Open Resources for Nursing (Open RN)
Distribution
The second stage of pharmacokinetics is the process known as distribution. Distribution is the process by which a drug is dispersed throughout the body’s blood and tissues. After a drug enters into systemic circulation by absorption or direct administration, it will pass from vascular spaces to tissues where a drug-receptor interaction will occur, creating the effect of the drug.
Drugs are designed to primarily cause one effect, meaning they bind more strongly to one specific receptor site and predictably cause or block an action. However, side effects and adverse effects can occur when the drug binds to other sites in addition to the target tissue, causing an unintended action. These side effects can range from tolerable to unacceptable and can result in the discontinuation of the medication. For example, a person might take the pain reliever ibuprofen (Advil) to treat a sore leg muscle, and the pain may be subsequently relieved, but there may also be stomach irritation as a side effect.
The distribution of a drug throughout the body is dependent on many body-related factors such as blood flow, tissue differences, plasma protein-binding, the blood-brain barrier, and the placental barrier.
Blood Flow
The circulatory system transports medications throughout the body in the bloodstream. Many factors can affect the blood flow and delivery of medication, such as decreased blood flow (due to dehydration), blocked vessels (due to atherosclerosis), constricted vessels (due to uncontrolled hypertension), or weakened pumping by the heart muscle (due to heart failure). As an example, when administering an antibiotic to a client with diabetes who has an infected toe, it may be difficult for the antibiotic to move through the blood vessels all the way to the area of the toe that is infected because of blocked vessels in the legs and feet due to atherosclerosis.
Tissue Differences
Distribution occurs most rapidly into tissues with a greater number of blood vessels that allow high blood flow (such as the lungs, kidneys, liver, brain). Distribution occurs least rapidly in tissues with fewer numbers of blood vessels (such as fat), resulting in low blood flow. However, lipophilic drugs (i.e., drugs that dissolve in lipid environments) disproportionately distribute into adipose tissue in obese subjects.
The permeability of capillaries is tissue-dependent. Capillaries of the liver and kidney are porous, allowing for greater permeability. Distribution rates are relatively slower or nonexistent into the central nervous system because of the tight junction between capillary endothelial cells and the blood-brain barrier.
Protein-Binding
After a drug enters the bloodstream, a portion of it exists as free drug, dissolved in plasma water, but a portion of it becomes bound to proteins. This is important because only free and unbound drugs will pass from the bloodstream to tissues where drug-receptor interactions will occur, thus producing the first effects of a medication. The other portion of the drug that becomes “protein-bound” is inactive while it is bound. For many drugs, these bound forms can account for 95-98% of the total.[1]
Protein binding can also act as a reservoir as the drug is released slowly, causing a prolonged action. When considering drug distribution, it is important to consider both the amount of free drug that is readily available to tissues, as well as the protein binding that causes the drug to be released over time.
Albumin is one of the most important proteins in the blood. Albumin levels can be decreased by several factors such as malnutrition and liver disease. Therefore, clients with low albumin levels may experience differences in the desired actions of administered medication because of the consequence effect on protein-binding and distribution.
Competition for plasma binding can also impact the effects of drugs. For example, aspirin and warfarin are anticoagulants that compete for the same plasma protein-binding site. Administering both drugs at the same time will increase the amount of unbound drug, thereby increasing their effects and increasing the client’s risk for bleeding.[2]

As an analogy of how protein binding affects the distribution of medications, consider passengers at a bus stop going to their destination. See Figure 1.4[3] for an image of a bus related to this analogy. Many passengers (i.e., drug molecules) want to take a ride on the bus. Everyone is eager to get to their destination (i.e., receptor sites) and tries to find a seat. Some passengers are stronger than others and take all the seats first (such as drug molecules with greater protein-binding ability). When there aren’t enough seats on the bus, some passengers are left at the bus stop and become “free” to move around or walk to their destination. In a similar way, “free” drug molecules that are not protein-bound circulate freely in the bloodstream. The “free” passengers in this analogy may go directly to their destination, or they may stop at other locations along the route. In a similar manner, “free” drug molecules produce the first intended or unintended effects in the body when they attach to receptors. Furthermore, similar to the passengers who had seats on the bus and then later got off at their destination, the medication molecules attached to proteins are eventually released and attach to the receptor sites.
Blood-Brain Barrier
Medications destined for the central nervous system (the brain and spinal cord) face an even larger hurdle than protein-binding; they must also pass through a nearly impenetrable barricade called the blood-brain barrier. This blockade is built from a tightly woven mesh of capillaries that protect the brain from potentially dangerous substances, such as poisons or viruses. Only certain medications made of lipids (fats) or those with a “carrier” can get through the blood-brain barrier.
