Open Resources for Nursing (Open RN)
Urinary incontinence is the involuntary loss of urine. Although abnormal, it is a common symptom that can seriously affect the physical, psychological, and social well-being of affected individuals of all ages. It has been estimated that 1 in 5 women develop urinary incontinence, but many are too embarrassed to discuss the condition with their health care providers. Some believe it’s a normal part of aging that they have to live with. The result can be isolation and depression when they limit their activities and social interactions because of embarrassment due to incontinence. Nurses can greatly improve the quality of life for these clients by assessing for incontinence in a sensitive manner and then providing health teaching about methods to prevent and/or manage incontinence.
Types of Urinary Incontinence
Continence is achieved through an interplay of the physiology of the bladder, urethra, sphincter, pelvic floor, and the nervous system coordinating these organs.[1] A disruption in any of these areas can cause several types of urinary incontinence.
- Stress urinary incontinence is the involuntary loss of urine with intra-abdominal pressure (e.g., laughing and coughing) or physical exertion (e.g., jumping). It is caused by weak pelvic floor muscles that is often the result of pregnancy and vaginal delivery, menopause, and vaginal hysterectomy.[2]
- Urge urinary incontinence (also referred to as “overactive bladder”) is urine leakage caused by the sensation of a strong desire to void (urgency). It can be caused by increased sensitivity to stimulation by the detrusor muscle in the bladder or decreased inhibitory control of the central nervous system.[3]
- Mixed urinary incontinence is a mix of urinary frequency, urgency, and stress incontinence.[4]
- Overflow incontinence occurs when small amounts of urine leak from a bladder that is always full. This condition tends to occur in males with enlarged prostates that prevent the complete emptying of the bladder.[5]
- Functional incontinence occurs in older adults who have normal bladder control but have a problem getting to the toilet because of arthritis or other disorders that make it hard to move quickly or manipulate zippers or buttons. Clients with dementia also have increased risk for functional incontinence.
It is important for nurses to understand the different types of incontinence so that appropriate interventions can be targeted to the cause.
Assessment of Incontinence
Assessment begins with screening questions during a health history, including questions such as, “Do you have any problems with the leakage or dribbling of urine? Do you ever have problems making it to the bathroom in time?” If a client responds “Yes” to either of these questions, it is helpful to encourage them to start a voiding diary to record their urination habits and activities. The voiding diary should include the following[6]:
- When and how much the client urinates
- Urinary leakage and what the client was doing when it happened (for example, running, biking, laughing)
- Sudden urges to urinate
- How often the client wakes at night to use the bathroom
- Type and volume of food and beverages and the time of intake
- Medication use, such as diuretics, and the timing of administration
- Any pain or problems experienced before, during, and after urinating (for example, sudden urges, difficulty urinating, dribbling urine, feeling as if the bladder is never empty, weak urine flow).
The provider will review information from the voiding diary, perform a physical assessment, and likely order diagnostic testing, such as a urine dip to check for a urinary tract infection, and urodynamic diagnostic testing that includes a variety of tests about bladder function, including filling, urine storage, and emptying.[7] Individualized treatment will be based on the assessment and tests to assess any structural abnormalities and bladder function.
Interventions
Nurses should use therapeutic communication with clients experiencing urinary incontinence to help them feel comfortable in expressing their fears, worries, and embarrassment about incontinence and work toward improving their quality of life. Let them know they’re not alone and that urinary incontinence is not something they have to live with. Provide education about pelvic floor muscle training exercises, timed voiding, lifestyle modification, and incontinence products. Encourage them to learn more about their condition so they can optimally manage it and improve their quality of life.[8]
Nurses play an important role in educating clients about bladder control training to prevent incontinence. Bladder control training includes several these techniques:
- Pelvic muscle exercises (also known as Kegel exercises) work the muscles used to stop urination, which can help prevent stress incontinence. Learn more about pelvic floor exercises in the box below.
- Timed voiding can be used to help a client regain control of the bladder. Timed voiding encourages the client to urinate on a set schedule, for example, every hour, whether they feel the urge to urinate or not. The time between bathroom trips is gradually extended with the general goal of achieving four hours between voiding. Timed voiding helps to control urge and overflow incontinence as the brain is trained to be less sensitive to the sensation of the bladder walls expanding as they fill.[9]
- Lifestyle changes can help with incontinence. Losing weight, drinking less caffeine (found in coffee, tea, and many sodas), preventing constipation, and avoiding lifting heavy objects may help with incontinence. Limiting fluid intake before bedtime and scheduling prescribed diuretic medication in the morning or early afternoon are also helpful.[10]
- Protective products may be needed to protect the skin from breakdown and prevent leakage onto clothing. Incontinence underwear has a waterproof liner and built-in cloth pad to absorb large amounts of urine to protect skin from moisture and control odor. It is available in daytime and nighttime styles (designed to hold more urine). A product resembling a tampon is another option for females. It is made of absorbent fibers that support the urethra and prevents accidental leaks but doesn’t inhibit urination and won’t move or fall out during bowel movements.[11]
Teaching Pelvic Floor Exercises
Kegel exercises are designed to make your pelvic floor muscles stronger. Your pelvic floor muscles hold up your bladder and prevent it from leaking urine.
- Start by finding the right muscles. There are two easy ways to do this: stop the stream of urine as you are urinating or imagine that you are trying to stop the passage of gas. Squeeze the muscles you would use to do both. If you sense a “pulling” feeling, you are squeezing the right muscles for pelvic exercises. Many people have trouble finding the right muscles. A doctor, nurse, or therapist can check to make sure you are doing the exercises correctly and targeting the correct muscles.
- Find a quiet spot to practice so you can concentrate. Lie on the floor. Pull in the pelvic muscles and hold for a count of 3. Then relax for a count of 3. Work up to 10 to 15 repeats each time you exercise.
