Open Resources for Nursing (Open RN)
Three major concepts associated with grieving are loss, grief, and mourning. Loss is the absence of a possession or future possession with the response of grief and the expression of mourning. The feeling of loss can be associated with the loss of health, changes in relationships and roles, and eventually the loss of life. After a client dies, the family members and other survivors experience loss.[1]
Grief is the emotional response to a loss, defined as the individualized and personalized feelings and responses that an individual makes to real, perceived, or anticipated loss. These feelings may include anger, frustration, loneliness, sadness, guilt, regret, and peace. Grief affects survivors physically, psychologically, socially, and spiritually. The grief process is not orderly and predictable. Emotional fluctuation is normal and expected. There are times when the person experiencing the loss feels in control and accepting, and there are other times when the loss feels unbearable and they feel out of control.[2] See Figure 17.1[3] for an image of an individual in a cemetery who may be experiencing grief.

Mourning is the outward, social expression of loss. Individuals outwardly express loss based on their cultural norms, customs, and practices, including rituals and traditions. Some cultures may be very emotional and verbal in their expression of loss, such as wailing or crying loudly. Other cultures are stoic and show very little reaction to loss. Culture also dictates how long one mourns and how the mourners “should” act. The expression of loss is also affected by an individual’s personality and previous life experiences.[4]
Types of Grief
There are five different categories of grief: anticipatory grief, acute grief, normal grief, disenfranchised grief, and complicated grief.
Anticipatory Grief
Anticipatory grief is defined as grief before a loss, associated with diagnosis of an acute, chronic, and/or terminal illness experienced by the client, family, or caregivers. Examples of anticipatory grief include actual or fear of potential loss of health, independence, body part, financial stability, choice, or mental function.[5]
Sometimes anticipatory grief starts at the time of a terminal diagnosis and can proceed until the person dies. Clients and their family members can feel anticipatory loss. The client often anticipates the loss of independence, function, or comfort, which can cause significant pain and anxiety if not given the proper support. A client may also have concrete fears such as the loss of the ability to drive, live independently, or maintain their current body image. They may also have grief regarding the loss of anticipated family experiences, such as celebrating the marriage of a child, the birth of a grandchild, an anniversary, or another significant life event. The family often starts grieving for the loss of their loved one before they die as they envision their life without their loved one in it. This type of grief has been shown to help cushion a person’s bereavement reaction.[6]
Acute Grief
Acute grief begins immediately after the death of a loved one and includes the separation response and response to stress. During this period of acute grief, the bereaved person may be confused and/or uncertain about their identity or social role. They may disengage from their usual activities and experience disbelief and shock that their loved one is gone.[7] See Figure 17.2[8] for an image of a sculpture depicting acute grief.