Scientists have devised ways for medications to penetrate the blood-brain barrier. For example, the brand-named medication Sinemet® is a combination of two drugs: carbidopa and levadopa. Carbidopa is designed to carry the levadopa medication across the blood-brain barrier, where it enters the brain and is converted into dopamine to exert its effect on symptoms related to Parkinson’s disease.
Some medications inadvertently bypass the blood-brain barrier and impact an individual’s central nervous system function as a side effect. For example, diphenhydramine is an antihistamine used to decrease allergy symptoms. However, it can also cross the blood-brain barrier, depress the central nervous system, and cause the side effect of drowsiness. In the case of a person who has difficulty falling asleep, this drowsy side effect may be useful, but for a person trying to carry out daily activities, drowsiness can be problematic.
Placental Barrier
The placenta links mother and fetus, and the blood-placental barrier regulates transfer of molecules between maternal and fetal circulation to protect the fetus. Drug transporters are involved in transport of drugs through the placenta, affecting potential drug distribution to the fetus.[4] The placenta is known to be permeable to some medications, and furthermore, some drugs can cause significant harm to the fetus. However, many medications have not been specifically studied in pregnant clients and their effects on the fetus are unknown.
For this reason, it is always important to consider the potential effects of medication on the fetus if it is administered to a client who is pregnant or who may become pregnant. Nurses play a critical role in notifying the health care provider regarding potential safety concerns if medication can be distributed to the fetus. Nurses must always check a recent, evidence-based drug reference before administering medications to a client who is pregnant or may become pregnant. This imperative is implied in the remaining chapters.
Life Span Considerations
Neonate & Pediatric
Fat content in infants and children is decreased because of greater total body water. Additionally, protein-binding capacity is decreased, and the developing blood-brain barrier allows more drugs to enter the central nervous system.[5]
Older Adult
At the same body mass index, older adults, on average, tend to have more body fat than younger adults. This increased body fat can result in a longer duration of action for many medications that accumulate in fatty tissues. Serum albumin also decreases, resulting in more active free drug circulating within the body. For these reasons related to distribution, many older adult clients require lower dosages of medication.[6]
- This work is a derivative of StatPearls by Onetto and Sharif and is licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Onetto and Sharif and is licensed under CC BY 4.0 ↵
- “Renault Type r321 Service Bus” by Emslichter is licensed under CC0 1.0 ↵
- Liu, L., & Liu, X. (2019). Contributions of drug transporters to blood-placental barrier. Advances in Experimental Medicine and Biology, 1141, 505–548. https://doi.org/10.1007/978-981-13-7647-4_11 ↵
- Fernandez, E., Perez, R., Hernandez, A., Tejada, P., Arteta, M., & Ramos, J. T. (2011). Factors and mechanisms for pharmacokinetic differences between pediatric population and adults. Pharmaceutics, 3(1), 53–72. https://doi.org/10.3390/pharmaceutics3010053 ↵
- Fernandez, E., Perez, R., Hernandez, A., Tejada, P., Arteta, M., & Ramos, J. T. (2011). Factors and mechanisms for pharmacokinetic differences between pediatric population and adults. Pharmaceutics, 3(1), 53–72. https://doi.org/10.3390/pharmaceutics3010053 ↵
The American Nurses Association (ANA) is a professional organization that represents the interests of the nation's four million registered nurses and is at the forefront of improving the quality of health care for all.[1] The ANA establishes ethical and professional standards for nurses that also guide safe administration of medications. These code of ethics and professional standards are described in ANA publications titled Code of Ethics for Nurses and Nursing: Scope and Standards of Practice.
Code of Ethics for Nurses
The ANA developed the Code of Ethics for Nurses as a guide for carrying out nursing responsibilities in a manner consistent with quality in nursing care and the ethical obligations of the profession.[2] Several provisions from the Code of Ethics impact how nurses should administer medication in an ethical manner. A summary of each provision from the Code of Ethics and how it pertains to medication administration is outlined below:
- Provision 1 focuses on respect for human dignity and the right for self-determination: “The nurse practices with compassion and respect for the inherent dignity, worth, and unique attributes of every person.”
- Provision 2 states, “The nurse's primary commitment is to the client…”[3] In health care settings, nurses often experience several competing loyalties, such as to their employer, to the doctor(s), to their supervisor, or to others on the health care team. However, the client should always receive the primary commitment of the nurse. Additionally, the client has the right to accept, refuse, or terminate any treatment, including medications.