- Complete pelvic exercises at least three times a day. Try to use three different positions while performing the exercises: lying down, sitting, and standing. For example, you can exercise while lying on the floor, sitting at a desk, or standing in the kitchen. Using all three positions while exercising makes these muscles their strongest.
- Be patient. Most people notice an improvement after a few weeks, but the maximum effect may take up to 3-6 weeks.
View a YouTube video about Kegel Exercises[12] from Michigan Medicine.
Health teaching regarding other treatment options may be provided:
- Biofeedback uses sensors to help a client become more aware of signals from the body to regain control over the muscles in their bladder and urethra.[13]
- Mechanical devices, such as pessaries, support the urethra and can support vaginal prolapse to prevent or reduce urinary leakage. They come in various sizes and are professionally fitted by trained health care providers. They should be removed, cleaned, and reinserted regularly to prevent infection. Some of the devices, such as ring pessaries, can be removed and reinserted by the client. They are similar to a diaphragm and can be removed or left in place for sexual intercourse.[14]
- Anticholinergic medications, such as oxybutynin, may be prescribed to treat urge urinary incontinence and mixed urinary incontinence. They block the action of acetylcholine and provide an antispasmodic effect on smooth muscle to relieve symptoms. However, side effects include dry mouth, constipation, dizziness, and drowsiness, which can increase fall risk in older adults.
- If bladder training and medications are not effective, surgery may be performed, such as a sling procedure or a bladder neck suspension.[15]
- McClurg, D., Pollock, A., Campbell, P., Hazelton, C., Elders, A., Hagen, S., & Hill, D. C. (2016). Conservative interventions for urinary incontinence in women: An overview of Cochrane systematic reviews. The Cochrane Database of Systematic Reviews, 2016(9). https://doi.org/10.1002/14651858.CD012337 ↵
- Tso, C. (2018, January 10). Postmenopausal women and urinary incontinence. American Nurse. https://www.myamericannurse.com/postmenopausal-women-urinary-incontinence/ ↵
- Tso, C. (2018, January 10). Postmenopausal women and urinary incontinence. American Nurse. https://www.myamericannurse.com/postmenopausal-women-urinary-incontinence/ ↵
- Tso, C. (2018, January 10). Postmenopausal women and urinary incontinence. American Nurse. https://www.myamericannurse.com/postmenopausal-women-urinary-incontinence/ ↵
- National Institute of Aging. (2017, May 16). Urinary incontinence in older adults. U.S. Department of Health & Human Services. https://www.nia.nih.gov/health/urinary-incontinence-older-adults ↵
- Tso, C. (2018, January 10). Postmenopausal women and urinary incontinence. American Nurse. https://www.myamericannurse.com/postmenopausal-women-urinary-incontinence/ ↵
- Tso, C. (2018, January 10). Postmenopausal women and urinary incontinence. American Nurse. https://www.myamericannurse.com/postmenopausal-women-urinary-incontinence/ ↵
- Tso, C. (2018, January 10). Postmenopausal women and urinary incontinence. American Nurse. https://www.myamericannurse.com/postmenopausal-women-urinary-incontinence/ ↵
- National Institute of Aging. (2017, May 16). Urinary incontinence in older adults. U.S. Department of Health & Human Services. https://www.nia.nih.gov/health/urinary-incontinence-older-adults ↵
- National Institute of Aging. (2017, May 16). Urinary incontinence in older adults. U.S. Department of Health & Human Services. https://www.nia.nih.gov/health/urinary-incontinence-older-adults ↵
- National Institute of Aging. (2017, May 16). Urinary incontinence in older adults. U.S. Department of Health & Human Services. https://www.nia.nih.gov/health/urinary-incontinence-older-adults ↵
- Michigan Medicine. (2016, September 14). Better kegels: How to do kegel exercises, and why they work [Video]. YouTube. All rights reserved. https://youtu.be/7C8uoq98x2A ↵
- National Institute of Aging. (2017, May 16). Urinary incontinence in older adults. U.S. Department of Health & Human Services. https://www.nia.nih.gov/health/urinary-incontinence-older-adults ↵
- National Institute of Aging. (2017, May 16). Urinary incontinence in older adults. U.S. Department of Health & Human Services. https://www.nia.nih.gov/health/urinary-incontinence-older-adults ↵
- National Institute of Aging. (2017, May 16). Urinary incontinence in older adults. U.S. Department of Health & Human Services. https://www.nia.nih.gov/health/urinary-incontinence-older-adults ↵
Before discussing assessments and interventions related to promoting good nutrition, let’s review the structure and function of the digestive system, essential nutrients, and nutritional guidelines.