Normal Grief
Normal grief includes the common feelings, behaviors, and reactions to loss. Normal grief reactions to a loss can include the following:
- Physical symptoms such as hollowness in the stomach, tightness in the chest, weakness, heart palpitations, sensitivity to noise, breathlessness, tension, lack of energy, and dry mouth
- Emotional symptoms such as numbness, sadness, fear, anger, shame, loneliness, relief, emancipation, yearning, anxiety, guilt, self-reproach, helplessness, and abandonment
- Cognitive symptoms such as a state of depersonalization, confusion, inability to concentrate, dreams of the deceased, idealization of the deceased, or a sense of presence of the deceased
- Behavioral signs such as impaired work performance, crying, withdrawal, overreactivity, changed relationships, or avoidance of reminders of the deceased[9]
Acute grieving may take months and but can also take years, depending on the loss. No one ever truly gets over the loss, but there is an eventual reconnection with the world of the living as the relationship with the deceased changes.[10]
Disenfranchised Grief
Disenfranchised grief is grief over any loss that is not validated or recognized. Those affected by this type of grief do not feel the freedom to openly acknowledge their grief. Individuals at risk for disenfranchised grief are those who have lost loved ones to stigmatized illnesses or events, such as AIDS. Mothers and/or fathers may grieve over terminated pregnancies or stillborn babies. The loss of a previously severed relationship or divorce can contribute to this type of grief because the individual may not be able to mourn openly due to the circumstances surrounding the relationship.
Complicated Grief
Complicated grief occurs when there is interference in the grieving process leading to a prolonged, more intense grieving. There is often preoccupation with the circumstances of the loss, which may manifest as feelings of guilt regarding the situation around the loss. There is generally a negative focus on the loss, which overrides any positive emotions the person may feel. Complicated grieving can cause significant distress, impaired functioning, and suicidal thinking.[11] Complicated grief is seen in 10-20% of individuals experiencing the death of a romantic partner and with higher estimates for parents who have lost a child. According to the ELNEC, there are four types of complicated grief, including chronic grief, delayed grief, exaggerated grief, and masked grief. Risk factors for developing complicated grief include sudden or traumatic death, suicide, homicide, a dependent relationship with the deceased, chronic illness, death of a child, multiple losses, unresolved grief from prior losses, concurrent stressors, witnessing a difficult dying process such as pain and suffering, lack of support systems, and lack of a faith system. Complicated grief may require professional assistance depending on its severity. Factors that contribute to complicated grief in older adults include lack of a support network, concurrent losses, poor coping skills, and loneliness.[12]
- Chronic Grief: Normal grief reactions that do not subside and continue over very long periods of time.
- Delayed Grief: Normal grief reactions that are suppressed or postponed by the survivor consciously or unconsciously to avoid the pain of the loss.
- Exaggerated Grief: An intense reaction to grief that may include nightmares, delinquent behaviors, phobias, and thoughts of suicide.
- Masked Grief: Grief that occurs when the survivor is not aware of behaviors that interfere with normal functioning as a result of the loss. For example, an individual cancels lunch with friends so they can go to the cemetery daily to visit their loved one’s grave.[13]
Stages of Grief
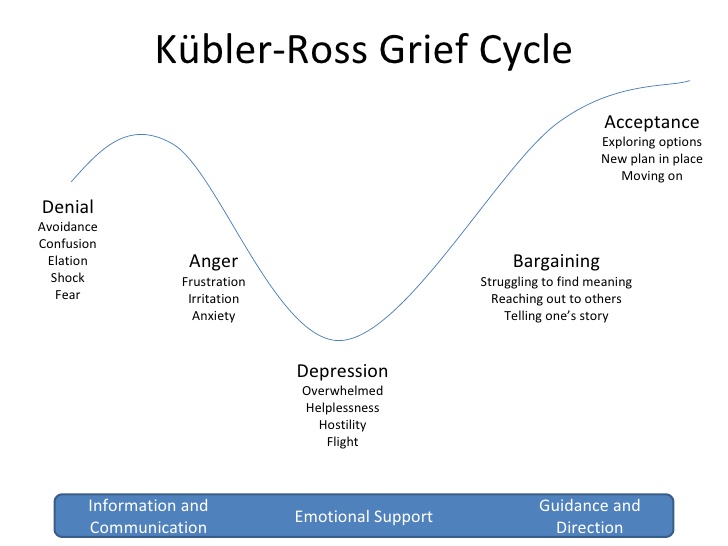
There are several stages of grief that may occur following a loss. It can be helpful for nurses to have an understanding of these stages to recognize the emotional reactions as symptoms of grief so they can support clients and families as they cope with loss. Famed Swiss psychiatrist Elizabeth Kubler-Ross identified five main stages of grief in her book On Death and Dying.[14] Clients and families may experience these stages along a continuum, move randomly and repeatedly from stage to stage, or skip stages altogether. There is no one correct way to grieve, and an individual’s specific needs and feelings must remain central to care planning.
Kuber-Ross identified that clients and families demonstrate various characteristic responses to grief and loss. These stages include denial, anger, bargaining, depression, and acceptance, commonly referred to by the mnemonic “DABDA.” See Figure 17.3[15] for an illustration of the Kubler-Ross Grief Cycle. Keep in mind that these stages of grief not only occur due to loss of life, but also occur due to significant life changes such as divorce, loss of friendships, loss of a job, or diagnosis with a chronic or terminal illness.[16]
View the beginning of this YouTube video clip[17] from the movie Steel Magnolias that shows a mother demonstrating stages of the grieving process.
Denial
Denial occurs when the individual refuses to acknowledge the loss or pretends it isn’t happening. This stage is characterized by an individual stating, “This can’t be happening.” The feeling of denial is self-protective as an individual attempts to numb overwhelming emotions as they process the information. The denial process can help to offset the immediate shock of a loss. Denial is commonly experienced during traumatic or sudden loss or if unexpected life-changing information or events occur. For example, a client who presents to the physician for a severe headache and receives a diagnosis of terminal brain cancer may experience feelings of denial. See Figure 17.4[18] for an image of a person depicting reaction to unexpected news with denial.

