an enteral tube when the patient is unable to orally swallow medication. Medications given through an enteral feeding tube (nasogastric, nasointestinal, percutaneous endoscopic gastrostomy {PEG}, or jejunostomy {J} tube) should be in liquid form whenever possible to avoid clogging the tube. If a liquid form is not available, medications that are safe to crush should be crushed finely and dissolved in water to keep the tube from becoming clogged. If a medication is not safe to crush, the prescribing provider should be notified and a prescription for alternative medication obtained. Capsules should be opened and emptied into liquid as indicated prior to administration, and liquids should be administered at room temperature. Keep in mind that some capsules are time-released and should not be opened. In this case, contact the provider for a change in order.[32],[33]
As always, follow agency policy for this medication administration procedure. Position the patient to at least 30 degrees and in high Fowler’s position when feasible. If gastric suctioning is in place, turn off the suctioning. See Figure 15.12[34] for an image of a nurse positioning the patient prior to administration of medications via a PEG tube. Follow the tube to the point of entry into the patient to ensure you are accessing the correct tube.[35],[36]
Prior to medication administration, verify tube placement. Placement is initially verified immediately after the tube is placed with an X-ray, and the nurse should verify these results. Additionally, bedside placement is verified by the nurse before every medication pass. There are multiple evidence-based methods used to check placement. One method includes aspirating tube contents with a 60-mL syringe and observing the fluid. Fasting gastric secretions appear grassy-green, brown, or clear and colorless, whereas secretions from a tube that has perforated the pleural space typically have a pale yellow serous appearance. A second method used to verify placement is to measure the pH of aspirate from the tube. Fasting gastric pH is usually 5 or less, even in patients receiving gastric acid inhibitors. Fluid aspirated from a tube in the pleural space typically has a pH of 7 or higher.[37],[38] Note that installation of air into the tube while listening over the stomach with a stethoscope is no longer considered a safe method to check tube placement according to evidence-based practices.[39]
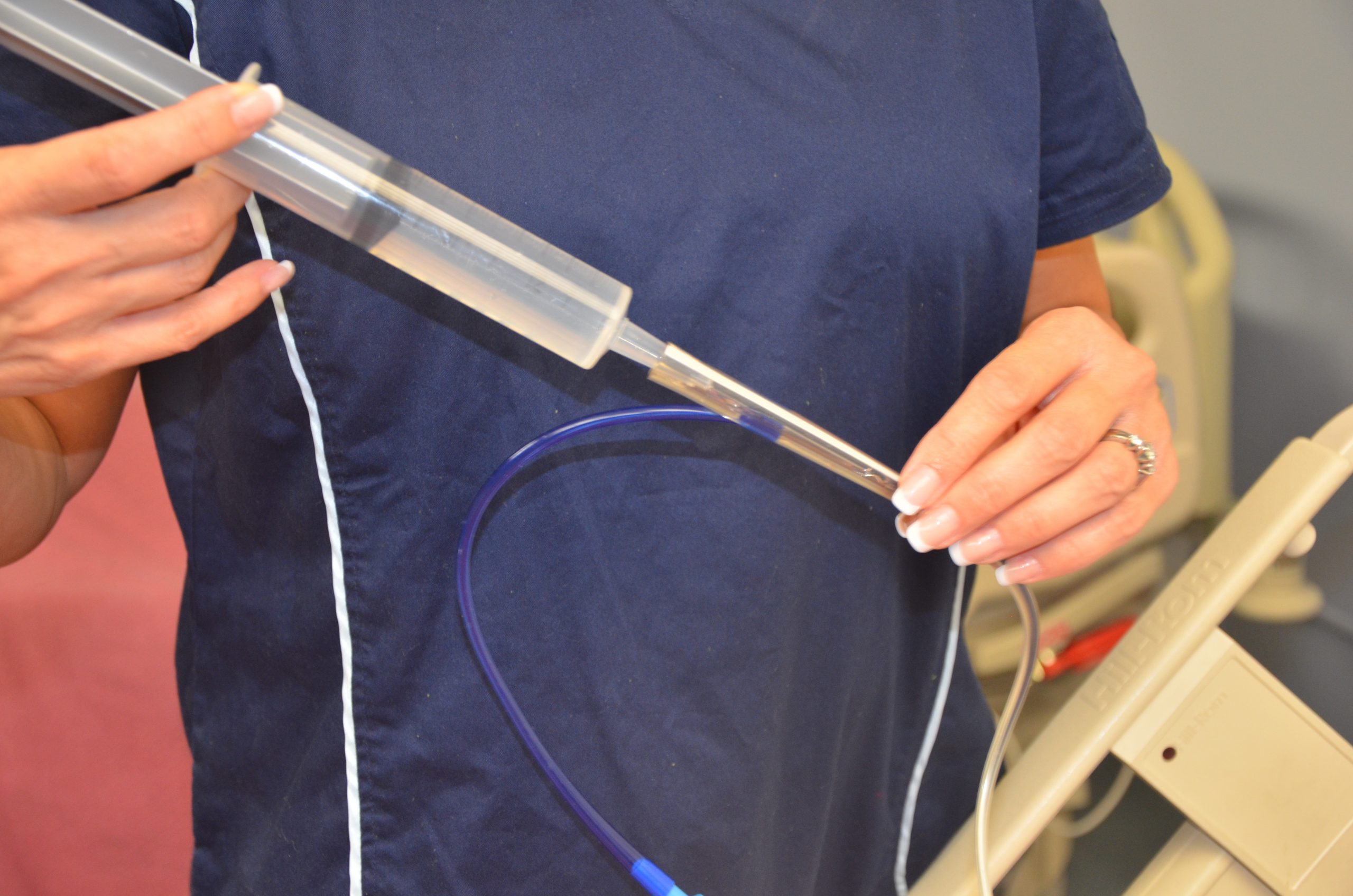
After tube placement is checked, a clean 60-mL syringe is used to flush the tube with a minimum of 15 mL of water (5-10 mL for children) before administering the medication. Follow agency policy regarding flushing amount. Liquid medication, or appropriately crushed medication dissolved in water, is administered one medication at a time. Medication should not be mixed because of the risks of physical and chemical incompatibilities, tube obstruction, and altered therapeutic drug responses. Between each medication, the tube is flushed with 15 mL of water, keeping in mind the patient’s fluid volume status. After the final medication is administered, the tube is flushed with 15 mL of water. The tube is then clamped, or if the patient is receiving tube feeding, it can be restarted. If the patient is receiving gastric suctioning, it can be restarted 30 minutes after medication administration.[40],[41],[42] See Figure 15.13[43] for an image of a nurse administering medication via an enteral tube.
Special considerations during this procedure include the following:
- If the patient has fluid restrictions, the amount of fluid used to flush the tube between each medication may need to be modified to avoid excess fluid intake.
- If the tube is attached to suctioning, the suctioning should be left off for 20 to 30 minutes after the medication is given to promote absorption of the medication.
- If the patient is receiving tube feedings, review information about the drugs that are being administered. If they cannot be taken with food or need to be taken on an empty stomach, the tube feeding running time will need to be adjusted.
- Be sure to document the amount of water used to flush the tube during the medication pass on the fluid intake record.
- If the patient has a chronic illness or is immunosuppressed, sterile water is suggested for use of mixing and flushing instead of tap water.
- Enteric-coated medications and other medications on the “Do Not Crush List” should not be crushed for this procedure. Instead, the prescribing provider must be notified and an order for a different form of the medication must be obtained.
- If the tube becomes clogged, attempt to flush it with water. If unsuccessful, notify the provider and a pancreatic enzyme solution or kit may be ordered before a new tube is placed.[44]

View a supplementary YouTube video on Crushing Medications[45]
Preventing Medication Errors
Medication errors can occur at various stages of the medication administration process, beginning with the prescribing provider, to the pharmacist preparing the medication, to the pharmacy technician stocking the medication, to the nurse administering the medication. Medication errors are most common at the ordering or prescribing stage. Typical errors include the prescribing provider writing the wrong medication, wrong route or dose, or the wrong frequency. These ordering errors account for almost 50% of medication errors. Data shows that nurses and pharmacists identify anywhere from 30% to 70% of medication-ordering errors.[46]
One of the major causes for medication errors is a distraction. Nearly 75% of medication errors have been attributed to this cause.[47] To minimize distractions, hospitals have introduced measures to reduce medication errors. For example, some hospitals set a “no-interruption zone policy” during medication dispensing and preparation and ask health care team members to only disrupt the medication administration process for emergencies. To reduce medication errors, agencies are also adopting many initiatives developed by the World Health Organization (WHO),[48] Institute for Safe Medication Practices (ISMP), Institute of Medicine (IOM),[49] and several other organizations. Initiatives include measures such as avoiding error-prone abbreviations, being aware of commonly confused medication names, and instituting additional safeguards for high-alert medications. Student nurses must also be aware of conditions that may contribute to making a medication error during their clinical courses. Read more about initiatives to prevent medication errors in the boxes and videos provided below.
For more information about preventing medication errors as a student nurse, visit IMSP’s Error-Prone Conditions that Lead to Student Nurse-Related Errors.
When you prepare to administer medications to your patients during clinical, your instructor will ask you questions to ensure safe medication administration. View a supplementary YouTube video of a nursing instructor asking a student typical medication questions.
View a supplementary YouTube video from the WHO on Administering Medications Without Harm[50]
Reporting Medication Errors
Despite multiple initiatives that have been instituted to prevent medication errors, including properly checking the rights of medication administration, medication errors happen. Examples of common errors include administering the wrong dose or an unsafe dose, giving medication to the wrong patient, administering medication by the wrong route or at the incorrect rate, and giving a drug that is expired. If a medication error occurs, the nurse must follow specific steps of reporting according to agency policy. In the past when medication errors occurred, the individual who caused it was usually blamed for the mishap and disciplinary action resulted. However, this culture of blame has shifted, and many medication errors by well-trained and careful nurses and other health care professions are viewed as potential symptoms of a system-wide problem. This philosophy is referred to as an institution’s safety culture. Thus, rather than focusing on disciplinary action, agencies are now trying to understand how the system failed causing the error to occur. This approach is designed to introduce safeguards at every level so that a mistake can be caught before the drug is given to the patient, which is often referred to as a “near miss.” For an agency to effectively institute a safety culture, all medication errors and near misses must be reported.
When a medication error occurs, the nurse’s first response should be to immediately monitor the patient’s condition and watch for any side effects from the medication. Secondly, the nurse must notify the nurse manager and prescribing provider of the error. The provider may provide additional orders to counteract the medication’s effects or to monitor for potential adverse reactions. In some situations, family members of the patient who are legal guardians or powers of attorney should also be notified. Lastly, a written report should be submitted documenting the incident, often referred to as an incident report. Incident reports are intended to identify if patterns of errors are occurring due to system-wide processes that can be modified to prevent future errors.