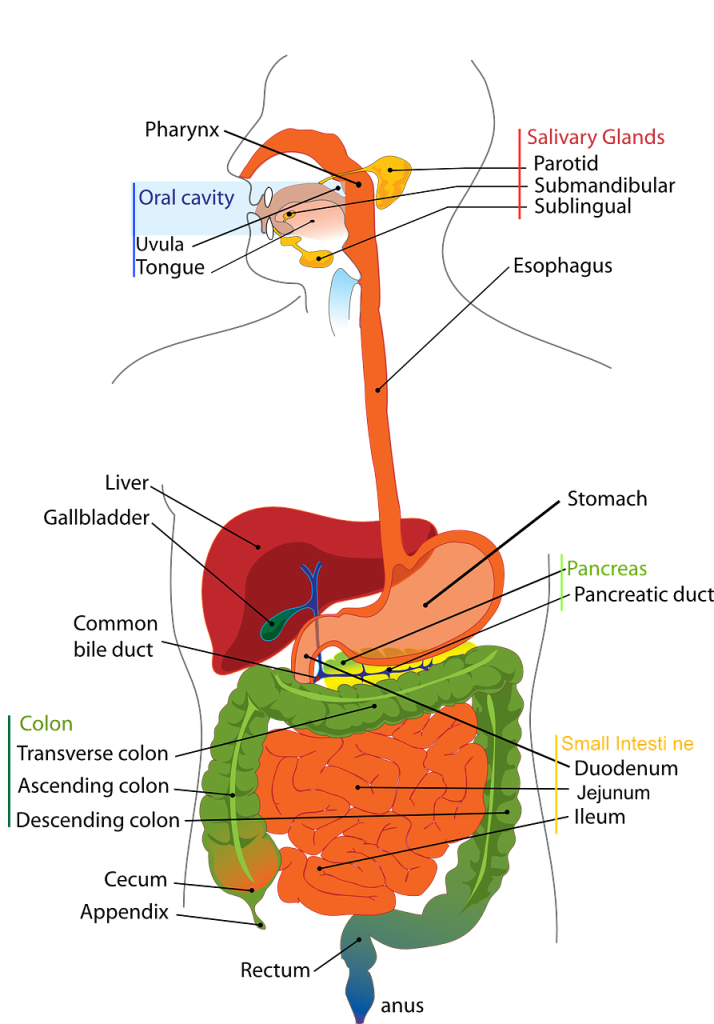
Digestive System
The digestive system breaks down food and then absorbs nutrients into the bloodstream via the small intestine and large intestine. Because good health depends on good nutrition, any disorder affecting the functioning of the digestive system can significantly impact overall health and well-being and increase the risk of chronic health conditions.
Structure and Function
The gastrointestinal system (also referred to as the digestive system) is responsible for several functions, including digestion, absorption, and immune response. Digestion begins in the upper gastrointestinal tract at the mouth, where chewing of food occurs, called mastication. Mastication results in mechanical digestion when food is broken down into small chunks and swallowed. Masticated food is formed into a bolus as it moves toward the pharynx in the back of the throat and then into the esophagus. Coordinated muscle movements in the esophagus called peristalsis move the food bolus into the stomach where it is mixed with acidic gastric juices and further broken down into chyme through a chemical digestion process. As chyme is moved out of the stomach and into the duodenum of the small intestine, it is mixed with bile from the gallbladder and pancreatic enzymes from the pancreas for further digestion.[1]
Absorption is a second gastrointestinal function. After chyme enters the small intestine, it comes into contact with tiny fingerlike projections along the inside of the intestine called villi. Villi increase the surface area of the small intestine and allow nutrients, such as protein, carbohydrates, fat, vitamins, and minerals, to absorb through the intestinal wall and into the bloodstream. Absorption of nutrients is essential for metabolism to occur because nutrients fuel bodily functions and create energy. Peristalsis moves leftover liquid from the small intestine into the large intestine, where additional water and minerals are absorbed. Waste products are condensed into feces and excreted from the body through the anus.[2] See Figure 14.1[3] for labeled parts of the gastrointestinal system.
In addition to digestion and absorption, the gastrointestinal system is also involved in immune function. Good bacteria in the stomach create a person’s gut biome. Gut biome contributes to a person’s immune response through antibody production in response to foreign materials, chemicals, bacteria, and other substances.[4] For example, clients may develop Clostridium difficile (C-diff) after taking antibiotics that kill these beneficial bacteria in the gut. Read additional details about our microbiome and immune response in the “Infection” chapter of this book.
Essential Nutrients
Nutrients from food and fluids are used by the body for growth, energy, and bodily processes. Essential nutrients refer to nutrients that are necessary for bodily functions but must come from dietary intake because the body is unable to synthesize them. Essential nutrients include vitamins, minerals, some amino acids, and some fatty acids.[5] Essential nutrients can be further divided into macronutrients and micronutrients.
Macronutrients
Macronutrients make up most of a person’s diet and provide energy, as well as essential nutrient intake. Macronutrients include carbohydrates, proteins, and fats. However, too many macronutrients without associated physical activity cause excess nutrition that can lead to obesity, cardiovascular disease, diabetes mellitus, kidney disease, and other chronic diseases. Too few macronutrients result in undernutrition, which contributes to nutrient deficiencies and malnourishment.[6]
Carbohydrates
Carbohydrates are sugars and starches and are an important energy source that provides 4 kcal/g of energy. Simple carbohydrates are small molecules (called monosaccharides or disaccharides) and break down quickly. As a result, simple carbohydrates are easily digested and absorbed into the bloodstream, so they raise blood glucose levels quickly. Examples of simple carbohydrates include table sugar, syrup, soda, and fruit juice. Complex carbohydrates are larger molecules (called polysaccharides) that break down more slowly, which causes slower release into the bloodstream and a slower increase in blood sugar over a longer period of time. Examples of complex carbohydrates include whole grains, beans, and vegetables.[7]
Foods can also be categorized according to their glycemic index, a measure of how quickly glucose levels increase in the bloodstream after carbohydrates are consumed. The glycemic index was initially introduced as a way for people with diabetes mellitus to control their blood glucose levels. For example, processed foods, white bread, white rice, and white potatoes have a high glycemic index. They quickly raise blood glucose levels after being consumed and also cause the release of insulin, which can result in more hunger and overeating. However, foods such as fruit, green leafy vegetables, raw carrots, kidney beans, chickpeas, lentils, and bran breakfast cereals have a low glycemic index. These foods minimize blood sugar spikes and insulin release after eating, which leads to less hunger and overeating. Eating a diet of low glycemic foods has been linked to a decreased risk of obesity and diabetes mellitus.[8] See Figure 14.2[9] for an image of the glycemic index of various foods.