Anger
Anger in the grief process often masks pain and sadness. The subject of anger can be quite variable; anger can be directed to the individual who was lost, internalized to self, or projected toward others. Additionally, an individual may lash out at those uninvolved with the situation or have bursts of anger that seemingly have no apparent cause. Health care professionals should be aware that anger may often be directed at them as they provide information or provide care. It is important that health care team members, family members, and others who become the target of anger recognize that the anger and emotion are not a personal attack, but rather a manifestation of the challenging emotions that are a part of the grief process. If possible, the nurse can provide supportive presence and allow the client or family member time to vent their anger and frustration while still maintaining boundaries for respectful discussion. Rather than focusing on what to say or not to say, allowing a safe place for a client or family member to verbalize their frustration, sorrow, and anger can offer great support. See Figure 17.5[19] for an image of a child depicting anger.

Bargaining
Bargaining can occur during the grief process in an attempt to regain control of the loss. When individuals enter this phase, they are looking to find ways to change or negotiate the outcome by making a deal. Some may try to make a deal with God or their higher power to take away their pain or to change their reality by making promises to do better or give more of themselves if only the circumstances were different. For example, a client might say, “I promised God I would stop smoking if He would heal my wife’s lung cancer.”
Depression
Feelings of depression can occur with intense sadness over the loss of a loved one or the situation. Depression can cause loss of interest in activities, people, or relationships that previously brought one satisfaction. Additionally, individuals experiencing depression may experience irritability, sleeplessness, and loss of focus. It is not uncommon for individuals in the depression phase to experience significant fatigue and loss of energy. Simple tasks such as getting out of bed, taking a shower, or preparing a meal can feel so overwhelming that individuals simply withdraw from activity. In the depression phase, it can be difficult for individuals to find meaning, and they may struggle with identifying their own sense of personal worth or contribution. Depression can be associated with ineffective coping behaviors, and nurses should watch for signs of self-medicating through the use of alcohol or drugs to mask or numb depressive feelings. See Figure 17.6[20] for an image of a person depicting feelings of depression.

Acceptance
Acceptance refers to an individual understanding the loss and knowing it will be hard but acknowledging the new reality. The acceptance phase does not mean absence of sadness but is the acknowledgement of one’s capabilities in coping with the grief experience. In the acceptance phase, individuals begin to reengage with others, find comfort in new routines, and even experience happiness with life activities again. See Figure 17.7[21] of an image of a person depicting acceptance.

Grief Tasks
Kubler-Ross’s grief stages describe many feelings that individuals commonly experience while grieving loss. Other experts also describe the grieving process in terms of tasks that one must accomplish. These tasks include notification and shock, experiencing the loss, and reintegration.[22]
- Notification and shock: This phase occurs when a person first learns of the loss and experiences feelings of numbness or shock. The person may isolate themselves from others while processing this information. The first task for the person to complete is to acknowledge the reality of the loss by assessing and recognizing the loss.
- Experiencing the loss: The second task involves experiencing the loss emotionally and cognitively. The person must work through the pain by reacting to, expressing, and experiencing the pain of separation and grief.
- Reintegration: The third task involves reorganization and restructuring of family systems and relationships by adjusting to the environment without the deceased. The person must form a new reality without the deceased and adapt to a new role while also retaining memories of the deceased.[23]
As a nurse, you can greatly assist clients and family members as they move through the grieving process by being willing and committed to spending time with them. Listen to their stories, be present, and bear witness to their pain. Remember that you cannot fix everything, but taking time to assess their symptoms of grief helps you identify other resources for support.
Palliative Care and Hospice
Palliative care and hospice care are specialty care areas related to the care of clients and their families experiencing loss and the grieving process.
Palliative care is a broad philosophy of care defined by the World Health Organization as improving the quality of life of clients, as well as their family members, who are facing problems associated with life-threatening illness. It prevents and relieves suffering through early identification, correct assessment, and treatment of pain and other problems, whether physical, psychosocial, or spiritual.[24] In the United States, palliative care is further described as, “Patient and family-centered care that optimizes quality of life by anticipating, preventing, and treating suffering. Palliative care occurs throughout the continuum of care and involves the interdisciplinary team collaboratively addressing physical, intellectual, emotional, social, and spiritual needs and facilitating patient autonomy, access to information, and choice.”[25] Palliative care focuses on comfort and quality of life but also includes continuing curative treatment such as dialysis, chemotherapy, and surgery.
Hospice care is a type of palliative care that addresses care for clients who are terminally ill when a health care provider has determined they are expected to live six months or less. Like palliative care, hospice provides comprehensive comfort care and support for the family, but in hospice, curative treatments are stopped. It is based on the idea that dying is part of the normal life cycle and supports the client and family through the dying and grief process. It also supports the surviving family members through the bereavement process. Hospice care does not hasten death but focuses on providing comfort while allowing a natural death. Symptoms control, including pain relief, and quality of life are of utmost importance.
Many clients decide to receive hospice care at home with the support of family, nurses, and hospice staff, but hospice services are also available across a variety of settings such as long-term care, assisted living facilities, hospitals, and prisons. In the United States, older adults enrolled in Medicare can choose to receive hospice care and stop receiving curative treatment. It is important to remember that stopping curative treatment does not mean discontinuing all medical treatment. For example, a client with cancer who is no longer responding to chemotherapy can decide to enter hospice care and focus on comfort and quality of life. The chemotherapy treatment will stop, but other medical care, such as blood pressure medications or antibiotics to treat infection, will continue as long as they are helpful in promoting quality of life. Medicare will also pay for all related home durable medical equipment (such as a hospital bed and home oxygen therapy equipment) and all medications related to the terminal diagnosis (including pain medications).[26],[27] See Figure 17.8[28] for an image of a client receiving hospice care.