For more information about safety culture, visit the following section of the “Legal/Ethical” chapter in Open RN Nursing Pharmacology.
Life Span Considerations
Children
It can be difficult to persuade children to take medications. It is often helpful for medications to be prescribed in liquid or chewable form. For example, droppers are used for infants or very young children; the medication should be placed between the gum and cheek to prevent aspiration. Mixing medication with soft foods can also be helpful to encourage the child to swallow medications, but it is best to avoid mixing the medication with a staple food in the child’s diet because of potential later refusal of the food associated with medication administration. It can be helpful to offer the child a cool item, such as a popsicle or frozen fruit bar, prior to medication administration to numb the child’s tongue and decrease the taste of the medication. Other clinical tips for medication administration include asking the caregiver how the child takes medications at home and mimicking this method or asking the caregiver to administer the medication if the child trusts them more than the nurse. Oral syringes (without needles attached) may be used to administer precise dosages of medication to children. See Figure 15.14[51] of a nurse administering oral medication to a child with an oral syringe. When administering medication with an oral syringe, remember to remove the cap prior to administration because this could be a choking hazard. It is also important to educate the caregiver of the child how to properly administer the medication at the correct dosage at home.

Older Adults
Many older adults have a “polypharmacy,” meaning many medications to keep track of and multiple times these medications need to be taken per day. Nurses should help patients set up a schedule to remember when to take the medications. Organizing medications in medication boxes by day and time is a very helpful strategy. See Figure 15.15[52] of a medication box. Nurses can suggest to patients to have all medications filled at the same pharmacy to avoid drug-drug interactions that can occur when multiple providers are prescribing medications.
Older adults often have difficulty swallowing, so obtaining a prescription for liquid medication or crushing the medication when applicable and placing it in applesauce or pudding is helpful. Allow extra time when administering medication to an older adult to give them time to ask questions and to swallow multiple pills. Monitor for adverse effects and drug interactions in older adults, who are often taking multiple medications and may have preexisting kidney or liver dysfunction.
Be sure to address the economic needs of an older adult as it relates to their medications. Medications can be expensive, and many older adults live on a strict budget. Nurses often advocate for less expensive alternatives for patients, such as using a generic brand instead of a name brand or a less expensive class of medication. Be aware that an older adult with financial concerns may try to save money by not taking medications as frequently as prescribed. Also, the older adult may “feel good” on their medications and think they don’t need to monitor or take medications because they are “cured.” Reinforce that “feeling good” usually means the medication is working as prescribed and should continue to be taken. Finally, empower patients to take control of managing their health by providing education and ongoing support.

- NCSBN.(2018). 2019 NCLEX-RN test plan. https://www.ncsbn.org/2019_RN_TestPlan-English.pdf ↵
- Centers for Medicare & Medicaid Services. (2014, March 14). Memo: Requirements for hospital medication administration, particularly intravenous (IV) medications and post-operative care of patients receiving IV opioids. https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/SurveyCertificationGenInfo/Downloads/Survey-and-Cert-Letter-14-15.pdf ↵
- This work is a derivative of StatPearls by Tariq, Vashisht, Sinha, and Scherbak and is licensed under CC BY 4.0 ↵
- Centers for Medicare & Medicaid Services. (2014, March 14). Memo: Requirements for hospital medication administration, particularly intravenous (IV) medications and post-operative care of patients receiving IV opioids. https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/SurveyCertificationGenInfo/Downloads/Survey-and-Cert-Letter-14-15.pdf ↵
- Centers for Medicare & Medicaid Services. (2014, March 14). Memo: Requirements for hospital medication administration, particularly intravenous (IV) medications and post-operative care of patients receiving IV opioids. https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/SurveyCertificationGenInfo/Downloads/Survey-and-Cert-Letter-14-15.pdf ↵
- Vera, M. (2020, June 30). The 10 rights of drug administration. Nurselabs. https://nurseslabs.com/10-rs-rights-of-drug-administration/ ↵
- Butcher, H., Bulechek, G., Dochterman, J., & Wagner, C. (2018). Nursing interventions classification (NIC). Elsevier, pp.250-251,257-258. ↵
- Centers for Medicare & Medicaid Services. (2014, March 14). Memo: Requirements for hospital medication administration, particularly intravenous (IV) medications and post-operative care of patients receiving IV opioids. https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/SurveyCertificationGenInfo/Downloads/Survey-and-Cert-Letter-14-15.pdf ↵
- “Patient Identification.png” by BruceBlaus is licensed under CC BY-SA 4.0 ↵
- “Wrist Identification Band.jpg” by Whoisjohngalt is licensed under CC BY-SA 4.0 ↵
- The Joint Commission. (n.d.). National patient safety goals. https://www.jointcommission.org/standards/national-patient-safety-goals/ ↵
- Centers for Medicare & Medicaid Services. (2014, March 14). Memo: Requirements for hospital medication administration, particularly intravenous (IV) medications and post-operative care of patients receiving IV opioids. https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/SurveyCertificationGenInfo/Downloads/Survey-and-Cert-Letter-14-15.pdf ↵
- “MAR.png” by Meredith Pomietlo for Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- Centers for Medicare & Medicaid Services. (2014, March 14). Memo: Requirements for hospital medication administration, particularly intravenous (IV) medications and post-operative care of patients receiving IV opioids. https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/SurveyCertificationGenInfo/Downloads/Survey-and-Cert-Letter-14-15.pdf ↵
- Centers for Medicare & Medicaid Services. (2014, March 14). Memo: Requirements for hospital medication administration, particularly intravenous (IV) medications and post-operative care of patients receiving IV opioids. https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/SurveyCertificationGenInfo/Downloads/Survey-and-Cert-Letter-14-15.pdf ↵
- Centers for Medicare & Medicaid Services. (2014, March 14). Memo: Requirements for hospital medication administration, particularly intravenous (IV) medications and post-operative care of patients receiving IV opioids. https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/SurveyCertificationGenInfo/Downloads/Survey-and-Cert-Letter-14-15.pdf ↵
- NCSBN. (2018). 2019 NCLEX-RN test plan. https://www.ncsbn.org/2019_RN_TestPlan-English.pdf ↵
- “Unit Dose Packaging.jpg” and “Unit Dose Label.jpg” by Deanna Hoyord, Chippewa Valley Technical College are licensed under CC BY 4.0 ↵
- “Med Cart 1_313A0209.jpg” and “Med Cart Drawer._313A0224.jpg” by Deanna Hoyord, Chippewa Valley Technical College are licensed under CC BY 4.0 ↵
- “Medication_blister_pack_2.jpg” by Sprinno is licensed under CC BY-SA 3.0 ↵
- “MMI medication cart.JPG” by BrokenSphere is licensed under CC BY-SA 3.0 ↵
- “DSC_17601-150x150.jpg” by British Columbia Institute of Technology is licensed under CC BY 4.0. Access for free at https://opentextbc.ca/clinicalskills/chapter/6-1-safe-medication-adminstration/ ↵
- “Book-pictures-2015-430-150x150.jpg” by British Columbia Institute of Technology is licensed under CC BY 4.0.. Access for free at https://opentextbc.ca/clinicalskills/chapter/6-1-safe-medication-adminstration/ ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology and is licensed under CC BY 4.0 ↵
- “DSC_17631-150x150.jpg” by British Columbia Institute of Technology is licensed under CC BY 4.0. Access for free at https://opentextbc.ca/clinicalskills/chapter/6-1-safe-medication-adminstration/ ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology and is licensed under CC BY 4.0 ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology and is licensed under CC BY 4.0 ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology and is licensed under CC BY 4.0 ↵
- “Administering-med-rectally-2.png” by British Columbia Institute of Technology is licensed under CC BY 4.0 ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology and is licensed under CC BY 4.0 ↵
- Butcher, H., Bulechek, G., Dochterman, J., & Wagner, C. (2018). Nursing interventions classification (NIC). Elsevier, pp.250-251, 257-258. ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology and is licensed under CC BY 4.0 ↵
- Boullata, J. I., Carrera, A. L., Harvey, L., Escuro, A. A., Hudson, L., Mays, A., McGinnis, C., Wessel, J. J., Bajpai, S., Beebe, M. L., Kinn, T. J., Klang, M. G., Lord, L., Martin, K., Pompeii‐Wolfe, C., Sullivan, J., Wood, A., Malone, A., & Guenter, P. (2017). ASPEN safe practices for enteral nutrition therapy. Journal of Parenteral and Enteral Nutrition, 41(1), 15-103. https://doi.org/10.1177/0148607116673053 ↵
- “degreeLow.jpg” by British Columbia Institute of Technology is licensed under CC BY 4.0. Access for free at https://opentextbc.ca/clinicalskills/chapter/3-4-positioning-a-patient-in-bed/ ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology and is licensed under CC BY 4.0 ↵
- Boullata, J. I., Carrera, A. L., Harvey, L., Escuro, A. A., Hudson, L., Mays, A., McGinnis, C., Wessel, J. J., Bajpai, S., Beebe, M. L., Kinn, T. J., Klang, M. G., Lord, L., Martin, K., Pompeii‐Wolfe, C., Sullivan, J., Wood, A., Malone, A., & Guenter, P. (2017). ASPEN safe practices for enteral nutrition therapy. Journal of Parenteral and Enteral Nutrition, 41(1), 15-103. https://doi.org/10.1177/0148607116673053 ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology and is licensed under CC BY 4.0 ↵
- Boullata, J. I., Carrera, A. L., Harvey, L., Escuro, A. A., Hudson, L., Mays, A., McGinnis, C., Wessel, J. J., Bajpai, S., Beebe, M. L., Kinn, T. J., Klang, M. G., Lord, L., Martin, K., Pompeii‐Wolfe, C., Sullivan, J., Wood, A., Malone, A., & Guenter, P. (2017). ASPEN safe practices for enteral nutrition therapy. Journal of Parenteral and Enteral Nutrition, 41(1), 15-103. https://doi.org/10.1177/0148607116673053 ↵
- ABoullata, J. I., Carrera, A. L., Harvey, L., Escuro, A. A., Hudson, L., Mays, A., McGinnis, C., Wessel, J. J., Bajpai, S., Beebe, M. L., Kinn, T.J., Klang, M. G., Lord, L., Martin, K., Pompeii‐Wolfe, C., Sullivan, J., Wood, A., Malone, A., & Guenter, P. (2017). ASPEN safe practices for enteral nutrition therapy. Journal of Parenteral and Enteral Nutrition, 41(1), 15-103. https://doi.org/10.1177/0148607116673053 ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology and is licensed under CC BY 4.0 ↵
- Boullata, J. I., Carrera, A. L., Harvey, L., Escuro, A. A., Hudson, L., Mays, A., McGinnis, C., Wessel, J. J., Bajpai, S., Beebe, M. L., Kinn, T. J., Klang, M. G., Lord, L., Martin, K., Pompeii‐Wolfe, C., Sullivan, J., Wood, A., Malone, A., & Guenter, P. (2017). ASPEN safe practices for enteral nutrition therapy. Journal of Parenteral and Enteral Nutrition, 41(1), 15-103. https://doi.org/10.1177/0148607116673053 ↵
- Butcher, H., Bulechek, G., Dochterman, J., & Wagner, C. (2018). Nursing interventions classification (NIC). Elsevier, pp. 250-251, 257-258. ↵
- “Administering medication into a gastric tube.jpg” by British Columbia Institute of Technology is licensed under CC BY 4.0 ↵
- Boullata, J. I., Carrera, A. L., Harvey, L., Escuro, A. A., Hudson, L., Mays, A., McGinnis, C., Wessel, J. J., Bajpai, S., Beebe, M. L., Kinn, T. J., Klang, M. G., Lord, L., Martin, K., Pompeii‐Wolfe, C., Sullivan, J., Wood, A., Malone, A., & Guenter, P. (2017). ASPEN safe practices for enteral nutrition therapy. Journal of Parenteral and Enteral Nutrition, 41(1), 15-103. https://doi.org/10.1177/0148607116673053 ↵
- RegisteredNurseRN. (2017, March 22). Crushing medications for tube feeding and oral administration [Video]. YouTube. All rights reserved. Video used with permission. https://youtu.be/86RzAgHu75U ↵
- This work is a derivative of StatPearls by Tariq, Vashisht, Sinha, and Scherbak and is licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Tariq, Vashisht, Sinha, and Scherbak and is licensed under CC BY 4.0 ↵
- World Health Organization (n.d.). Patient safety. https://www.who.int/patientsafety/medication-safety/technical-reports/en/ ↵
- IOM. Institute of Medicine. (2007). Preventing medication errors. The National Academies Press. https://doi.org/10.17226/11623 ↵
- World Health Organization (WHO). (2017, October 6). WHO: Medication without harm [Video]. YouTube. All rights reserved. https://youtu.be/MWUM7LIXDeA ↵
- “USMC-080623-M-9467O-024.jpg” by Lance Cpl. Regina A. Ochoa for the United States Marine Corps is in the Public Domain. ↵
- “pills-4005382_960_720.jpg” by Nemo73 is licensed under CC0 ↵
There are two basic ways the body defends against pathogens: nonspecific innate immunity and specific adaptive immunity.