Proteins
Proteins are peptides and amino acids that provide 4 kcal/g of energy. Proteins are necessary for tissue repair and function, growth, energy, fluid balance, clotting, and the production of white blood cells. Protein status is also referred to as nitrogen balance. Nitrogen is consumed in dietary intake and excreted in the urine and feces. If the body excretes more nitrogen than it takes in through the diet, this is referred to as a negative nitrogen balance. Negative nitrogen balance is seen in clients with starvation or severe infection. Conversely, if the body takes in more nitrogen through the diet than what is excreted, this is referred to as a positive nitrogen balance.[10] During positive nitrogen balance, excess protein is converted to fat tissue for storage.
Proteins are classified as complete, incomplete, or partially complete. Complete proteins must be ingested in the diet. They have enough amino acids to perform necessary bodily functions, such as growth and tissue maintenance. Examples of foods containing complete proteins are soy, quinoa, eggs, fish, meat, and dairy products. Incomplete proteins do not contain enough amino acids to sustain life. Examples of incomplete proteins include most plants, such as beans, peanut butter, seeds, grains, and grain products. Incomplete proteins must be combined with other types of proteins to add to amino acids and form complete protein combinations.[11] For example, vegetarians must be careful to eat complementary proteins, such as grains and legumes, or nuts and seeds and legumes, to create complete protein combinations during their daily food intake. Partially complete proteins have enough amino acids to sustain life, but not enough for tissue growth and maintenance. Because of the similarities, most sources consider partially complete proteins to be in the same category as incomplete proteins. See Figure 14.3[12] for an image of protein-rich foods.

Fats
Fats consist of fatty acids and glycerol and are essential for tissue growth, insulation, energy, energy storage, and hormone production. Fats provide 9 kcal/g of energy.[13] While some fat intake is necessary for energy and uptake of fat-soluble vitamins, excess fat intake contributes to heart disease and obesity. Due to its high-energy content, a little fat goes a long way.
Fats are classified as saturated, unsaturated, and trans fatty acids. Saturated fats come from animal products, such as butter and red meat (e.g., steak). Saturated fats are solid at room temperature. Recommended intake of saturated fats is less than 10% of daily calories because saturated fat raises cholesterol and contributes to heart disease.[14]
Unsaturated fats come from oils and plants, although chicken and fish also contain some unsaturated fats. Unsaturated fats are healthier than saturated fats. Examples of unsaturated fats include olive oil, canola oil, avocados, almonds, and pumpkin seeds. Fats containing omega-3 fatty acids are considered polyunsaturated fats and help lower LDL cholesterol levels. Fish and other seafood are excellent sources of omega-3 fatty acids.
Trans fats are fats that have been altered through a hydrogenation process, so they are not in their natural state. During the hydrogenation process, fat is changed to make it harder at room temperature and have a longer shelf life. Trans fats are found in processed foods, such as chips, crackers, and cookies, as well as in some margarines and salad dressings. Minimal trans-fat intake is recommended because it increases cholesterol and contributes to heart disease.[15]
Micronutrients
Micronutrients include vitamins and minerals.
Vitamins
Vitamins are necessary for many bodily functions, including growth, development, healing, vision, and reproduction. Most vitamins are considered essential because they are not manufactured by the body and must be ingested in the diet. Vitamin D is also manufactured through exposure to sunlight.[16]
Vitamin toxicity can be caused by overconsumption of certain vitamins, such as vitamins A, D, C, B6, and niacin. Conversely, vitamin deficiencies can be caused by various factors, including poor food intake due to poverty, malabsorption problems with the gastrointestinal tract, drug and alcohol abuse, proton pump inhibitors, and prolonged parenteral nutrition. Deficiencies can take years to develop, so it is usually a long-term problem for clients.[17]
Vitamins are classified as water soluble or fat soluble. Water-soluble vitamins are not stored in the body and include vitamin C and B-complex vitamins: B1 (thiamine), B2 (riboflavin), B3 (niacin), B6 (pyridoxine), B12 (cyanocobalamin), and B9 (folic acid). Additional water-soluble vitamins include biotin and pantothenic acid. Excess amounts of these vitamins are excreted through the kidneys in urine, so toxicity is rarely an issue, though excess intake of vitamin B6, C, or niacin can result in toxicity.[18] See Table 14.2a for a list of selected water-soluble vitamins, their sources, and their function.[19],[20],[21],[22],[23],[24],[25],[26],[27]
Table 14.2a Selected Water-Soluble Vitamins
| Water-Soluble Vitamin | Sources | Functions | Deficiency |
|---|---|---|---|