Unfortunately, instead of viewing hospice as a care option to promote quality of life and reduce suffering, many clients and their families associate hospice care with “giving up,” or as a “death sentence,” and are resistant to this type of care. For this reason, many health care teams advocate the implementation of palliative care until clients and their family members are ready to discuss hospice care.
When a client and their family members make the decision to implement home hospice, their desire is for the client to comfortably spend their final days in their home environment. However, if the client’s condition later becomes challenging for family members to manage at home, it can be very difficult to consider transferring the client to a hospice inpatient unit at that time. It is often helpful to encourage clients and family members to tour alternative care agencies when considering hospice and be prepared if this decision is later warranted.
Comfort Care
Comfort care is a term commonly used in the acute care setting that is similar to palliative care and hospice. Comfort care occurs when the clients and medical team’s goals shift from curative intervention to symptom control, pain relief, and quality of life. However, there is no formal admission to hospice or palliative care that can impact insurance coverage. Rather than focusing on aggressive medical intervention, the focus changes to symptom control to provide the client with the greatest degree of comfort possible as they approach their end of life. When comfort care is ordered by the provider, many interventions are eliminated to promote comfort, such as administering medications (with the exception of analgesics or antianxiety medications), monitoring vital sign monitoring, or performing blood draws or other invasive procedures.
Read more about the National Coalition for Hospice and Palliative Care’s Palliative Care Guidelines.
Ethical and Legal Considerations
End-of-life care often includes unique complexities for the client, family, and nurse. There may be times when what the physician or nurse believes to be the best treatment conflicts with what the client desires. There may also be challenges related to decision-making that cause disagreements within a family or cause conflict with the treatment plan. Additional challenging factors include availability of resources and insurance company policies and programs.
Despite these complexities, it is important for the nurse to honor and respect the wishes of the client. Despite any conflicts in decision-making among health care providers, family members, and the client, the nurse must always advocate for the client’s wishes. Nurses should also be aware of the practice guidelines for ethical dilemmas stated in the American Nurses Association’s Standards of Professional Nursing Practice and Code of Ethics.[29],[30] These resources assist the nurse in implementing expected behaviors according to their professional role as a nurse.
If complex ethical dilemmas occur, many organizations have dedicated ethics committees that offer support, guidance, and resources for complex ethical decisions. These committees can serve as support systems, share resources, provide legal insight, and make recommendations for action. The nurse should feel supported in raising concerns within their health care organization if they believe an ethical dilemma is occurring.
Review ANA’s Code of Ethics.
Do-Not-Resuscitate Orders and Advance Directives
Additional legal considerations when providing care at the end of life are do-not-resuscitate orders (DNR) orders and advance directives. A do-not-resuscitate (DNR) order is a medical order that instructs health care professionals not to perform cardiopulmonary resuscitation (CPR) if a client’s breathing stops or their heart stops beating. The order is only written with the permission of the client (or the client’s health care power of attorney, if activated.) Ideally, a DNR order is set up before a critical condition occurs. CPR is emergency treatment provided when a client’s blood flow or breathing stops that may involve chest compressions and mouth-to-mouth breathing, electric shocks to stop lethal cardiac rhythms, breathing tubes to open the airway, or cardiac medications. The DNR order only refers to not performing CPR and is recorded in a client’s medical record. It is crucial to understand that with a DNR order, clients are still entitled to medical treatment, such as antibiotics, IVs, and medications, and as such, treatment should be rendered when abnormalities are noted or anticipated. Wallet cards, bracelets, or other DNR documents are also available to have at home or in nonhospital settings. The decision to implement a DNR order is typically very difficult for a client and their family members to make.[31] Many people have unrealistic ideas regarding the success rates of CPR and the quality of life a client experiences after being revived, especially for clients with multiple chronic diseases or those receiving palliative care. For example, a recent study found the overall rate of survival leading to hospital discharge for someone who experiences cardiac arrest is about 10.6 percent.[32] Nurses can provide up-to-date health teaching regarding CPR and its effectiveness based on the client’s current condition and facilitate discussion about a DNR order.
Advance directives are legal documents that direct care when the client can no longer speak for themselves and include a health care power of attorney and a living will. The health care power of attorney legally identifies a trusted individual to serve as a decision maker for health issues when the client is no longer able to speak for themselves. It is the responsibility of this designated individual to carry out care actions in accordance with the client’s wishes. A health care power of attorney can be a trusted family member, friend, or colleague who is of sound mind and is over the age of 18. They should be someone who the client is comfortable expressing their wishes to and someone who will enact those desired wishes on the client’s behalf.