Nonspecific Innate Immunity
Nonspecific innate immunity is a system of defenses in the body that targets invading pathogens in a nonspecific manner. It is called “innate” because it is present from the moment we are born. Nonspecific innate immunity includes physical defenses, chemical defenses, and cellular defenses.[1]
Physical Defenses
Physical defenses are the body’s most basic form of defense against infection. They include physical barriers to microbes, such as skin and mucous membranes, as well as mechanical defenses that physically remove microbes and debris from areas of the body where they might cause harm or infection. In addition, a person’s microbiome provides physical protection against disease as normal flora compete with pathogens for nutrients and cellular-binding sites.[2]
Skin
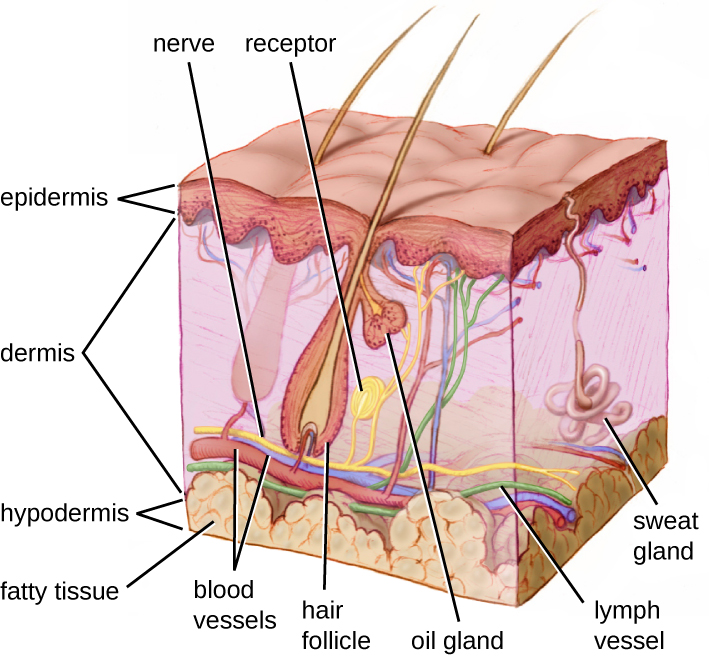
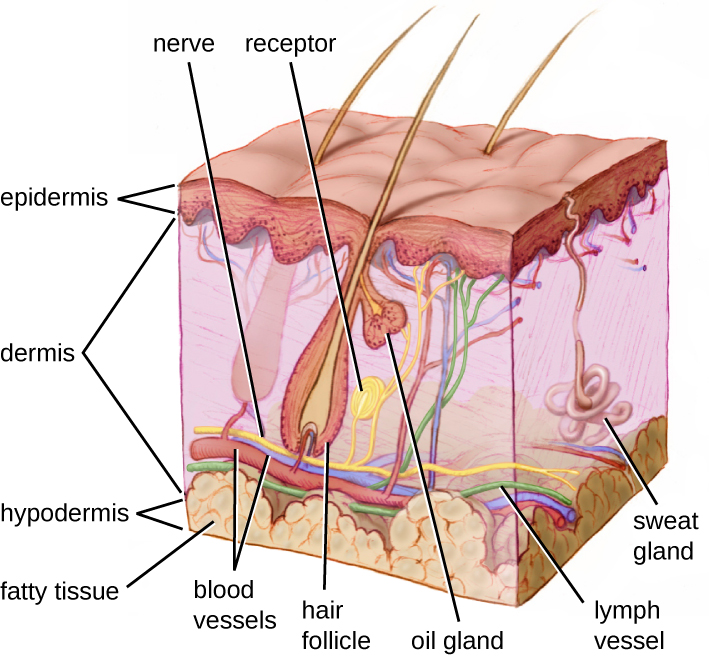
One of the body’s most important physical barriers is the skin barrier, which is composed of three layers of closely packed cells. See Figure 9.5[3] for an illustration of the layers of skin. The topmost layer of skin called the epidermis consists of cells that are packed with keratin. Keratin makes the skin’s surface mechanically tough and resistant to degradation by bacteria. Infections can occur when the skin barrier is broken, allowing the entry of opportunistic pathogens that infect the skin tissue surrounding the wound and possibly spread to deeper tissues.[4]
Mucus Membranes
The mucous membranes lining the nose, mouth, lungs, and urinary and digestive tracts provide another nonspecific barrier against potential pathogens. Mucous membranes consist of a layer of epithelial cells bound by tight junctions. The epithelial cells secrete a moist, sticky substance called mucous. Mucous covers and protects the fragile cell layers beneath it and also traps debris, including microbes. Mucus secretions also contain antimicrobial peptides.[5]
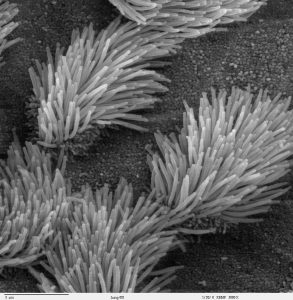
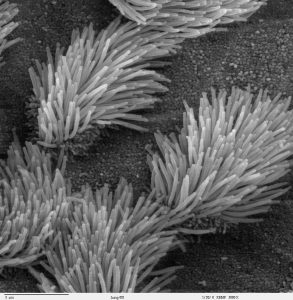
In many regions of the body, mechanical actions flush mucus (along with trapped or dead microbes) out of the body or away from potential sites of infection. For example, in the respiratory system, inhalation can bring microbes, dust, mold spores, and other small airborne debris into the body. This debris becomes trapped in the mucus lining the respiratory tract. The epithelial cells lining the upper parts of the respiratory tract have hair-like appendages known as cilia. Movement of the cilia propels debris-laden mucus out and away from the lungs. The expelled mucus is then swallowed and destroyed in the stomach, coughed up, or sneezed out. This system of removal is often called the mucociliary escalator. Disruption of the mucociliary escalator by the damaging effects of smoking can lead to increased colonization of bacteria in the lower respiratory tract and frequent infections, which highlights the importance of this physical barrier to host defenses.[6] See Figure 9.6[7] for an image of a magnified mucociliary escalator.
Like the respiratory tract, the digestive tract is a portal of entry through which microbes enter the body, and the mucous membranes lining the digestive tract provide a nonspecific physical barrier against ingested microbes. The intestinal tract is lined with epithelial cells, interspersed with mucus-secreting goblet cells. This mucus mixes with material received from the stomach, trapping foodborne microbes and debris, and is moved forward through the digestive tract via the mechanical action of peristalsis. Peristalsis refers to involuntary contraction and relaxation of the muscles of the intestine, creating wave-like movements that push digested content forward in the digestive tract.[8] For this reason, feces can contain microorganisms that can cause the spread of infection, making it essential to perform good hand hygiene to prevent transmission of disease through the fecal-oral route.