| C (Ascorbic Acid) | Citrus fruits, broccoli, greens, sweet peppers, tomatoes, lettuce, potatoes, tropical fruits, and strawberries | Infection prevention, wound healing, collagen formation, iron absorption, amino acid metabolism, antioxidant, and bone growth in children. | Early Signs: weakness, weight loss, myalgias, and irritability. Late Signs: scurvy; swollen, spongy gums; loose teeth; bleeding gums and skin; poor wound healing; edema; leg pain; anorexia; irritability; and poor growth in children. |
| B1 (Thiamine) | Nuts, liver, whole grains, pork, and legumes | Nerve function; metabolism of carbohydrates, fat, amino acids, glucose, and alcohol; appetite and digestion. | Fatigue, memory deficits, insomnia, chest pain, abdominal pain, anorexia, numbness of extremities, muscle wasting, heart failure, and shock in severe cases. |
| B2 (Riboflavin) | Eggs, liver, leafy greens, milk, and whole grains | Protein and carbohydrate metabolism, healthy skin, and normal vision. | Pallor, lip fissures, and seborrheic dermatitis. |
| B3 (Niacin) | Fish, chicken, eggs, dairy, mushrooms, peanut butter, whole grains, and red meat | Glycogen metabolism, cell metabolism, tissue regeneration, fat synthesis, nerve function, digestion, and skin health. | Pellagra characterized by skin lesions at pressure points/sun exposed skin, glossitis (swollen tongue), constipation progressing to bloody diarrhea, abdominal pain, abdominal distention, nausea, psychosis, and encephalopathy. |
| B6 (Pyridoxine) | Organ meats, fish, and various fruits and vegetables | Protein metabolism and red blood cell formation. | Rare due to presence in most foods. Peripheral neuropathy, seizures refractory to antiseizure medications, anemia, glossitis (swollen tongue), seborrheic dermatitis, depression, and confusion. |
| B9 (Folic Acid) | Liver, legumes, leafy greens, seeds, orange juice, and enriched refined grains | Coenzyme in protein metabolism and cell growth, red blood cell formation, and prevention of fetal neural tube defects in utero. | Glossitis (swollen tongue), confusion, depression, diarrhea, anemia, and fetal neural tube defects. |
| B12 (Cyanocobalamin) | Meat, organ meat, dairy, seafood, poultry, and eggs | Mature red blood cell formation, DNA/RNA synthesis, new cell formation, and nerve function. | Pernicious anemia from lack of intrinsic factor in intestines. Early Signs: weight loss, abdominal pain, peripheral neuropathy, weakness, hyporeflexia, and ataxia. Late Signs: irritability, depression, paranoia, and confusion. |
Fat-soluble vitamins are absorbed with fats in the diet and include vitamins A, D, E, and K. They are stored in fat tissue and can build up in the liver. They are not excreted easily by the kidneys due to storage in fatty tissue and the liver, so overconsumption can cause toxicity, especially with vitamins A and D.[28] See Table 14.2b for a list of selected fat-soluble vitamins, their sources, their function, and manifestations of deficiencies and toxicities.[29],[30],[31],[32],[33],[34],[35],[36],[37]
Table 14.2b Selected Fat-Soluble Vitamins
| Fat-Soluble Vitamin | Source | Function | Deficiency | Toxicity |
|---|---|---|---|---|
| A (Retinol)
|
Retinol: fortified milk and dairy, egg yolks, and fish liver oil
Beta carotene: green leafy vegetables, and dark orange fruits and vegetables |
Eyesight, epithelial, bone and tooth development, normal cellular proliferation, and immunity. | Night blindness, rough scaly skin, dry eyes, and poor tooth/ bone development. Causes poor growth and infections common with mortality >50%. | Dry, itchy skin; headache; nausea; blurred vision; and yellowing skin (carotenosis). |
| D | Milk, dairy, sun exposure, egg yolks, fatty fish, and liver | Changed to active form with sun exposure. Needed for calcium/ phosphorus absorption, immunity, and bone strength. | Rickets, poor dentition, tetany, osteomalacia, muscle aches and weakness, bone pain, poor calcium absorption leading to hypocalcemia and subsequent hyperparathyroidism and tetany. | Hypercalcemia resulting in nausea, vomiting, anorexia, renal failure, weakness, pruritus, and polyuria. |
| E | Green leafy vegetables, whole grains, liver, egg yolks, nuts, and plant oils | Anticoagulant, antioxidant, and cellular protection. | Red blood cell breakdown leading to anemia, neuron degeneration, neuropathy, and retinopathy. | Rare. Occasionally muscle weakness, fatigue, GI upset with diarrhea, and hemorrhagic stroke. |
| K | Green leafy vegetables and green vegetables
*Produced by bacteria in intestines |
Needed for producing clotting factors in the liver. | Rare in adults. Prolonged clotting times, hemorrhaging (especially in newborns causing morbidity & mortality), and jaundice. | Rare, but can interfere with effectiveness of certain anticoagulant medications (Warfarin). |
Minerals
Minerals are inorganic materials essential for hormone and enzyme production, as well as for bone, muscle, neurological, and cardiac function. Minerals are needed in varying amounts and are obtained from a well-rounded diet. In some cases of deficiencies, mineral supplements may be prescribed by a health care provider. Deficiencies can be caused by malnutrition, malabsorption, or certain medications, such as diuretics.
Minerals are classified as either macrominerals or trace minerals. Macrominerals are needed in larger amounts and are typically measured in milligrams, grams, or milliequivalents. Macrominerals include sodium, potassium, calcium, magnesium, chloride, and phosphorus. Macrominerals are discussed in further detail in the "Electrolytes" section of the “Fluids and Electrolytes” chapter of this book.