The health care power of attorney should also have knowledge of the client’s wishes outlined in their living will. A living will is a legal document that describes the client’s wishes if they are no longer able to speak for themselves due to injury, illness, or a persistent vegetative state. The living will addresses issues like ventilator support, feeding tube placement, cardiopulmonary resuscitation, and intubation. It is a vital means of ensuring that the health care provider has a record of one’s wishes. However, the living will cannot feasibly cover every possible potential circumstance, so the health care power of attorney is vital when making decisions outside the scope of the living will document.
Read more about advance care planning at the National Institute on Aging and at Honoring Choices Wisconsin.
![]() Nurses must understand the health care practice legalities for the state in which they practice nursing. There can be practice issues in various states that raise additional ethical complexities for the practicing nurse. For example, Oregon, Washington, Vermont, and New Mexico all have laws that allow clients to participate in assisted dying practices involving assisted suicide or active euthanasia. In assisted suicide, the client is provided the means to carry out suicide such as a lethal dose of medication. Active euthanasia involves someone other than the client carrying out action to end a person’s life. Most nursing organizations prevent a nurse from participating in assisted dying practices. Nurses must be aware of the Nurse Practice Act in their state and the legalities and ethical challenges of nursing actions surrounding complex issues such as assisted suicide, active euthanasia, and abortion.
Nurses must understand the health care practice legalities for the state in which they practice nursing. There can be practice issues in various states that raise additional ethical complexities for the practicing nurse. For example, Oregon, Washington, Vermont, and New Mexico all have laws that allow clients to participate in assisted dying practices involving assisted suicide or active euthanasia. In assisted suicide, the client is provided the means to carry out suicide such as a lethal dose of medication. Active euthanasia involves someone other than the client carrying out action to end a person’s life. Most nursing organizations prevent a nurse from participating in assisted dying practices. Nurses must be aware of the Nurse Practice Act in their state and the legalities and ethical challenges of nursing actions surrounding complex issues such as assisted suicide, active euthanasia, and abortion.
Caring for the Family of a Dying Client
When caring for a client who is nearing the end of life, the family members require nursing care as well. Fading away is a transition that families make when they realize their seriously ill family member is dying. Although they may have been previously told by a health care provider that their loved one would die from the illness, there is often a sudden realization their family member “is not going to get any better” when their health begins to significantly decline. With this realization comes the transition of fading away.[33]
There are various dimensions that both clients and family members experience during this fading away process:
- Redefining: There is a shift for both clients and families from “what used to be” to “what is now.”
- Burdening: As clients become more dependent, they may feel as if they are a burden to their family–physically, financially, emotionally, socially, and spiritually. Yet, family members typically do not feel the care they are providing is a burden, but rather, “something you do for someone you love.”
- Searching for Meaning: Clients journey inward, seek spiritual reflection, and become more connected to important family members and friends. Family members may search for meaning inwardly through spiritual reflection or explore for meaning with family members and friends.
- Living Day to Day: Clients who eventually find meaning in their illness live each day with a more positive attitude. Family members who try to “make the best of it” make efforts to enjoy the limited time left with their loved one.
- Preparing for Death: Clients often want to leave a legacy. Spouses often want to meet every need of their ill spouse. Clients and family members may begin to make prearrangements for the funeral, as well as get their will and other financial matters in order.
- Contending with Change: Clients and their family members change roles, social patterns, and work patterns. They know the life they used to have will soon be gone.[34]
Nurses can assist clients and family members during the fading away transition by being present and actively listening.
Caregiver Support
Most clients with chronic illness have family caregivers that are an extension of the health care team and work around the clock, all days of the week. They typically provide 70-80% of the care at home. It is important for nurses to assess the caregiver when seeing them with the client in the home, clinic, hospital, or long-term setting and provide encouragement. It is helpful to acknowledge their work is very difficult and to praise them for their efforts.[35] See Figure 17.9[36] for an image of a mother acting as caregiver and supporting her son’s health.