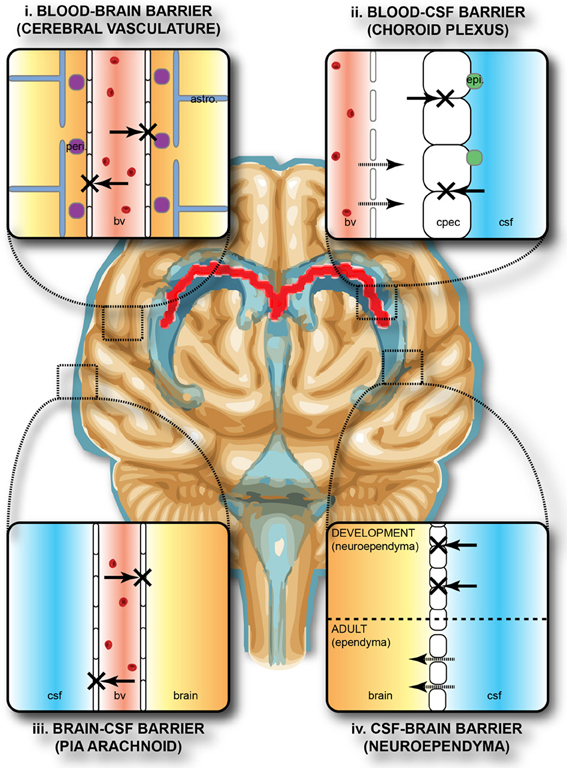
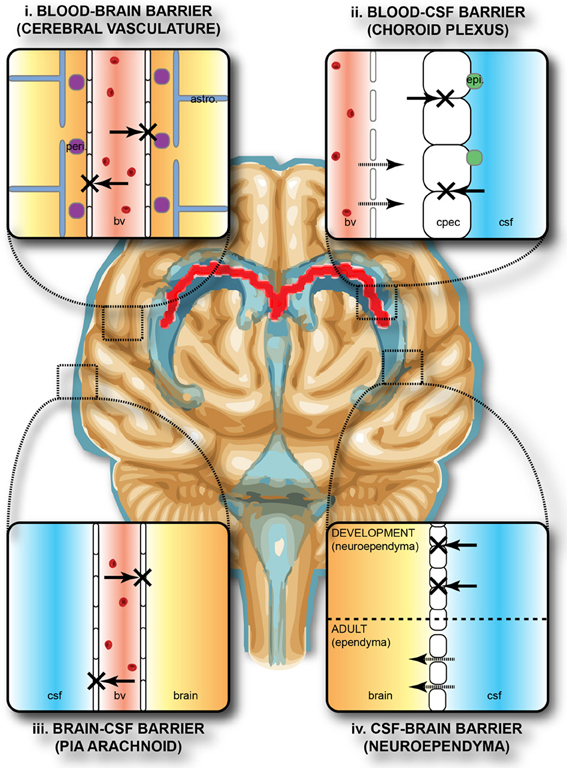
Endothelia
The epithelial cells lining the urogenital tract, blood vessels, lymphatic vessels, and other tissues are known as endothelia. These tightly packed cells provide an effective frontline barrier against invaders. The endothelia of the blood-brain barrier, for example, protects the central nervous system (CNS) from microorganisms. Infection of the CNS can quickly lead to serious and often fatal inflammation. The protection of the blood-brain barrier keeps the cerebrospinal fluid that surrounds the brain and spinal cord sterile.[9] See Figure 9.7[10] for an illustration of the blood-brain barrier.
Mechanical Defenses
In addition to physical barriers that keep microbes out, the body has several mechanical defenses that physically remove pathogens from the body and prevent them from taking up residence. For example, the flushing action of urine and tears serves to carry microbes away from the body. The flushing action of urine is responsible for the normally sterile environment of the urinary tract. The eyes have additional physical barriers and mechanical mechanisms for preventing infections. The eyelashes and eyelids prevent dust and airborne microorganisms from reaching the surface of the eye. Any microbes or debris that make it past these physical barriers is flushed out by the mechanical action of blinking, which bathes the eye in tears, washing debris away.[11] See Figure 9.8[12] for an image of an infant’s eyelashes that prevent dust from reaching the surface of the eye.

Microbiome
Normal flora that contributes to an individual’s microbiome serve as an important first-line defense against invading pathogens. Through their occupation of cellular binding sites and competition for available nutrients, normal flora prevents the early steps of pathogen attachment and proliferation required for the establishment of an infection. For example, in the vagina, normal flora competes with opportunistic pathogens like Candida albicans. This competition prevents yeast infection by limiting the availability of nutrients and inhibiting the growth of Candida, keeping its population in check. Similar competitions occur between normal flora and potential pathogens on the skin, in the upper respiratory tract, and in the gastrointestinal tract.[13]
The importance of the normal flora in host defenses is highlighted by a person’s increased susceptibility to infectious diseases when their microbiome is disrupted or eliminated. For example, treatment with antibiotics can significantly deplete the normal flora of the gastrointestinal tract, providing an advantage for pathogenic bacteria such as Clostridium difficile (C-diff) to colonize and cause diarrheal infection. Diarrhea caused by C-diff can be severe and potentially lethal. In fact, a recent strategy for treating recurrent C-diff infections is fecal transplantation that involves the transfer of fecal material from a donor into the intestines of the client as a method of restoring their normal flora.[14]
Chemical Defenses
In addition to physical defenses, our nonspecific innate immune system uses several chemical mediators that inhibit microbial invaders. The term chemical mediators encompass a wide array of substances found in various fluids and tissues throughout the body. For example, sebaceous glands in the dermis secrete an oil called sebum that is released onto the skin surface through hair follicles. Sebum provides an additional layer of defense by helping seal off the pore of the hair follicle and preventing bacteria on the skin’s surface from invading sweat glands and surrounding tissue. Environmental factors can affect these chemical defenses of the skin. For example, low humidity in the winter makes the skin drier and more susceptible to pathogens normally inhibited by the skin’s low pH. Application of skin moisturizer restores moisture and essential oils to the skin and helps prevent dry skin from becoming infected.[15]
Examples of other chemical defenses are enzymes, pH level, and chemical mediators. Enzymes in saliva and the digestive tract eliminate most pathogens that manage to survive the acidic environment of the stomach. In the urinary tract, the slight acidity of urine inhibits the growth of potential pathogens in the urinary tract. The respiratory tract also uses various chemical mediators in the nasal passages, trachea, and lungs that have antibacterial properties.[16]
Plasma Protein Mediators
In addition to physical, mechanical, and chemical defenses, there are also nonspecific innate immune factors in plasma, the fluid portion of blood, such as acute-phase proteins, complement proteins, and cytokines. These plasma protein mediators contribute to the inflammatory response.[17]
An example of an acute-phase protein is C-reactive protein. High levels of C-reactive protein indicate inflammation caused by a serious infection or other medical condition.[18]
Complement proteins are always present in the blood and tissue fluids, allowing them to be activated quickly. They aid in the destruction of pathogens by piercing their outer membranes (cell lysis) or by making them more attractive to phagocytic cells such as macrophages.[19]
Cytokines are proteins that affect interaction and communication between cells. When a pathogen enters the body, the first immune cell to notice the pathogen is like the conductor of an orchestra. That cell directs all the other immune cells by creating and sending out messages (cytokines) to the rest of the organs or cells in the body to respond to and initiate inflammation. Too many cytokines can have a negative effect and result in what's known as a cytokine storm.[20],[21] A cytokine storm is a severe immune reaction in which the body releases too many cytokines into the blood too quickly. A cytokine storm can occur as a result of an infection, autoimmune condition, or other disease. Signs and symptoms include high fever, inflammation, severe fatigue, and nausea. A cytokine storm can be severe or life-threatening and lead to multiple organ failure. For example, many COVID-19 complications and deaths were caused by a cytokine storm.[22],[23]
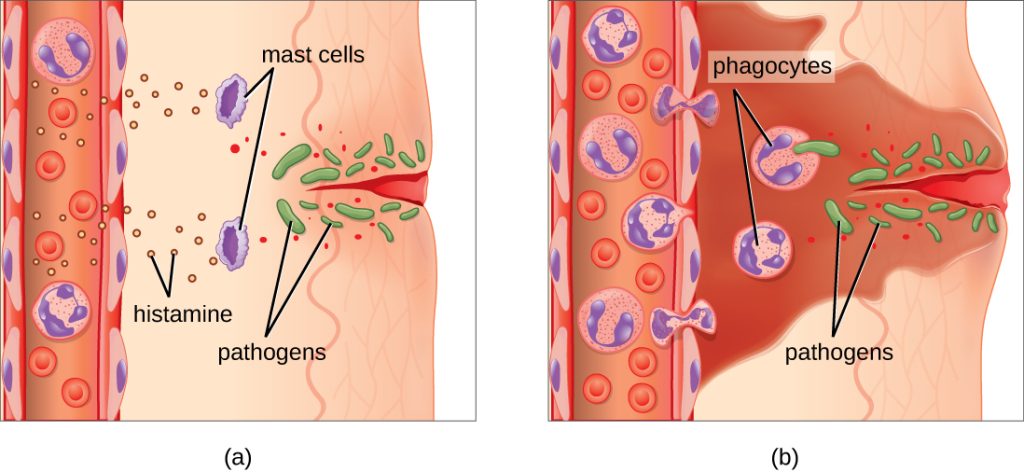
Inflammation
Inflammation is a response triggered by a cascade of chemical mediators and occurs when pathogens successfully breach the nonspecific innate immune system or when an injury occurs. Although inflammation is often perceived as a negative consequence of injury or disease, it is a necessary process that recruits cellular defenses needed to eliminate pathogens, remove damaged and dead cells, and initiate repair mechanisms. Excessive inflammation, however, can result in local tissue damage, and in severe cases, such as sepsis, it can become deadly.[24]
An immediate response to tissue injury is acute inflammation. Vasoconstriction occurs to minimize blood loss if injury has occurred. Vasoconstriction is followed by vasodilation with increased permeability of the blood vessels due to the release of histamine by mast cells. Histamine contributes to the five observable signs of the inflammatory response: erythema (redness), edema (swelling), heat, pain, and altered function. It is also associated with an influx of phagocytes at the site of injury and/or infection. See Figure 9.9[25] for an illustration of the inflammatory response, with (a) demonstrating when mast cells detect injury to nearby cells and release histamine, initiating an inflammatory response and (b) illustrating where histamine increases blood flow to the wound site and the associated increased vascular permeability allows fluid, proteins, phagocytes, and other immune cells to enter infected tissue. These events result in the swelling and reddening of the injured site. The increased blood flow to the injured site causes it to feel warm. Inflammation is also associated with pain due to these events stimulating nerve pain receptors in the tissue. Increasing numbers of neutrophils are then recruited to the area to fight pathogens. As the fight rages on, white blood cells are recruited to the area, and pus forms from the accumulation of neutrophils, dead cells, tissue fluids, and lymph. Typically, after a few days, macrophages clear out this pus.[26] During injury, if this nonspecific inflammatory process does not successfully kill the pathogens, infection occurs.