Trace minerals are needed in tiny amounts. Trace minerals include zinc, iron, chromium, copper, fluorine, iodine, manganese, molybdenum, and selenium.[38] See Table 14.2c for a list of selected macrominerals and Table 14.2d for a list of trace minerals.[39],[40],[41],[42]
Table 14.2c Macrominerals
| Macromineral | Source | Function |
|---|---|---|
| Sodium | Table salt, spinach, and milk | Water balance |
| Potassium | Legumes, potatoes, bananas, and whole grains | Muscle contraction, cardiac muscle function, and nerve function |
| Calcium | Dairy, eggs, and green leafy vegetables | Bone and teeth development, nerve function, muscle contraction, immunity, and blood clotting |
| Magnesium | Raw nuts, spinach (cooked has higher magnesium content), tomatoes, and beans | Cell energy, muscle function, cardiac function, and glucose metabolism |
| Chloride | Table salt | Fluid and electrolyte balance and digestion |
| Phosphorus | Red meat, poultry, rice, oats, dairy, and fish | Bone strength and cellular function |
Table 14.2d Trace Minerals
| Trace Mineral | Source | Function |
|---|---|---|
| Zinc | Eggs, spinach, yogurt, whole grains, fish, and brewer’s yeast | Immune function, healing, and vision |
| Iron | Red meat, organ meats, spinach, shrimp, tuna, salmon, kidney beans, peas, and lentils (nonanimal forms are harder to absorb, so need more!) | Hemoglobin production and collagen production |
| Chromium | Whole grains, meat, and brewer’s yeast | Glucose metabolism |
| Copper | Shellfish, fruits, nuts, and organ meats | Hemoglobin production, collagen, elastin, neurotransmitter production, and melanin production |
| Fluorine | Fluoridated water and toothpaste | Retention of calcium in bones and teeth |
| Iodine | Iodized salt and seafood | Energy production and thyroid function |
| Manganese | Whole grain and nuts | Not fully understood |
| Molybdenum | Organ meats, green leafy vegetables, legumes, whole grains, and dairy | Not fully understood; detoxification |
| Selenium | Broccoli, cabbage, garlic, whole grains, brewer’s yeast, celery, onions, and organ meats | Not fully understood |
Nutritional Guidelines
Nutritional guidelines are developed by governmental agencies to provide guidance to the population on how to best meet nutritional needs. These guidelines may vary by country. The National Academies of Sciences, Engineering, and Medicine set the Dietary Reference Intakes (DRIs) for the United States and Canada. Dietary Reference Intakes (DRIs) are a set of reference values used to plan and assess nutrient intakes of healthy people, including proteins, carbohydrates, fats, vitamins, minerals, and fiber. Nutrients included in the DRIs are obtained through a typical diet, although some foods may be fortified with certain nutrients that are commonly deficient in diets.[43]
Choose MyPlate Food Guide
The U.S. Department of Agriculture (USDA) issues dietary guidelines for appropriate serving sizes of each food group and number of servings recommended each day. The “Choose MyPlate” food guide is an easy-to-understand visual representation of how a healthy plate of food should be divided based on food groups. See Figure 14.4[44] for a Choose MyPlate image. A little more than half of the plate should be grains and vegetables, with a focus on whole grains and a variety of vegetables. About one quarter of the plate should be fruits, with an emphasis on whole fruits. About one quarter of the plate should be protein, with an emphasis on consuming a variety of low-fat protein sources. All of these groups combined should make up no more than 85% of daily caloric intake based on a 2,000-calorie diet. Fats, oils, and added sugars are not included, but should make up no more than 15% of daily caloric intake. Foods should be selected that are as nutrient-dense as possible. Nutrient-dense foods mean there is a high proportion of nutritional value relative to calories contained in the food, such as fruits and vegetables. Conversely, calorie-dense foods should be minimized because they have a large amount of calories with few nutrients. For example, candy and soda are calorie-dense with few nutrients and should be minimized.[45],[46] See Figure 14.5 for an image of MyPlate [47]
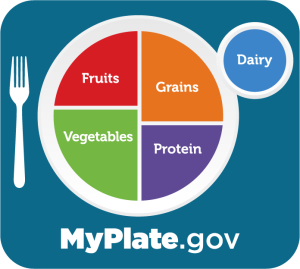
Figure 14.4 MyPlate Food Guide
Read more about USDA MyPlate guidelines at https://www.myplate.gov/.
MyPlate information and images are also available in several other languages so that education can be tailored to the client’s preferred language. For example, Figure 14.5[48] shows MyPlate in Vietnamese. This image would be accompanied with written information about food groups that include the client’s typical dietary choices.
Vegetable Group
For a well-rounded diet, a variety of vegetables should be consumed, including vegetables from all five vegetable groups: dark green leafy vegetables; red and orange vegetables; beans, peas, and lentils (formerly called the legumes group); starchy vegetables; and other vegetables. Vegetables can be fresh, frozen, canned, or dried. Dark green leafy vegetables include kale, Swiss chard, spinach, broccoli, and salad greens. Red and orange vegetables include carrots, bell peppers, sweet potatoes, tomatoes, tomato juice, and squash. The beans, peas, and lentils group includes dried beans, black beans, chickpeas, kidney beans, split peas, and black-eyed peas. (Note that this group does not include green beans or green peas.) This vegetable group also supplies some protein and can be included in the protein group as well. Starchy vegetables include root vegetables, such as potatoes, as well as corn. The “other vegetables” category includes any vegetable that doesn’t fit in the other four categories, such as asparagus, avocados, brussels sprouts, cabbage, cucumbers, snow peas, and mushrooms, and a variety of others.
Daily serving suggestions of vegetables for individuals with a 2,000 calorie diet are 2 ½ cup equivalents of vegetables per day. For example, a “one cup equivalent” equals 1 cup raw or cooked vegetables, one cup 100% vegetable juice, ½ cup of dried vegetables, or 2 cups of leafy green vegetables. Approximately 90% of Americans do not meet the recommended daily intake of vegetables.[49] See Figure 14.6[50] for an image of vegetables.

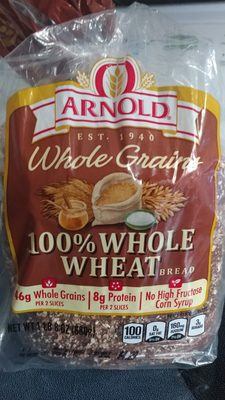
Grain Group
Grains are classified as whole grains or refined grains. Whole grains include the entire grain kernel and supply more fiber than refined grains. Examples of whole grains include amaranth, whole barley, popcorn, oats, whole grain cornmeal, brown or wild rice, and whole grain cereal or crackers. Refined grains have been processed to remove parts of the grain kernel and supply little fiber. As a result, they quickly increase blood glucose levels. Examples of refined grains include white bread, white rice, Cream of Wheat, pearled barley, white pasta, and refined-grain cereals or crackers. Some grains are fortified to ensure adequate intake of folic acid. See Figure 14.7[51] for an image of whole grain whole wheat bread.