Research shows caregivers often have the following needs[37]:
- Support, assistance, and practical help (e.g., finding others to assist with grocery shopping, going to the pharmacy, and food preparation)
- Honest conversations with the health care team
- Assurance their loved one is being honored
- Inclusion in decision-making
- Desire to be listened to and their concerns heard
- Remembrance as a good and compassionate caregiver
- Assurance that they did all they possibly could for their loved one
Assess the caregiver’s needs for further assistance, as well as their social support network. Assess their physical needs, sleep patterns, and ability to perform other responsibilities. Watch for signs of declining health, clinical depression, or signs of increased use of alcohol and drugs. Listen to the caregiver’s stories and provide presence, active listening, and touch. Assist them in identifying and using support systems and refer them to resources and support groups in the community as needed.[38]
Cultural Considerations Regarding Death
When assessing clients, family members, and caregivers, it is important to respect their values, beliefs, and traditions related to health, illness, family caregiver roles, and decision-making. Information gathered through this comprehensive assessment is used to develop a nursing care plan that incorporates culturally sensitive resources and strategies to meet the needs of clients and their family members.[39] See Figure 17.10[40] for an image depicting a community grieving.

Nurses can acquire knowledge about how different cultural beliefs influence a client and their family members’ decision-making, approach to illness, pain, spirituality, grief, dying, death, and bereavement. See Table 17.2 for a brief comparison of various spiritual beliefs about death.[41],[42]
To learn more about holistic nursing care that addresses the spiritual needs of clients and their significant others, refer to the “Spirituality” chapter.
Table 17.2 Comparison of Spiritual Beliefs about Death[43]
| Religion | Beliefs Pertaining to Death | Preparation of the Body | Funeral |
|---|---|---|---|
| Christian
(Catholic and Protestant) |
Belief in Jesus Christ, the Bible, and an afterlife are central, although differences in interpretation exist in the various denominations. Catholics receive a sacrament called “anointing of the sick” when approaching the end of life. | Organ donation and autopsy are permitted. | Individuals are buried in cemeteries. Some denominations accept cremation as an alternative. Funerals or celebration of life services are typically held in a funeral home or church. |
| Jewish | Tradition cherishes life but death itself is not viewed as a tragedy. Views on an afterlife vary with the denomination (Reform, Conservative, or Orthodox). | Autopsy and embalming are forbidden under ordinary circumstances. Open caskets are not permitted. | Funeral is held as soon as possible after death. Dark clothing is worn at the funeral and after burial. It is forbidden to bury the deceased on the Sabbath or during festivals. Three mourning periods may be held after the burial, with Shiva being the first that occurs seven days after burial. |
| Buddhist | Both a religion and way of life with the goal of enlightenment. Life is believed to be a cycle of death and rebirth. | Goal is a peaceful death. Statue of Buddha may be placed at the bedside as the person is dying. Organ donation is not permitted. Incense is lit in the room following death. | Family washes and prepares the body after death. Cremation is preferred, but if buried, deceased are typically dressed in regular daily clothes instead of fancy clothing. Monks may be present at the funeral and lead the chanting. |
| Native American | Beliefs vary among tribes. Sickness is thought to mean that one is out of balance with nature. It is thought that ancestors can guide the deceased. Death is perceived as a journey to another world. Family may or may not be present for death. | Preparation of the body may be done by family. Organ donation is generally not preferred. | Various practices differ with tribes. Among the Navajo, hearing an owl or coyote is a sign of impending death, and the casket is left slightly open so the spirit can escape. Navajo and Apache tribes believe that spirits of the deceased can haunt the living. The Comanche tribe buries the dead in the place of death when possible or in a cave. |
| Hindu | Beliefs include reincarnation where a deceased person returns in the form of another, as well as Karma. | Organ donation and autopsy are acceptable. Death and dying must be peaceful. It is customary for the body to not be left alone until cremated. | Prefer cremation within 24 hours after death. Ashes are often scattered in sacred rivers. |
| Muslim | Believe in an afterlife and that the body must be quickly buried so that the soul may be freed. | Embalming and cremation are not permitted. Autopsy is permitted for legal or medical reasons only. After death, the body should face Mecca or the East. The body should be prepared by a person of the same gender. | Burial takes place as soon as possible. Women and men sit separately at the funeral. Flowers and excessive mourning are discouraged. The body is usually buried in a shroud and is buried with the head pointing toward Mecca. |
Read more about funeral traditions around the globe: Death is not the end: Fascinating funeral traditions from around the globe.
A Good Death
Death is a physical, psychological, social, and spiritual event. Family members who witness the last weeks, days, hours, and minutes of their loved one’s life will remember the death for all their lives. Although death is often perceived negatively in the American culture, research has found several themes that define a “good death” when nurses and the interdisciplinary team are caring for dying clients and their families:[44]
- Client preferences are met, including preferences for the dying process (i.e., where and with whom) and preparation for death (i.e., advanced directives, funeral arrangements).
- The client is pain-free with emotional well-being.
- The family is prepared for death and supportive of client’s preferences.
- Dignity and respect are demonstrated for the client.
- The client has a sense of life completion (i.e., saying goodbye and feeling life was well-lived).
- Spirituality and religious comfort are provided.
- Quality of life was maintained (i.e., maintaining hope, pleasure, gratitude).
- There is a feeling of trust/support/comfort from the nurse and interdisciplinary team.[45]
Nurses are often present during these final days and moments with clients during this difficult and sacred time.[46] Read more about nursing care performed during this time in the “Nursing Care During the Final Hours of Life” section.
Bereavement
The bereavement period includes grief (the inner feelings) and mourning (the outward reactions) after a loved one has died. A bereavement period is the time it takes for the mourner to feel the pain of the loss, mourn, grieve, and adjust to the world without the presence of the deceased. Bereavement can take a physical toll on a survivor. It is associated with an increased risk of myocardial infarction and cardiomyopathy for survivors, and widows and widowers have an increased chance of dying after their spouses die.[47] See Figure 17.11[48] for an image depicting bereavement by family members.