Fever
A fever is part of the inflammatory response that extends beyond the site of infection and affects the entire body, resulting in an overall increase in body temperature. Like other forms of inflammation, a fever enhances the nonspecific innate immune defenses by stimulating white blood cells to kill pathogens. The rise in body temperature also inhibits the growth of many pathogens. During fever, the client’s skin may appear pale due to vasoconstriction of the blood vessels in the skin to divert blood flow away from extremities, minimize the loss of heat, and raise the body’s core temperature. The hypothalamus also stimulates the shivering of muscles to generate heat and raise the core temperature.[27]
A low-level fever is thought to help an individual overcome an illness. However, in some instances, this immune response can be too strong, causing tissue and organ damage and, in severe cases, even death. For example, Staphylococcus aureus and Streptococcus pyogenes are capable of producing superantigens that cause toxic shock syndrome and scarlet fever, respectively. Both of these conditions are associated with extremely high fevers in excess of 42 °C (108 °F) that must be managed to prevent tissue injury and death.[28]
When a fever breaks, the hypothalamus stimulates vasodilation, resulting in a return of blood flow to the skin and a subsequent release of heat from the body. The hypothalamus also stimulates sweating, which cools the skin as the sweat evaporates.[29]
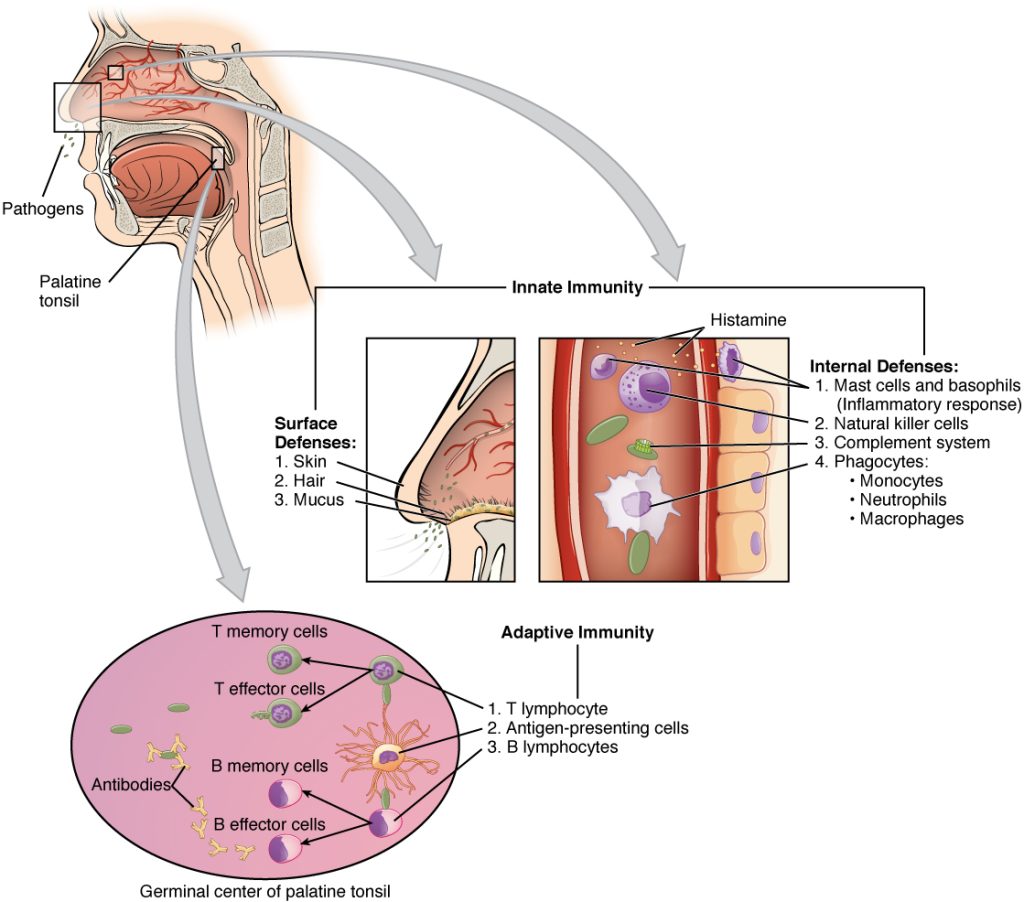
Specific Adaptive Immunity
Now that we have discussed several nonspecific innate defenses against a pathogen, let’s discuss specific adaptive immunity. Specific adaptive immunity is the immune response that is activated when the nonspecific innate immune response is insufficient to control an infection. There are two types of adaptive responses: the cell-mediated immune response, which is carried out by T cells, and the humoral immune response, which is controlled by activated B cells and antibodies.[30]
B cells mature in the bone marrow. B cells make Y-shaped proteins called antibodies that are specific to each pathogen and lock onto its surface and mark it for destruction by other immune cells. The five classes of antibodies are IgG, IgM, IgA, IgD, and IgE. They also turn into memory B cells. Memory B cells are stored and released in the event a specific antigen reappears in the future. This allows the immune system to mount a quick defense because of the previously created memory B cells.[31]
T cells mature in the thymus. T cells are categorized into three classes: helper T cells, regulatory T cells, and cytotoxic T cells. Helper T cells stimulate B cells to make antibodies and help killer cells develop. Killer T cells directly kill cells that have already been infected by a pathogen. T cells also use cytokines as messenger molecules to send chemical instructions to the rest of the immune system to ramp up its response.[32]
Specific adaptive immunity also creates memory cells for each specific pathogen that provides the host with long-term protection from reinfection with that pathogen. On reexposure, these memory cells facilitate an efficient and quick immune response. For example, when an individual recovers from chicken pox, the body develops a memory of the varicella-zoster virus that will specifically protect it from reinfection if it is exposed to the virus again. Vaccines are administered with the purpose of enhancing a person's specific adaptive immunity.[33]
See Figure 9.10[34] for an illustration of innate immunity and specific adaptive immunity that occur in response to a pathogen entering the body through the nose.
There are two basic ways the body defends against pathogens: nonspecific innate immunity and specific adaptive immunity.
Nonspecific Innate Immunity
Nonspecific innate immunity is a system of defenses in the body that targets invading pathogens in a nonspecific manner. It is called “innate” because it is present from the moment we are born. Nonspecific innate immunity includes physical defenses, chemical defenses, and cellular defenses.[35]
Physical Defenses
Physical defenses are the body’s most basic form of defense against infection. They include physical barriers to microbes, such as skin and mucous membranes, as well as mechanical defenses that physically remove microbes and debris from areas of the body where they might cause harm or infection. In addition, a person’s microbiome provides physical protection against disease as normal flora compete with pathogens for nutrients and cellular-binding sites.[36]
Skin
One of the body’s most important physical barriers is the skin barrier, which is composed of three layers of closely packed cells. See Figure 9.5[37] for an illustration of the layers of skin. The topmost layer of skin called the epidermis consists of cells that are packed with keratin. Keratin makes the skin’s surface mechanically tough and resistant to degradation by bacteria. Infections can occur when the skin barrier is broken, allowing the entry of opportunistic pathogens that infect the skin tissue surrounding the wound and possibly spread to deeper tissues.[38]
Mucus Membranes
The mucous membranes lining the nose, mouth, lungs, and urinary and digestive tracts provide another nonspecific barrier against potential pathogens. Mucous membranes consist of a layer of epithelial cells bound by tight junctions. The epithelial cells secrete a moist, sticky substance called mucous. Mucous covers and protects the fragile cell layers beneath it and also traps debris, including microbes. Mucus secretions also contain antimicrobial peptides.[39]
In many regions of the body, mechanical actions flush mucus (along with trapped or dead microbes) out of the body or away from potential sites of infection. For example, in the respiratory system, inhalation can bring microbes, dust, mold spores, and other small airborne debris into the body. This debris becomes trapped in the mucus lining the respiratory tract. The epithelial cells lining the upper parts of the respiratory tract have hair-like appendages known as cilia. Movement of the cilia propels debris-laden mucus out and away from the lungs. The expelled mucus is then swallowed and destroyed in the stomach, coughed up, or sneezed out. This system of removal is often called the mucociliary escalator. Disruption of the mucociliary escalator by the damaging effects of smoking can lead to increased colonization of bacteria in the lower respiratory tract and frequent infections, which highlights the importance of this physical barrier to host defenses.[40] See Figure 9.6[41] for an image of a magnified mucociliary escalator.
Like the respiratory tract, the digestive tract is a portal of entry through which microbes enter the body, and the mucous membranes lining the digestive tract provide a nonspecific physical barrier against ingested microbes. The intestinal tract is lined with epithelial cells, interspersed with mucus-secreting goblet cells. This mucus mixes with material received from the stomach, trapping foodborne microbes and debris, and is moved forward through the digestive tract via the mechanical action of peristalsis. Peristalsis refers to involuntary contraction and relaxation of the muscles of the intestine, creating wave-like movements that push digested content forward in the digestive tract.[42] For this reason, feces can contain microorganisms that can cause the spread of infection, making it essential to perform good hand hygiene to prevent transmission of disease through the fecal-oral route.
Endothelia
The epithelial cells lining the urogenital tract, blood vessels, lymphatic vessels, and other tissues are known as endothelia. These tightly packed cells provide an effective frontline barrier against invaders. The endothelia of the blood-brain barrier, for example, protects the central nervous system (CNS) from microorganisms. Infection of the CNS can quickly lead to serious and often fatal inflammation. The protection of the blood-brain barrier keeps the cerebrospinal fluid that surrounds the brain and spinal cord sterile.[43] See Figure 9.7[44] for an illustration of the blood-brain barrier.
Mechanical Defenses
In addition to physical barriers that keep microbes out, the body has several mechanical defenses that physically remove pathogens from the body and prevent them from taking up residence. For example, the flushing action of urine and tears serves to carry microbes away from the body. The flushing action of urine is responsible for the normally sterile environment of the urinary tract. The eyes have additional physical barriers and mechanical mechanisms for preventing infections. The eyelashes and eyelids prevent dust and airborne microorganisms from reaching the surface of the eye. Any microbes or debris that make it past these physical barriers is flushed out by the mechanical action of blinking, which bathes the eye in tears, washing debris away.[45] See Figure 9.8[46] for an image of an infant’s eyelashes that prevent dust from reaching the surface of the eye.