- Provision 3 states, “The nurse promotes, advocates for, and protects the rights, health, and safety of the patient...”[4] This provision includes a nurse's responsibility to promote a culture of safety for clients. If errors occur, they must be reported, and nurses should ensure responsible disclosure of errors to clients. This also includes proper disclosure of questionable practices, such as drug diversion or impaired practice by any professional.
- Provision 4 involves authority, accountability, and responsibility by a nurse to follow legal requirements, such as state practice acts and professional standards of care.
- Provision 5 includes the responsibility of the nurse to promote health and safety.
- Provision 6 focuses on virtues that make a nurse a morally good person. For example, nurses are held accountable to use their clinical judgment to avoid causing harm to clients (maleficence) and to do good (beneficence). When administering medications, nurses should validate the medication is doing more “good” than “harm” (adverse or side effects).
- Provision 7 focuses on a nurse practicing within the professional standards set forth by their state nurse practice act, as well as standards established by professional nursing organizations.
- Provision 8 explains that a nurse must address the social determinants of health, such as poverty, education, safe medication, and health care disparities.[5]
Whenever a nurse provides client care, the ANA's Code of Ethics should be used as a guide for professional ethical behavior.
View the ANA's Code of Ethics for Nurses.
Critical Thinking Activity 2.2a
A nurse is preparing to administer medications to a client. While reviewing the chart, the nurse notices two medications with similar mechanisms of action have been prescribed by two different providers.
What is the nurse's best response?
Note: Answers to the Critical Thinking activities can be found in the “Answer Key” sections at the end of the book.
Standards and Scope of Practice
The ANA publishes Nursing: Scope and Standards of Practice. This resource establishes national standards for nurses and is updated regularly.[6]
The ANA defines the scope of nursing as “the protection, promotion, and optimization of health and abilities, prevention of illness and injury, facilitation of healing, alleviation of suffering through the diagnosis and treatment of human response, and advocacy in the care of individuals, families, groups, communities, and populations.” A registered nurse (RN) is defined as an individual who is educationally prepared and licensed by a state to practice as a registered nurse. Nursing practice is characterized by the following tenets[7]:
- Caring and health are central to the practice of the registered nurse.
- Nursing practice is individualized to the unique needs of the health care consumer.
- Registered nurses use the nursing process to plan and provide individualized care for health care consumers.
- Nurses coordinate care by establishing partnerships to reach a shared goal of delivering safe, quality health care.
The ANA establishes Standards of Practice and Standards of Professional Performance in the Nursing: Scope and Standards of Practice publication. State nurse practice acts further define the scope of practice of RNs and Licensed Practical Nurses/Vocational Nurses (LPNs/VNs) within each state. Nurse practice acts are further discussed in the “Legal Foundations and National Guidelines for Safe Medication Administration” section of this chapter.
The ANA's Nursing: Scope and Standards of Practice publication can be purchased on the nursingworld.org website or borrowed from many libraries.
Standards of Practice
The ANA's Standards of Practice are authoritative statements of duties that all registered nurses, regardless of role, population, or specialty, are expected to perform competently. Standards of Practice include assessment, diagnosis, outcome identification, planning, implementation, and evaluation (ADOPIE) components of providing client care, also known as the "nursing process." When nurses safely administer medication, all components of ADOPIE are addressed.
Assessment
The "Assessment" Standard of Practice is defined as, “The registered nurse collects pertinent data and information relative to the health care consumer’s health or the situation.”[8] A registered nurse uses a systematic method to collect and analyze client data. Assessment includes physiological data, as well as psychological, sociocultural, spiritual, economic, and lifestyle data. For example, when a nurse assesses multiple pieces of data for a hospitalized client with pain, this is considered part of a comprehensive pain assessment.
Diagnosis
The "Diagnosis" Standard of Practice is defined as, “The registered nurse analyzes the assessment data to determine actual or potential diagnoses, problems, and issues.”[9] A nursing diagnosis is the nurse’s clinical judgment about the client's response to actual or potential health conditions or needs. Nursing diagnoses are used to create the nursing care plan and are different than medical diagnoses.[10]
Outcomes Identification
The "Outcomes Identification" Standard of Practice is defined as, “The registered nurse identifies expected outcomes for a plan individualized to the health care consumer or the situation.”[11] The nurse sets measurable and achievable short- and long-term goals and specific outcomes in collaboration with the client based on their assessment data and nursing diagnoses.