A bereaved person should be encouraged to talk about the death and understand their feelings are normal. They should allow for sufficient time for expression of grief and should postpone significant decisions such as changing jobs or moving. It is also important to encourage them to focus on their spirituality to enhance coping during this difficult time.[49] See Figure 17.12[50] for an image a person depicting one type of spirituality.

Americans often deny the need to express grief or feel the pain that accompanies a loss. However, although painful, both are beneficial to healing. As part of the interdisciplinary health team, nurses are often at the front line of helping clients and family members cope with their feelings of loss and grief. The nursing role during the bereavement period includes the following[51]:
- Assisting with enhanced coping mechanisms
- Assessing and facilitating spirituality
- Facilitating the grieving process by supporting the client and survivors to feel the loss, express the loss, and move through the tasks of grief
- Communicating assessments and interventions with the interdisciplinary team
Children
Children who have experienced the loss of a parent, sibling, grandparent, or friend experience grief based on their developmental stage. It can be normal grief or complicated grief. Children may be limited in their ability to verbalize and describe their feelings and grief. See Figure 17.13[52] for an image of a child depicting grief.

Symptoms of grief in younger children include nervousness, uncontrollable rages, frequent illness, incontinence, rebellious behavior, hyperactivity, nightmares, depression, compulsive behavior, memories fading in and out, excessive anger, overdependence on the remaining parent, denial, and/or disguised anger. Children may not understand that death is permanent until they are in preschool or older. It is important to use the word “death” and not euphemisms like “gone to sleep” or “gone away,” which can be confusing or ambiguous to children. Additionally, using these euphemisms may cause children to fear sleep.[53]
Symptoms of grief in older children include difficulty concentrating, forgetfulness, decreased academic performance, insomnia or sleeping too much, compulsiveness, social withdrawal, antisocial behavior, resentment of authority, overdependence, regression, resistance to discipline, suicidal thoughts or actions, nightmares, symbolic dreams, frequent sickness, accident proneness, overeating or undereating, truancy, experimentation with alcohol or drugs, depression, secretiveness, sexual promiscuity, or running away from home.[54]
Play is the universal language of children, so nurses should use it therapeutically when possible. Encouraging children that their grief is “normal” gives them comfort. Refer children, parents, and families to grief specialists as indicated. Make sure families are aware of local support groups.[55]
Parents and Grandparents
For parents, the death of a child can be devastating with a great need for bereavement support. For grandparents, the grief can be twofold as they experience their own grief, in addition to witnessing the grief of their child (the parent). Studies have shown that grandparents’ grief is seldom acknowledged.[56] See Figure 17.14[57] for an image of a sculpture depicting mourning for a child.