Microbiome
Normal flora that contributes to an individual’s microbiome serve as an important first-line defense against invading pathogens. Through their occupation of cellular binding sites and competition for available nutrients, normal flora prevents the early steps of pathogen attachment and proliferation required for the establishment of an infection. For example, in the vagina, normal flora competes with opportunistic pathogens like Candida albicans. This competition prevents yeast infection by limiting the availability of nutrients and inhibiting the growth of Candida, keeping its population in check. Similar competitions occur between normal flora and potential pathogens on the skin, in the upper respiratory tract, and in the gastrointestinal tract.[47]
The importance of the normal flora in host defenses is highlighted by a person’s increased susceptibility to infectious diseases when their microbiome is disrupted or eliminated. For example, treatment with antibiotics can significantly deplete the normal flora of the gastrointestinal tract, providing an advantage for pathogenic bacteria such as Clostridium difficile (C-diff) to colonize and cause diarrheal infection. Diarrhea caused by C-diff can be severe and potentially lethal. In fact, a recent strategy for treating recurrent C-diff infections is fecal transplantation that involves the transfer of fecal material from a donor into the intestines of the client as a method of restoring their normal flora.[48]
Chemical Defenses
In addition to physical defenses, our nonspecific innate immune system uses several chemical mediators that inhibit microbial invaders. The term chemical mediators encompass a wide array of substances found in various fluids and tissues throughout the body. For example, sebaceous glands in the dermis secrete an oil called sebum that is released onto the skin surface through hair follicles. Sebum provides an additional layer of defense by helping seal off the pore of the hair follicle and preventing bacteria on the skin’s surface from invading sweat glands and surrounding tissue. Environmental factors can affect these chemical defenses of the skin. For example, low humidity in the winter makes the skin drier and more susceptible to pathogens normally inhibited by the skin’s low pH. Application of skin moisturizer restores moisture and essential oils to the skin and helps prevent dry skin from becoming infected.[49]
Examples of other chemical defenses are enzymes, pH level, and chemical mediators. Enzymes in saliva and the digestive tract eliminate most pathogens that manage to survive the acidic environment of the stomach. In the urinary tract, the slight acidity of urine inhibits the growth of potential pathogens in the urinary tract. The respiratory tract also uses various chemical mediators in the nasal passages, trachea, and lungs that have antibacterial properties.[50]
Plasma Protein Mediators
In addition to physical, mechanical, and chemical defenses, there are also nonspecific innate immune factors in plasma, the fluid portion of blood, such as acute-phase proteins, complement proteins, and cytokines. These plasma protein mediators contribute to the inflammatory response.[51]
An example of an acute-phase protein is C-reactive protein. High levels of C-reactive protein indicate inflammation caused by a serious infection or other medical condition.[52]
Complement proteins are always present in the blood and tissue fluids, allowing them to be activated quickly. They aid in the destruction of pathogens by piercing their outer membranes (cell lysis) or by making them more attractive to phagocytic cells such as macrophages.[53]
Cytokines are proteins that affect interaction and communication between cells. When a pathogen enters the body, the first immune cell to notice the pathogen is like the conductor of an orchestra. That cell directs all the other immune cells by creating and sending out messages (cytokines) to the rest of the organs or cells in the body to respond to and initiate inflammation. Too many cytokines can have a negative effect and result in what's known as a cytokine storm.[54],[55] A cytokine storm is a severe immune reaction in which the body releases too many cytokines into the blood too quickly. A cytokine storm can occur as a result of an infection, autoimmune condition, or other disease. Signs and symptoms include high fever, inflammation, severe fatigue, and nausea. A cytokine storm can be severe or life-threatening and lead to multiple organ failure. For example, many COVID-19 complications and deaths were caused by a cytokine storm.[56],[57]
Inflammation
Inflammation is a response triggered by a cascade of chemical mediators and occurs when pathogens successfully breach the nonspecific innate immune system or when an injury occurs. Although inflammation is often perceived as a negative consequence of injury or disease, it is a necessary process that recruits cellular defenses needed to eliminate pathogens, remove damaged and dead cells, and initiate repair mechanisms. Excessive inflammation, however, can result in local tissue damage, and in severe cases, such as sepsis, it can become deadly.[58]
An immediate response to tissue injury is acute inflammation. Vasoconstriction occurs to minimize blood loss if injury has occurred. Vasoconstriction is followed by vasodilation with increased permeability of the blood vessels due to the release of histamine by mast cells. Histamine contributes to the five observable signs of the inflammatory response: erythema (redness), edema (swelling), heat, pain, and altered function. It is also associated with an influx of phagocytes at the site of injury and/or infection. See Figure 9.9[59] for an illustration of the inflammatory response, with (a) demonstrating when mast cells detect injury to nearby cells and release histamine, initiating an inflammatory response and (b) illustrating where histamine increases blood flow to the wound site and the associated increased vascular permeability allows fluid, proteins, phagocytes, and other immune cells to enter infected tissue. These events result in the swelling and reddening of the injured site. The increased blood flow to the injured site causes it to feel warm. Inflammation is also associated with pain due to these events stimulating nerve pain receptors in the tissue. Increasing numbers of neutrophils are then recruited to the area to fight pathogens. As the fight rages on, white blood cells are recruited to the area, and pus forms from the accumulation of neutrophils, dead cells, tissue fluids, and lymph. Typically, after a few days, macrophages clear out this pus.[60] During injury, if this nonspecific inflammatory process does not successfully kill the pathogens, infection occurs.
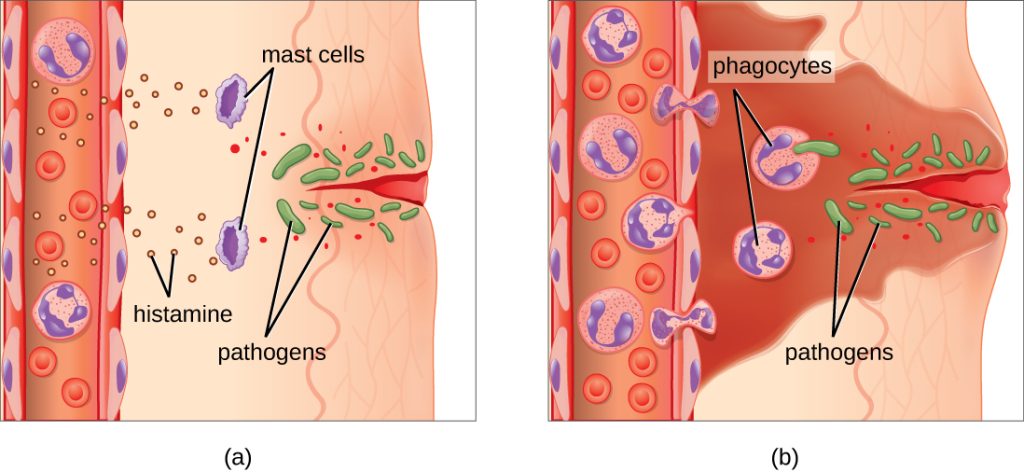
Fever
A fever is part of the inflammatory response that extends beyond the site of infection and affects the entire body, resulting in an overall increase in body temperature. Like other forms of inflammation, a fever enhances the nonspecific innate immune defenses by stimulating white blood cells to kill pathogens. The rise in body temperature also inhibits the growth of many pathogens. During fever, the client’s skin may appear pale due to vasoconstriction of the blood vessels in the skin to divert blood flow away from extremities, minimize the loss of heat, and raise the body’s core temperature. The hypothalamus also stimulates the shivering of muscles to generate heat and raise the core temperature.[61]
A low-level fever is thought to help an individual overcome an illness. However, in some instances, this immune response can be too strong, causing tissue and organ damage and, in severe cases, even death. For example, Staphylococcus aureus and Streptococcus pyogenes are capable of producing superantigens that cause toxic shock syndrome and scarlet fever, respectively. Both of these conditions are associated with extremely high fevers in excess of 42 °C (108 °F) that must be managed to prevent tissue injury and death.[62]
When a fever breaks, the hypothalamus stimulates vasodilation, resulting in a return of blood flow to the skin and a subsequent release of heat from the body. The hypothalamus also stimulates sweating, which cools the skin as the sweat evaporates.[63]
Specific Adaptive Immunity
Now that we have discussed several nonspecific innate defenses against a pathogen, let’s discuss specific adaptive immunity. Specific adaptive immunity is the immune response that is activated when the nonspecific innate immune response is insufficient to control an infection. There are two types of adaptive responses: the cell-mediated immune response, which is carried out by T cells, and the humoral immune response, which is controlled by activated B cells and antibodies.[64]
B cells mature in the bone marrow. B cells make Y-shaped proteins called antibodies that are specific to each pathogen and lock onto its surface and mark it for destruction by other immune cells. The five classes of antibodies are IgG, IgM, IgA, IgD, and IgE. They also turn into memory B cells. Memory B cells are stored and released in the event a specific antigen reappears in the future. This allows the immune system to mount a quick defense because of the previously created memory B cells.[65]
T cells mature in the thymus. T cells are categorized into three classes: helper T cells, regulatory T cells, and cytotoxic T cells. Helper T cells stimulate B cells to make antibodies and help killer cells develop. Killer T cells directly kill cells that have already been infected by a pathogen. T cells also use cytokines as messenger molecules to send chemical instructions to the rest of the immune system to ramp up its response.[66]
Specific adaptive immunity also creates memory cells for each specific pathogen that provides the host with long-term protection from reinfection with that pathogen. On reexposure, these memory cells facilitate an efficient and quick immune response. For example, when an individual recovers from chicken pox, the body develops a memory of the varicella-zoster virus that will specifically protect it from reinfection if it is exposed to the virus again. Vaccines are administered with the purpose of enhancing a person's specific adaptive immunity.[67]
See Figure 9.10[68] for an illustration of innate immunity and specific adaptive immunity that occur in response to a pathogen entering the body through the nose.
