Open Resources for Nursing (Open RN)
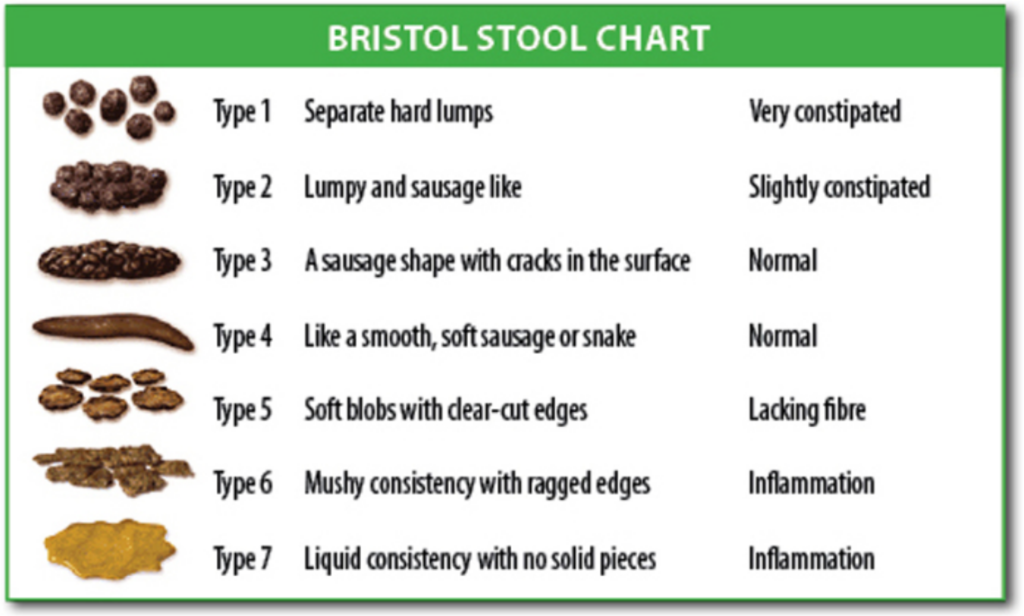
Constipation is defined by NANDA-I as, “A decrease in normal frequency of defecation accompanied by difficult or incomplete passage of stool and/or passage of excessively hard, dry stool.”[1] Typically a client is diagnosed with constipation if they have less than three bowel movements per week. Constipation can be caused by slowed peristalsis due to decreased activity, dehydration, lack of fiber, medications such as opioids, depression, or surgical procedures in the abdominal area. As the stool moves slowly through the large intestine, additional water is reabsorbed, resulting in the stool becoming hard, dry, and difficult to move through the lower intestines. See Figure 16.6[2] for the Bristol Stool Chart used to assess the characteristics of stools, ranging from constipation to diarrhea.
The client may experience associated symptoms such as rectal pressure, abdominal cramps, bloating, distension, and straining. Fecal impaction can occur when stool accumulates in the rectum, usually due to the client not feeling the presence of stool or not using the toilet when the urge is felt. Fecal impact has hallmark signs of seepage of liquid stool from the anus. It is important to not confuse this seepage with diarrhea. Large balls of hard stool are treated with mineral oil enemas or digital removal (i.e., with a lubricated, gloved finger that can be painful for the client.)
Interventions
The goal of interventions implemented to treat constipation is to establish what is considered a normal bowel pattern for each client and to set an expected outcome of a bowel movement at least every 72 hours regardless of intake. Treatment typically includes a prescribed daily bowel regimen, such as oral stool softeners (e.g., docusate) and a mild stimulant laxative (e.g., sennosides). Stronger laxatives (e.g., Milk of Magnesia or bisacodyl), rectal suppositories, or enemas are implemented when oral medications are not effective.
Clients should be educated about the importance of increased fluids, increased dietary fiber, and increased activity to prevent constipation. Some food sources, such as prune juice, prunes, and apricots, are helpful in preventing constipation. Over-the-counter medication, such as methylcellulose or psyllium, can be used to increase dietary fiber. When administering these medications, mix in a full eight-ounce glass of water to avoid the development of an intestinal obstruction.
Read more about laxatives used to treat constipation in the “Gastrointestinal” chapter in Open RN Nursing Pharmacology, 2e.