The daily serving suggestions of grains for an individual with a 2,000-calorie diet are six-ounce equivalents per day, split equally between whole and refined grains. For example, a “one ounce equivalent” of grains equals ½ cup of cooked rice, pasta, or cereal or 1 cup of flaked cereal. Most Americans consume adequate amounts of total grains, although roughly 98% are deficient in recommended whole grain amounts, and 74% consume more than the recommended refined grain amounts.[52]
Fruit Group
Fruits can be frozen, canned, or dried, in addition to 100% fruit juice. A few examples of fruits include apples, oranges, bananas, melons, peaches, apricots, pineapples, and rhubarb. Daily serving suggestions of fruits for an individual with a 2,000-calorie diet are 2 cup equivalents per day. For example, “one cup equivalent” equals 1 cup of raw or cooked fruit, 8 ounces of 100% fruit juice, or ½ cup of dried fruit. Approximately 80% of Americans do not consume the recommended daily intake of fruits.[53] See Figure 14.8[54] for an image of fruits.

Dairy Group
Dairy products can be liquid, dried, semi-solid, or solid depending on the type of product. Dairy products include milk, lactose-free milk, fortified soy milk, buttermilk, cheese, yogurt, and kefir. Sour cream and cream cheese are not considered dairy items in terms of nutritional benefits. Daily serving suggestions of dairy products for an individual with a 2,000-calorie diet are 3 cup equivalents per day. For example, “one cup equivalent” equals 1 cup of milk, soy milk, or yogurt; 1 ½ ounces of natural cheese, or 2 ounces of processed cheese. Approximately 90% of Americans consume less than the recommended daily intake of dairy products.[55] See Figure 14.9[56] for an image of dairy products.

Protein Group
Proteins are categorized by the type of protein source. The meats, poultry, and eggs category consists of any type of animal or poultry meat, organ meat, or poultry egg. Lean meats should be selected to minimize fat and calorie intake from high-fat meats.
The seafood category includes any type of fish, clams, crab, lobster, oyster, and scallops. It is important to choose fish with low mercury levels to prevent negative effects of a buildup of mercury in the body. In general, large, fatty ocean fish, such as tuna, have higher levels of mercury due to their diet and storage of mercury in their fatty tissues.
The nuts, seeds, and soy products category includes tree nuts, peanuts, nut butters, seeds, or seed butters. Soy products include tofu and any other products made from soy. Unsalted nuts should be selected to avoid excess salt intake.
Protein is also contained in other food groups, such as dairy or the vegetable category of peas, beans, and lentils. Daily serving suggestions of proteins for individuals with a 2,000-calorie diet are 5 ½ ounce equivalents per day. Servings should total up to 26-ounce equivalents per week of meats, eggs, and poultry; 8-ounce equivalents per week of seafood; and 5-ounce equivalents per week of nuts, seeds, or soy products. A “one ounce equivalent” of protein equals 1 ounce of lean meat, one egg, ¼ cup cooked beans, or 1 tablespoon of peanut butter. Most Americans consume adequate amounts of protein, but many consume proteins high in saturated fat and sodium that contribute to diseases such as coronary artery disease.[57]
Oil/Fat Group
Examples of oils are vegetable oil, canola oil, olive oil, butter, lard, and coconut oil. Daily serving suggestions of fats or oils for individuals with a 2,000-calorie diet are 27 grams per day. While it is important to limit oils and fats due to their calorie-dense nature, some fat and oil intake is essential for nutrient absorption and overall health. It is best to select healthy unsaturated fats, such as avocados, nuts, or olive oil.[58]
Gender
A person’s gender affects their calorie and nutrient requirements. Males typically have higher calorie and protein needs related to increased muscle mass. Females typically require fewer calories to maintain their body weight due to a higher proportion of adipose (fat tissue) than muscle. Menstruating females also have higher iron requirements to offset losses that occur during menstruation.
Read Nutrition and Food Safety Information and Resources for Healthcare Professionals from the U.S. Food and Drug Administration.
Factors Affecting Nutritional Status
Now that we have discussed basic nutritional concepts and dietary guidelines, let’s discuss factors that can affect a person’s nutritional status. Many things that can cause altered nutrition, such as physiological factors, cultural and religious beliefs, economic resources, drug and nutrient disorders, surgery, altered metabolic states, alcohol and drug abuse, and psychological states.
Physiological Factors
Nutritional intake is affected by several physiological factors. Appetite is controlled by the hypothalamus, a tiny gland deep within the brain that triggers feelings of hunger or fullness depending on hormone and neural signals being sent and received. See Figure 14.10[59] for an image of the hypothalamus indicated by the red arrow. Hunger causes a feeling of emptiness in the abdomen and is often accompanied by audible noises coming from the abdomen as the stomach contracts due to emptiness. Hunger can cause feelings of discomfort, nausea, and tiredness. Satiety is a feeling of fullness that often comes after eating, although it can also be caused by impairments of the hypothalamus. Electrolyte imbalances and fluid volume imbalances can also trigger hunger and thirst by sending signals to the hypothalamus.[60]

The five senses play an important role in food intake. For example, food with a pleasing aroma may induce mouth watering and hunger, whereas food or environments with displeasing aromas often suppress the appetite. Texture and taste of foods also play a role in stimulation of appetite.
Poor dentition or poor oral care has a negative effect on appetite, so adequate oral care is crucial for clients prior to eating.[61] Additionally, the condition of a client’s teeth and gums, the fit of dentures, and gastrointestinal function also play an important role in nutrition. Loose teeth, swollen gums, or poor-fitting dentures can make eating difficult.
Difficulty swallowing, called dysphagia, can make it dangerous for the client to swallow food because it can result in pneumonia from aspiration of food into the lungs. Special soft diets or enteral or parenteral nutrition are typically prescribed for clients with dysphagia. Nurses collaborate with speech therapists when assessing and managing dysphagia.