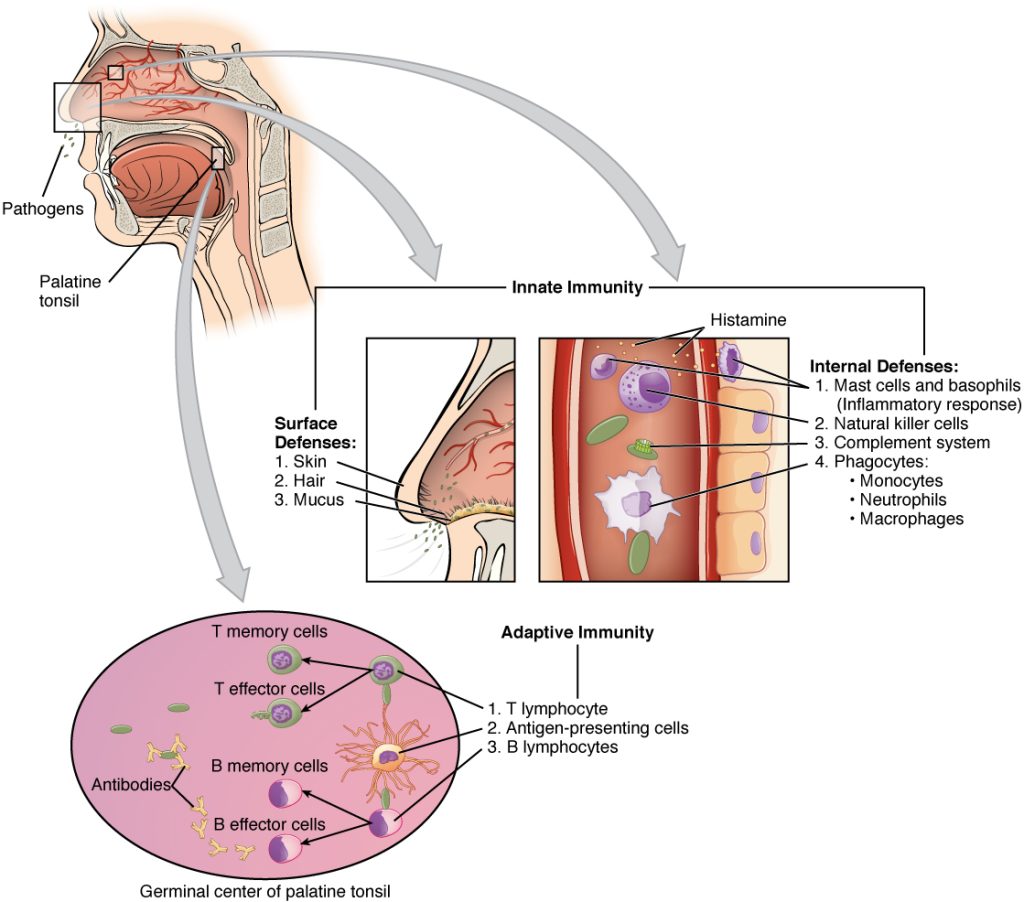
Now that we have discussed the pathophysiology of our immune system and interventions to treat and prevent infection, let’s apply this information to using the nursing process when providing client care.
Assessment
When assessing an individual who is feeling ill but has not yet been diagnosed with an infection, general symptoms associated with the prodromal period of disease may be present due to the activation of the immune system. These symptoms include a feeling of malaise (not feeling well), headache, fever, and lack of appetite. As an infection moves into the acute phase of disease, more specific signs and symptoms related to the specific type of infection will occur.
A fever is a common sign of inflammation and infection. A temperature of 38 degrees Celsius (100.4 degrees F) is generally considered a low-grade fever, and a temperature of 38.3 degrees Celsius (101 degrees F) is considered a fever.[69] As discussed earlier in this chapter, fever is part of the nonspecific innate immune response and can be beneficial in destroying pathogens. However, extremely elevated temperatures can cause cell and organ damage, and prolonged fever can cause dehydration.
Infection raises the metabolic rate, causing an increased heart rate. The respiratory rate may also increase as the body rids itself of carbon dioxide created during increased metabolism. However, be aware that an elevated heart rate above 90 and a respiratory rate above 20 are also criteria for systemic inflammatory response syndrome (SIRS) in clients with an existing infection.
As an infection develops, the lymph nodes that drain that area often become enlarged and tender. The swelling indicates that the lymphocytes and macrophages in the lymph node are fighting the infection. If a skin infection is developing, general signs of inflammation, such as redness, warmth, swelling, and tenderness, will occur at the site. As white blood cells migrate to the site, purulent drainage may occur.
Some viruses, bacteria, and toxins cause gastrointestinal inflammation, resulting in loss of appetite, nausea, vomiting, and diarrhea.
See Table 9.7a for a comparison of expected findings on physical assessment versus unexpected findings indicating a new infectious process that requires notification of the health care provider.
Table 9.7a Expected Versus Unexpected Findings on Assessment Related to Infection
| Assessment | Expected Findings | Unexpected Findings to Report to Health Care Provider |
|---|---|---|
| Vital Signs | Within normal range | New temperature over 100.4 F or 38 C. |
| Neurological | Within baseline level of consciousness | New or worsening confusion and/or worsening level of consciousness. |
| Wound or Incision | Progressive healing of a wound with no signs of infection | New or worsening redness, warmth, tenderness, or purulent drainage from a wound. |
| Respiratory | No cough or production of sputum | New or worsening cough and/or productive cough of purulent sputum. Adventitious breath sounds (crackles, rhonchi, wheezing). New or worsening dyspnea. |
| Genitourinary | Urine clear, light yellow without odor | Malodorous, cloudy, bloody urine, with increased frequency, urgency, or pain with urination. |
| Gastrointestinal | Good appetite and food intake; feces formed and brown | Loss of appetite. Nausea and vomiting. Diarrhea. Discolored or unusually malodorous feces. |
| *CRITICAL CONDITIONS requiring immediate notification of the provider and/or implementation of a sepsis protocol:
Two or more of the following criteria in a client with an existing infection indicate SIRS:
|
Life Span Considerations
Infants do not have well-developed immune systems, placing this group at higher risk of infection. Breastfeeding helps protect infants from some infectious diseases by providing passive immunity until their immune system matures. New mothers should be encouraged to breastfeed their newborns.[70]
On the other end of the continuum, the immune system gradually decreases in effectiveness with age, making older adults also more vulnerable to infection. Early detection of infection can be challenging in older adults because they may not have a fever or increased white blood cell count (WBC), but instead develop subtle changes like new mental status changes.[71] For example, new, acute confusion is a classic sign of urinary tract infection on older adults. The most common infections in older adults are urinary tract infections (UTI), bacterial pneumonia, influenza, and skin infections.
Diagnostic Tests
Several types of diagnostic tests may be ordered by a health care provider when a client is suspected of having an infection, such as complete blood count with differential, Erythrocyte Sedimentation Rate (ESR), C-Reactive Protein (CRP), serum lactate levels, and blood cultures (if sepsis is suspected). Other cultures may be obtained based on the site of the suspected infection.
CBC With Differential
When an infection is suspected, a complete blood count with differential is usually obtained.
A complete blood count (CBC) includes the red blood cell count (RBC), white blood cell count (WBC), platelets, hemoglobin, and hematocrit values. A differential provides additional information, including the relative percentages of each type of white blood cell. See Figure 9.22[72] for an illustration of a complete blood count with differential.
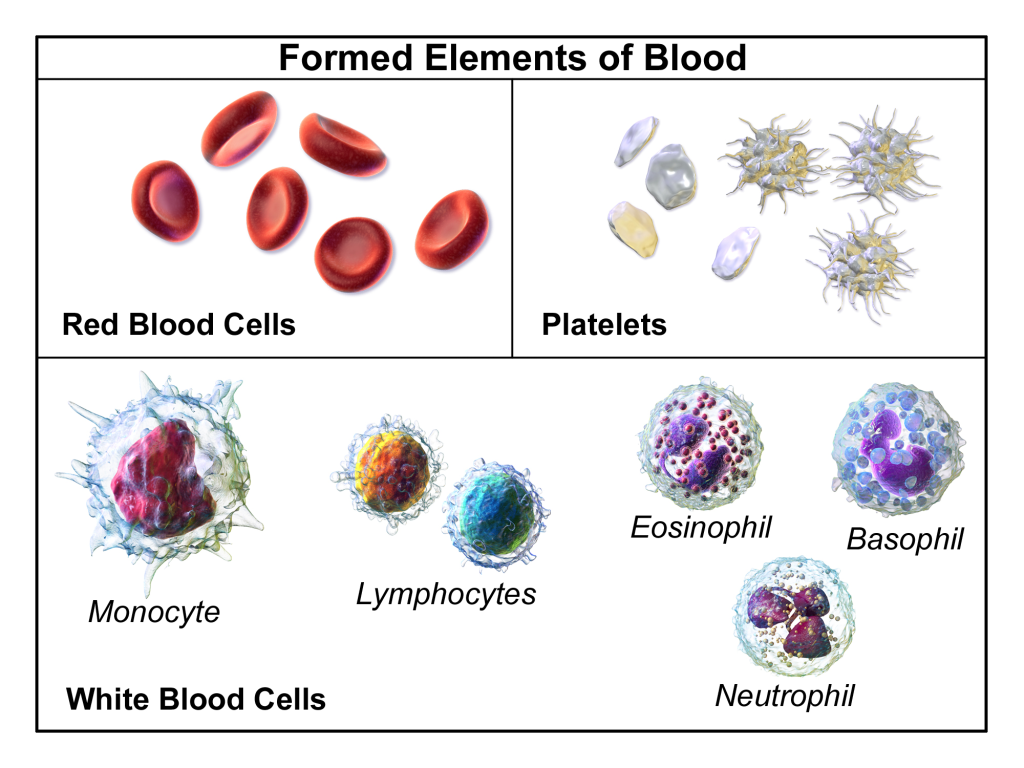
When there is an infection or an inflammatory process somewhere in the body, the bone marrow produces more WBCs (also called leukocytes), releasing them into the blood where they move to the site of infection or inflammation. An increase in white blood cells is known as leukocytosis and is a sign of the inflammatory response. The normal range of WBC varies slightly from lab to lab but is generally 4,500-11,000 for adults, reported as 4.5-11.0 x 109 per liter (L).[73]
There are five types of white blood cells, each with different functions. The differential blood count gives the relative percentage of each type of white blood cell and also reveals abnormal white blood cells. The five types of white blood cells are as follows:
- Neutrophils
- Eosinophils
- Basophils
- Lymphocytes
- Monocytes
Neutrophils make up the largest number of circulating WBCs. They move into an area of damaged or infected tissue where they engulf and destroy bacteria or sometimes fungi.[74] An elevated neutrophil count is called neutrophilia, and decreased neutrophil count is called neutropenia.[75]
Eosinophils respond to infections caused by parasites, play a role in allergic reactions (hypersensitivities), and control the extent of immune responses and inflammation. Elevated levels of eosinophils are referred to as eosinophilia.[76]
Basophils make up the fewest number of circulating WBCs and are thought to be involved in allergic reactions.[77]
Lymphocytes include three types of cells, although the differential count does not distinguish among them:
- B lymphocytes (B cells) produce antibodies that target and destroy bacteria, viruses, and other "non-self" foreign antigens.
- T lymphocytes (T cells) mature in the thymus and consist of a few different types. Some T cells help the body distinguish between "self" and "non-self" antigens; some initiate and control the extent of an immune response, boosting it as needed and then slowing it as the condition resolves; and other types of T cells directly attack and neutralize virus-infected or cancerous cells.