Intestinal Obstruction or Paralytic Ileus
Intestinal obstruction is a partial or complete blockage of the intestines so that contents of the intestine cannot pass through it. It can be caused by paralytic ileus, a condition where peristalsis is not propelling the contents through the intestines, or by a mechanical cause, such as fecal impaction. Clients who have undergone abdominal surgery or received general anesthesia are at increased risk for paralytic ileus. Other risk factors include the chronic use of opioids, electrolyte imbalances, bacterial or viral infections of the intestines, decreased blood flow to the intestines, or kidney or liver disease. If an obstruction blocks the blood supply to the intestine, it can cause infection and tissue death (gangrene).[3]
Symptoms of an intestinal obstruction or paralytic ileus include abdominal distention or a feeling of fullness, abdominal pain or cramping, inability to pass gas, vomiting, constipation, or diarrhea. Bowel sounds must be assessed for abnormal findings. It can be difficult to accurately interpret changes in bowel sounds, so any change in bowel sounds accompanied with other symptoms should be reported to the health care provider. Early intestinal obstruction can present with high-pitched “tinkling” sounds. Hypoactive bowel sounds can indicate constipation and may occur after abdominal surgery, anesthesia, or with use of opioid medications. Absent bowel sounds can indicate an ileus or mechanical bowel obstruction.[4] Because of the common occurrence of paralytic ileus in postoperative clients, nurses routinely monitor for these symptoms, and diet orders are not upgraded until the client is able to pass gas.
Treatment includes maintaining strict NPO status and typically includes insertion of an NG tube attached to suction to help relieve abdominal distention and vomiting until peristalsis returns. Obstructions may require surgery if the tube does not relieve the symptoms or if there are signs of tissue death.[5]
- Herdman, T., & Kamitsuru, S. (2017). NANDA international nursing diagnoses: Definitions & classification 2018-2020 (11th ed.). Thieme Publishers ↵
- “Bristol_stool_chart.svg” by Cabot Health, Bristol Stool Chart is licensed under CC BY-SA 3.0 ↵
- A.D.A.M. Medical Encyclopedia [Internet]. Atlanta (GA): A.D.A.M., Inc.; c1997-2021. Intestinal obstruction and ileus; [updated 2021, Feb 8; cited 2021, Feb 16]. https://medlineplus.gov/ency/article/000260.htm ↵
- Medline Plus. (2022). Abdominal sounds. https://medlineplus.gov/ency/article/003137.htm ↵
- A.D.A.M. Medical Encyclopedia [Internet]. Atlanta (GA): A.D.A.M., Inc.; c1997-2021. Intestinal obstruction and ileus; [updated 2021, Feb 8; cited 2021, Feb 16]. https://medlineplus.gov/ency/article/000260.htm ↵
Learning Activities
(Answers to “Learning Activities” can be found in the “Answer Key” at the end of the book. Answers to interactive activity elements will be provided within the element as immediate feedback.)
Scenario 1
Mr. Jones is a 67-year-old client on the medical-surgical floor who recently underwent a colon resection. See Figure 14.14 for an image of Mr. Jones.[1] He is post-op Day 2 and has been NPO since surgery. He has been receiving IV fluids but has been asking about when he can resume eating.
Questions:
- What assessments should be performed to determine if the client's diet can be progressed?
- What are the first steps during dietary transition from NPO status?
Scenario 2
Mrs. Casey is a 78-year-old widow who recently had a stroke and continues to experience mild right-sided weakness. See Figure 14.15 for an image of Mrs. Casey.[2] She is currently receiving physical therapy in a long-term care facility and ambulates with the assistance of a walker. Mrs. Casey confides, "I am looking forward to going home, but I will miss the three meals a day here."
Her height is 5'2" and she weighs 84 pounds. Her recent lab work results include the following results: Hgb: 8.8 g/dL, WBC 3500, Magnesium 1.4 mg/dL, Albumin 1.0 g/dL

Questions:
- What is Mrs. Casey's BMI and what does this number indicate?
- Analyze Mrs. Casey's recent lab work and interpret the findings.
- Describe focused assessments the nurse should perform regarding Mrs. Casey's nutritional status.
- Create a PES nursing diagnosis statement for Mrs. Casey based on her nutritional status.
- Create a SMART outcome statement for Mrs. Casey.
- Outline planned nutritional interventions for Mrs. Casey while she is at the facility, as well as when she returns home.
- How will you evaluate if your nursing care plan is successful for Mrs. Casey?

Test your knowledge using this NCLEX Next Generation-style bowtie question. You may reset and resubmit your answers to this question an unlimited number of times.[3]
A broad term used in nursing that includes “reasoning about clinical issues such as teamwork, collaboration, and streamlining workflow.”
Learning Objectives
- Describe risk factors for fluid and electrolyte disturbances
- Identify cues related to fluid/electrolyte balance
- Identify diagnostic tests and lab values indicative of a disturbance in fluid and electrolyte disturbances
- Identify essential nutrients
- Identify supplements to enhance nutrition alterations
- Contribute to a plan of care for clients with an alteration in nutrition and fluid and electrolyte disturbances
The human body maintains a delicate balance of fluids and electrolytes to help ensure proper functioning and homeostasis. When fluids or electrolytes become imbalanced, individuals are at risk for organ system dysfunction. If an imbalance goes undetected and is left untreated, organ systems cannot function properly and ultimately death will occur. Nurses must be able to recognize subtle changes in fluid or electrolyte balances in their clients so they can intervene promptly. Timely assessment and intervention prevent complications and save lives.