A poorly functioning gastrointestinal tract makes nutrient absorption difficult and can result in malnourishment. Diseases that cause inflammation of the gastrointestinal tract impair absorption of nutrients. Examples of these conditions include esophagitis, gastritis, inflammatory bowel disease, and cholecystitis. Clients with these disorders should select nutrient-dense foods and may require prescribed supplements to increase nutrient intake.
Cultural and Religious Beliefs
Cultural and religious beliefs often influence food selection and food intake. It is important for nurses to conduct a thorough client assessment, including food preferences, to ensure adequate nutritional intake during hospitalization. The nurse should not assume a particular diet based on a client’s culture or religion, but instead should determine their individual preferences through the assessment interview.
Cultural beliefs affect types of food eaten and when they are eaten. Some foods may be restricted due to beliefs or religious rituals, whereas other foods may be viewed as part of the healing process. For example, some cultures do not eat pork because it is considered unclean, and others eat “kosher” food that prescribes how food is prepared. Some religions fast during religious holidays from sunrise to sunset, where others avoid eating meat during the time of Lent.[62],[63]
Read more about the impact of religious and cultural beliefs on food intake in the “Spirituality” chapter of this book.
Economic Resources
If a client has inadequate financial resources, food security and food choices are often greatly impacted. Healthy, nutrient-dense, fresh foods typically cost more than prepackaged, heavily processed foods. Poor economic status is correlated with the consumption of calorie-dense, nutrient-poor food choices, putting these individuals at risk for inadequate nutrition and obesity.[64] Social programs such as Meals on Wheels, free or reduced-cost school breakfast and lunch programs, and government subsidies based on income help reduce food insecurity and promote the consumption of healthy, nutrient-dense foods. Nurses refer at-risk clients to social workers and case managers for assistance in applying for these social programs.
Drug and Nutrient Interactions
Some prescription drugs affect nutrient absorption. For example, some medications such as proton pump inhibitors (omeprazole) alter the pH of stomach acid, resulting in poor absorption of nutrients. Other medications, such as opioids, often decrease a person’s appetite or cause nausea, resulting in decreased calorie and nutrient intake.
Surgery
Surgery can affect a client’s nutritional status due to several factors. Food and drink are typically withheld for a period of time prior to surgery to prevent aspiration of fluid into the lungs during anesthesia. Anesthesia and pain medication used during surgery slow peristalsis, and it often takes time to return to normal. Slow peristalsis can cause nausea, vomiting, and constipation. Until the client is able to pass gas and bowel sounds return, the client is typically ordered to have nothing by mouth (NPO). If a client experiences prolonged NPO status, such as after significant abdominal surgery, intravenous fluids and nutrition may be required.
Surgery also stimulates the physiological stress response and increases metabolic demands, causing the need for increased calories. The stress response can also cause elevated blood glucose levels due to the release of corticosteroids, even if the client has not been previously diagnosed with diabetes mellitus. For this reason, nurses often monitor post-op clients’ bedside blood glucose levels carefully.
Bowel resection surgery in particular has a negative impact on nutrient absorption. Because all or parts of the intestine are removed, there is decreased absorption of nutrients, which can result in nutrient deficiencies. Many clients who have experienced bowel resection require nutrient supplementation.
Bariatric surgery is used to treat obesity and reduce obesity-related cardiovascular risk factors. Bariatric procedures alter the anatomy and physiology of the gastrointestinal tract, which makes clients susceptible to nutritional deficiencies.[65] Read more about bariatric surgery and long-term nutritional issues in the following box.
Read more about bariatric surgery and long-term nutritional issues.[66]
Altered Metabolic States
Metabolic demands impact nutrient intake. In conditions where metabolic demands are increased, such as during growth spurts in childhood or adolescence, nutritional intake should be increased. Disease states, such as cancer, hyperthyroidism, and AIDS, can increase metabolism and require an increased amount of nutrients. However, cancer treatment, such as radiation and chemotherapy, often causes nausea, vomiting, and decreased appetite, making it difficult for clients to obtain adequate nutrients at a time when they are needed in high amounts due to increased metabolic demand.
Other diseases like diabetes mellitus cause complications with nutrient absorption due to insulin. Insulin is necessary for the metabolism of fats, proteins, and carbohydrates, but in clients with diabetes mellitus, insulin production is insufficient or their body is not able to effectively use circulating insulin. This lack of insulin can result in impaired nutrient metabolism.
Alcohol and Drug Misuse
Alcohol and drug misuse can affect nutritional status. Alcohol is calorie-dense and nutrient-poor. With alcohol use, the consumption of water, food, and other nutrients often decreases as clients “drink their calories.” This may result in decreased protein intake and body protein deficiency. Nutrient digestion and absorption can also decrease with alcohol consumption if the stomach lining becomes eroded or scarred. This can cause hemoglobin, hematocrit, albumin, folate, thiamine, vitamin B12, and vitamin C deficiencies, as well as decreased calcium, magnesium, and phosphorus levels.[67]
Misuse of stimulants, such as methamphetamine and cocaine, causes an increased metabolic rate and decreased appetite and contributes to weight loss and malnourishment.
Psychological State
Various psychological states have a direct effect on appetite and a client’s desire to eat. Acute and chronic stress stimulates the hypothalamus and increases production of glucocorticoids and glucose. This can increase the person’s appetite, causing increased calorie intake, fat storage, and subsequent weight gain. When a person feels stressed, their food choices are often nutrient-poor and calorie-dense, which further increases weight gain and nutrient deficiencies. In other individuals, the stress response causes loss of appetite, weight loss, and nutrient deficiencies.[68]
Depression can cause loss of appetite or overeating. Many people eat calorie-dense “comfort foods” as a coping mechanism. Additionally, many antidepressants can cause weight gain as a side effect.
Conditions having a sudden and severe onset.
Have a slow onset and may gradually worsen over time.