Planning
The "Planning" Standard of Practice is defined as, “The registered nurse develops a collaborative plan encompassing strategies to achieve expected outcomes.”[12] Assessment data, diagnoses, and goals are used to select evidence-based nursing interventions customized to each client’s needs and concerns. Goals, expected outcomes, and nursing interventions are documented in the client’s nursing care plan so that nurses, as well as other health professionals, have access to it for continuity of care.[13]
Implementation
The "Implementation" Standard of Practice is defined as, "The nurse implements the identified plan.”[14] Nursing interventions are implemented or delegated to licensed practical nurses/vocational nurses (LPNs/VNs) or unlicensed assistive personnel (UAP) with supervision. Interventions are also documented in the client’s electronic medical record as they are completed.[15]
The "Implementation" Standard of Professional Practice also includes the subcategories "Coordination of Care" and "Health Teaching and Health Promotion" to promote health and a safe environment.[16]
Coordination of Care
The ANA standard for coordination of care states, “The registered nurse coordinates care delivery.”[17] When ensuring medications are administered safely, the nurse collaborates with the client and the interprofessional health care team to meet mutually agreed upon outcomes. The nurse also engages the client in self-care to achieve their preferred goals for quality of life. For example, one client with chronic pain may have a pain management goal of "5" with their quality of life preference of having the ability to participate in social activities with friends but not experiencing burdensome side effect of medication. Another client with chronic pain may have a pain management goal of "0" with a quality of life preference of having no pain no matter what the side effects. The nurse advocates for these clients' goals and preferences with the interprofessional team.
Nurses also serve vital roles in ensuring safe transitions and continuity of care regarding clients' use of medications. Additional information about safe medication use and transitions of care is discussed in the "Preventing Medication Errors" section of this chapter.
Health Teaching and Health Promotion
When administering medications, nurses teach clients about the medications and potential side effects to promote optimal health. The ANA standard for health teaching and health promotion states, “The registered nurse employs strategies to teach and promote health and wellness.”[18] Specific behaviors related to teaching about medication are as follows[19]:
- Use health teaching and health promotion methods in collaboration with the client's values, beliefs, health practices, developmental level, learning needs, readiness and ability to learn, language preference, spirituality, culture, and socioeconomic status.
- Provide clients with information and education about intended effects and potential adverse effects of the plan of care.
- Provide anticipatory guidance to clients to promote health and prevent or reduce risk.
In the book Preventing Medication Errors by the Institute of Medicine (2007), the following are additional key national guidelines when teaching clients about safe use of their medications:
- Clients should maintain an active list of all prescription drugs, over-the-counter (OTC) drugs, and dietary supplements they are taking, the reasons for taking them, and any known drug allergies. Every provider involved in the medication-use process for a client should have access to this list.
- Clients should be provided information about side effects, contraindications, methods for handling adverse reactions, and sources for obtaining additional objective, high-quality information.[20]
Evaluation
The "Evaluation" Standard of Practice is defined as, “The registered nurse evaluates progress toward attainment of goals and outcomes.”[21] During evaluation, nurses assess the client and compare the findings against the initial assessment to determine the effectiveness of the interventions and overall nursing care plan. Both the client’s status and the effectiveness of the nursing care must be continuously evaluated and modified as needed.[22]
Read additional information about the nursing process in the "Nursing Process" chapter of Open RN Nursing Fundamentals.
Standards of Professional Performance
ANA's Standards of Professional Performance describe a competent level of behavior for nurses, including activities related to ethics, culturally congruent practice, communication, collaboration, leadership, education, evidence-based practice, and quality of practice.[23]
The ANA defines culturally congruent practice as the application of evidence-based nursing that is in agreement with the preferred cultural values, beliefs, worldview, and practices of the health care consumer and other stakeholders. Cultural competence represents the process by which nurses demonstrate culturally congruent practice. Nurses must assess the cultural beliefs and practices of their clients and implement culturally congruent interventions when administering medications and teaching about them. Additional information about cultural implications for medication administration is further discussed in the “Cultural and Social Determinants Related to Medication Administration” section later in this chapter.
Critical Thinking Activity 2.2b
A nurse is preparing to administer metoprolol, a cardiac medication, to a client and implements the nursing process:
ASSESSES the vital signs prior to administration and discovers the heart rate is 48.
DIAGNOSES that the heart rate is too low to safely administer the medication per the parameters provided. Establishes the OUTCOME to keep the client's heart rate within normal range of 60-100.
PLANS to call the provider, as well as report this incident in the shift handoff report.
Implements INTERVENTIONS by withholding the metoprolol at this time, documenting the incident that the medication is withheld, and notifying the provider.