- Natural killer cells (NK cells) directly attack and kill abnormal cells such as cancer cells or those infected with a virus.[78]
Monocytes, similar to neutrophils, move to an area of infection and engulf and destroy bacteria. They are associated with chronic rather than acute infections. They are also involved in tissue repair and other functions involving the immune system.[79]
Care must be taken when interpreting the results of a differential. A health care provider will consider an individual's signs and symptoms and medical history, as well as the degree to which each type of cell is increased or decreased. A number of factors can cause a transient rise or drop in the number of any type of cell. For example, bacterial infections usually produce an increase in neutrophils, but a severe infection, like sepsis, can use up the available neutrophils, causing a low number to be found in the blood. Eosinophils are often elevated in parasitic and allergic responses. Acute viral infections often cause an increased level of lymphocytes (referred to as lymphocytosis).[80]
Erythrocyte Sedimentation Rate (ESR)
An Erythrocyte Sedimentation Rate (ESR) is a test that indirectly measures inflammation. This test measures how quickly erythrocytes or red blood cells (RBCs) settle at the bottom of a test tube that contains a blood sample. When a sample of blood is placed in a tube, the red blood cells normally settle out relatively slowly, leaving a small amount of clear plasma. The red cells settle at a faster rate when there is an increased level of proteins, such as C-reactive protein (CRP), that increases in the blood in response to inflammation. The ESR test is not diagnostic; it is a nonspecific test indicating the presence or absence of an inflammatory condition.[81]
C-Reactive Protein (CRP)
C-Reactive Protein (CRP) levels in the blood increase when there is a condition causing inflammation somewhere in the body. CRP is a nonspecific indicator of inflammation and one of the most sensitive acute phase reactants, meaning it is released into the blood within a few hours after the start of an infection or other causes of inflammation. The level of CRP can jump as much as a thousand-fold in response to a severe bacterial infection, and its rise in the blood can precede symptoms of fever or pain.[82]
Lactate
Serum lactate levels are measured when sepsis is suspected in a client with an existing infection. Sepsis can quickly lead to septic shock and death due to multi-organ failure so early recognition is crucial.
Lactate is one of the substances produced by cells as the body turns food into energy (i.e., cellular metabolism), with the highest level of production occurring in the muscles. Normally, the level of lactate in blood is low. Lactate is produced in excess by muscle cells and other tissues when there is insufficient oxygen at the cellular level, causing metabolism to change from aerobic (with oxygen) to anaerobic (without oxygen).
Lactic acid can accumulate in the body and blood when it is produced faster than the liver can break it down, which can lead to lactic acidosis. Excess lactate may be produced due to several medical conditions that cause decreased transport of oxygen to the tissues, such as sepsis, hypovolemic shock, necrotic bowel, heart attack, heart failure, or respiratory distress.[83]
Blood Culture
Blood cultures are ordered when sepsis is suspected. In many facilities, lab personnel draw the blood samples for blood cultures to avoid contamination of the sample. With some infections, pathogens are only found in the blood intermittently, so a series of three or more blood cultures, as well as blood draws from different veins, may be performed to increase the chance of finding the infection and to minimize false-positive cultures resulting from bacterial contamination of the site.
Blood cultures are incubated for several days before being reported as negative. Some types of bacteria and fungi grow more slowly than others and/or may take longer to detect if initially present in low numbers.
A positive result indicates bacteria have been found in the blood (bacteremia). Other types of pathogens, such as a fungus or a virus, may also be found in a blood culture. When a blood culture is positive, the specific microbe causing the infection is identified and susceptibility testing is performed to inform the health care provider which antibiotics or other medications are most likely to be effective for treatment.
It is important for nurses to remember that when new orders for both antibiotics and a blood culture are received, antibiotics should not be administered until after the blood culture is drawn. Administering antibiotics before the blood culture is drawn will impact the results and adversely affect the treatment plan.
Cultures and Other Diagnostic Tests
Several types of swabs and cultures may be ordered based on the site of a suspected infection, such as a nasal swab, nasopharyngeal swab, sputum culture, urine culture, and wound culture. If a lower respiratory tract infection is suspected, a chest X-ray may be ordered.
Read additional information about the following topics in Open RN Nursing Skills, 2e:
- "Specimen Collection"
- Collecting urine cultures in "Facilitation of Elimination"
- Collecting wound cultures in "Wound Care"
Therapeutic Drug Monitoring
When antibiotics are prescribed to treat an infection, some types of antibiotics require blood tests to ensure the dosage of the medication reaches and stays within therapeutic ranges in the blood. These tests are often referred to as peak and/or trough levels. A peak level refers to when the medication is at its highest concentration in the bloodstream. A trough level is when the medication is a the lowest concentration in the bloodstream, just prior to the next dose to be administered. The nurse must be aware of these orders because they impact the timing of administration of antibiotics.
Diagnoses
There are many NANDA-I nursing diagnoses applicable to infection. Nursing diagnoses associated with actual infections are customized based on the signs and symptoms of the specific infection (e.g., a client with pneumonia may have an actual nursing diagnosis of Ineffective Airway Clearance). Review a nursing care planning source for a list of current NANDA-I approved nursing diagnoses based on the type of infection occurring.[84]
Two common risk diagnoses are Risk for Infection for clients at risk for developing an infection and Risk for Shock for clients with an existing infection who are at risk for developing sepsis and septic shock. See Table 9.7b for the risk diagnoses of Risk for Infection and Risk for Shock.
Table 9.7b NANDA-I Diagnoses Associated with Infection
| NANDA-I Diagnosis | Definition | Other |
|---|---|---|
| Risk for Infection | Susceptible to invasion and multiplication of pathogenic organisms, which may compromise health
|
Risk Factors
|
| Risk of Shock | Susceptible to inadequate blood flow to the body’s tissues that may lead to life-threatening cellular dysfunction, which may compromise health
|
Associated Conditions
|
Examples
For example, a nurse caring for a client with an open wound assesses the wound regularly because clients with nonintact skin are always at increased risk for developing infection. A sample PES statement would be the following: "Risk for Infection as evidenced by alteration in skin integrity and insufficient knowledge to avoid exposure to pathogens." The nurse plans to provide client education regarding care of the wound to prevent bacterial contamination during dressing changes.
Whenever caring for a client with an existing infection, nurses know it is important to closely monitor for signs of developing SIRS and sepsis. A sample PES statement for a client with an existing infection is as follows: "Risk for Shock as evidenced by the associated condition of infection."
Note: Recall that in NANDA-I risk diagnoses, there are no etiological factors because a vulnerability reflects the potential for developing a problem. Read more about creating PES statements for risk diagnoses in the “Nursing Process” chapter.
Outcomes
An example of a broad goal for all clients is the following: “The client will remain free from infection during their health care stay.”[85]
An example of a SMART expected outcome to prevent infection is: “The client will demonstrate how to perform dressing changes using aseptic technique prior to discharge from the hospital.”[86]
Read more about creating SMART outcomes in the "Nursing Process" chapter.
Planning Interventions
When planning interventions for a client who is at risk for developing an infection, the nurse selects interventions such as those listed in the following box.
Interventions for Infection Prevention[87],[88]
- Monitor vital signs for signs of infection
- Monitor for early signs of localized and systemic infection for clients at risk
- Screen all visitors for communicable disease
- Encourage respiratory hygiene for clients, visitors, and staff members
- Maintain aseptic technique during nursing procedures
- Use sterile technique for invasive procedures or care of open wounds
- Use standard precautions with all clients to prevent the spread of infection
- Initiate transmission-based precautions for clients suspected of communicable infection, as appropriate
- Promote sufficient nutritional intake
- Encourage fluid intake, as appropriate
- Encourage rest
- Encourage frequent ambulation or turn immobilized clients frequently
- Ensure appropriate hygienic care, including proper hand hygiene, daily bathing, oral care, and perineal care performed by either the nurse or the client, as appropriate
- Moisturize dry skin to keep it intact
- Use strategies to prevent healthcare-acquired respiratory infection, such as incentive spirometry, coughing and deep breathing, positional changes, and early ambulation as appropriate
- Use strategies to prevent wound infection such as changing saturated dressings to reduce the potential reservoir of bacteria
- Teach the client and family members the importance of a nutritious diet, exercise, and adequate rest to promote healing and health at home
- Teach the client and family about signs and symptoms of infection and when to report them to the health care provider
- Encourage the annual influenza vaccine and keeping other recommended vaccinations up-to-date
- If a client smokes, encourage smoking cessation because smoking damages the mucociliary escalator and places the client at increased risk for infection
- Report signs and symptoms of suspected infection or sepsis to the health care provider
- Suspect an infection if an older adult client has new signs of lethargy or confusion
If a client has an infection with a fever, the nursing diagnosis Hyperthermia may be applicable. See the following box for interventions for clients with fever/hyperthermia.
Interventions for Hyperthermia
- Assess for associated symptoms such as diaphoresis, shaking chills (rigors)
- Monitor level of consciousness
- Adjust room temperature to the client’s comfort without inducing chilling
- Administer antipyretics, as appropriate (e.g., acetaminophen, ibuprofen)
- Apply external cooling methods as needed (cold packs or cool sponge bath)
- Encourage fluid intake
- Monitor for signs of dehydration
Implementing Interventions
When caring for a client with an active infection, transmission-based precautions may be required based on the specific type of pathogen. Antibiotics and/or other antimicrobials are administered as prescribed, and the client and family are instructed how to take prescribed antibiotics with measures to prevent antibiotic resistance (i.e., complete prescribed length of therapy even if they feel better in a few days).
If cultures have been obtained, it is important to monitor and report new results to the provider to ensure the prescribed antibiotic therapy is appropriate based on susceptibility results.
It is important to continually monitor clients with an existing infection for signs of SIRS/sepsis:
- Carefully monitor vital signs. Immediately notify the provider for two or more of the following indicators that suggest SIRS: heart rate greater than 90 beats per minute, temperature greater than 38 degrees C or less than 36 degrees C, systolic blood pressure less than 90 mm Hg, respiratory rate greater than 20, or a white blood cell count greater than 12,000 or less than 4,000.[89] Anticipate new orders for a lactate level and blood cultures for early diagnosis of sepsis.
- Monitor for signs of new decreased mental status, especially in older adults, that can indicate decreased oxygenation or tissue perfusion associated with sepsis and septic shock.
- For clients presenting with early signs of shock, administer oxygen immediately to maintain oxygen saturation greater than 90%. Administer prescribed antibiotics within an hour after diagnosis for improved survival. Be aware that IV fluids and vasopressor medications may be required to treat shock.[90]
Evaluation
It is always important to evaluate the effectiveness of interventions used to prevent and treat infection. Evaluation helps the nurse determine whether the established outcomes have been met and if the planned interventions are still appropriate for the client at the time of implementation. If outcomes are not met, interventions may need to be added or revised to help the client meet their goals.
Localized damage to the skin or underlying soft tissue, usually over a bony prominence, as a result of intense and prolonged pressure in combination with shear.