Continues to EVALUATE the client status throughout the shift after not receiving the metoprolol.
The nurse is providing health teaching to a client about the medication before discharge. The nurse provides a handout with instructions, as well as a list of the current medications.
What other information should be provided to the client?
Note: Answers to the Critical Thinking activities can be found in the “Answer Key” sections at the end of the book.
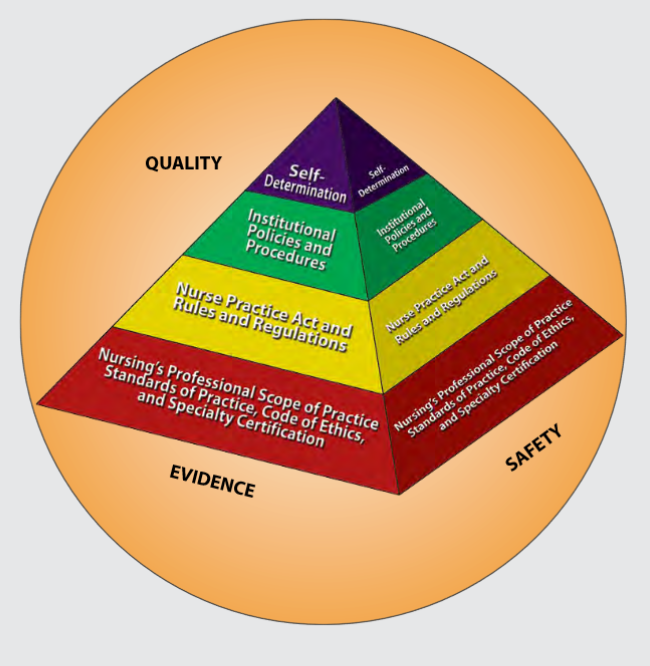
Figure 2.1 is an image from Nursing: Scope and Standards of Practice by the ANA that illustrates how the scope of practice, standards of practice, and code of ethics form the “base” of nursing practice.[24] Nursing practice is further guided by the Nurse Practice Act in the state in which a nurse works, federal and state rules and regulations, institutional policies and procedures, and self-determination by the individual nurse. All these components are required to provide quality, safe client care that is evidence-based. These components will be further discussed in the remaining sections of this chapter.
NCLEX and the Clinical Judgment Model
The National Council Licensure Examination (NCLEX) is the national exam that graduates must pass successfully to obtain their nursing license after graduating from a nursing program of study. The NCLEX-PN is taken to become a licensed practical/vocational nurse (LPN/VN), and the NCLEX-RN is taken to become a licensed registered nurse (RN). The purpose of the NCLEX is to evaluate if a nursing graduate demonstrates the ability to provide safe, competent, entry-level nursing care. The NCLEX is developed by the National Council of State Boards of Nursing (NCSBN), an independent, nonprofit organization composed of the 50 state boards of nursing and other regulatory agencies.[25]
A new edition of the NCLEX was launched in April 2023 that contains “Next Generation” questions. The Next Generation NCLEX (NGN) assesses how well the candidate can think critically and use clinical judgment. The NCSBN defines clinical judgment as "the observed outcome of critical thinking and decision-making. It is an iterative process with multiple steps that uses nursing knowledge to observe and assess presenting situations, identify a prioritized client concern and generate the best possible evidence-based solutions in order to deliver safe client care."
The NCLEX uses the NCSBN's Clinical Judgment Measurement Model (NCJMM) to assess the candidate's ability to use safe clinical judgment when providing nursing care. Exam questions used to assess clinical judgment may be contained in a case study or as individual stand-alone items. A case study contains six questions that are associated with the same client scenario and addresses the following steps in clinical judgment[26]:
- Recognize cues: Identify relevant and important information from different sources (e.g., medical history, vital signs).
- Analyze cues: Organize and connect the recognized cues to the client’s clinical presentation.
- Prioritize hypotheses: Evaluate and prioritize hypotheses (based on urgency, likelihood, risk, difficulty, time constraints, etc.).
- Generate solutions: Identify expected outcomes and use hypotheses to define a set of interventions for the expected outcomes.
- Take action: Implement the solution(s) that address the highest priority.
- Evaluate outcomes: Compare observed outcomes to expected outcomes.
Throughout this book, learning activities are provided to assist students in learning how to apply the nursing process (i.e., ANA's Standards of Care) to answer NGN-style questions that evaluate clinical judgment. Some of these activities are written, with answers in the Answer Key at the end of the book, and others are interactive and require use of the online book.