For more information on support for parents experiencing infant loss, go to http://nationalshare.org/
Spouses
The death of a husband or wife is well recognized as an emotionally devastating event, being ranked on life event scales as the most stressful of all possible losses. The intensity and persistence of the pain associated with this type of bereavement is thought to be due to the emotional marital bonds linking husbands and wives to each other. Spouses are co-managers of home and family, companions, sexual partners, and fellow members of larger social units.
Therapeutic Communication Tips
When communicating with the bereaved, it is more important to listen and be present rather than say the “right words.” It is also helpful to simply encourage silence. However, certain phrases should be avoided because they can create barriers in therapeutic communication:
- Avoid statements like, “I know/can imagine/understand how you feel.” Even if you have been through a similar situation, you don’t know how the survivor feels. Instead say, “This must be very difficult for you. Would you like to talk about it?”
- Don’t minimize the individual’s grief reaction with a statement like, “You should be over this by now.” Instead, say, “This process takes time, so don’t feel as if you need to rush through it.”
- Avoid statements that minimize the significance of the loss, such as, “At least you had a good life with them,” or “They’re in a better place now.” Instead, focus on exploring their feelings related to the loss, such as, “Tell me what your relationship was like.”[58]
Completion of the Grieving Process
Grief work is never completely finished because there will always be times when a memory, object, song, or anniversary of the death will cause feelings of loss for the survivor. However, healing occurs and is characterized by the following:
- The pain of the loss is lessened.
- The survivor has adapted to life without the deceased.
- The survivor has physically, psychologically, and socially “let go.”[59]
Letting go is a difficult process. One can let go and still find love and true meaning in the relationship they had with their loved one. Letting go does not mean cutting oneself off from the memories, but adapting to the loss and the continued bonds with the deceased.[60] See Figure 17.15[61] for a depiction of letting go by lighting a candle in memory of the deceased.

Self-Care
It is important for nurses to recognize that providing end-of-life care can have a significant impact on them. A nurse’s grief might be exacerbated when client loss is unexpected or is the result of a traumatic experience. For example, an emergency room nurse who provides care for a child who died as a result of a motor vehicle accident may find it difficult to cope with the loss and resume their normal work duties.
Grief can also be compounded when loss occurs repeatedly in one’s work setting or after providing care for a client for a long period of time. In some health care settings, especially during the COVID-19 pandemic, nurses do not have time to resolve grief from a loss before another loss occurs. Compassion fatigue and burnout occur frequently with nurses and other health care professionals who experience cumulative losses that are not addressed therapeutically.
Compassion fatigue is a state of chronic and continuous self-sacrifice and/or prolonged exposure to difficult situations that affect a health care professional’s physical, emotional, and spiritual well-being. This can lead to a person being unable to care for or empathize with someone’s suffering. Burnout can be manifested physically and psychologically with a loss of motivation. It can be triggered by workplace demands, lack of resources to do work professionally and safely, interpersonal relationship stressors, or work policies that can lead to diminished caring and cynicism.[62] See Figure 17.16[63] for an image depicting a nurse at home experiencing burnout due to exposure to multiple competing demands of work, school, and family responsibilities.

Self-care is important to prevent compassion fatigue and burnout. It is important for nurses to recognize the need to take time off, seek out individual healthy coping mechanisms, or voice concerns within their workplace. Prayer, meditation, exercise, art, and music are examples of healthy coping mechanisms that nurses can use to progress through their individual grief experience. Additionally, many organizations sponsor employee assistance programs that provide counseling services. These programs can be of great value and benefit in allowing individuals to voice their individual challenges with client loss. In times of traumatic client loss, many organizations hold debriefing sessions to allow individuals who participated in the care to come together to verbalize their feelings. These sessions are often held with the support of chaplains to facilitate individual coping and verbalization of feelings. (Read more about the role of chaplains in the “Spirituality” chapter.)
Throughout your nursing career, there will be times to stop and pay attention to warning signs of compassion fatigue and burnout. Here are some questions to consider:
- Has my behavior changed?
- Do I communicate differently with others?
- What destructive habits tempt me?
- Do I project my inner pain onto others?[64]
By becoming self-aware, you can implement self-care strategies to prevent compassion fatigue and burnout. Use the following “A’s” to assist in building resilience, connection, and compassion:
- Attention: Become aware of your physical, psychological, social, and spiritual health. What are you grateful for? What are your areas of improvement? This protects you from drifting through life on autopilot.
- Acknowledgement: Honestly look at all you have witnessed as a health care professional. What insight have you experienced? Acknowledging the pain of loss you have witnessed protects you from invalidating the experiences.
- Affection: Choose to look at yourself with kindness and warmth. Affection prevents you from becoming bitter and “being too hard” on yourself.
- Acceptance: Choose to be at peace and welcome all aspects of yourself. By accepting both your talents and imperfections, you can protect yourself from impatience, victim mentality, and blame.[65]
In addition to self-care strategies, it is helpful for nurses to obtain additional education in end-of-life care. See the following for more information about obtaining a palliative care certificate for your portfolio.
Read more about online end-of-life curriculum available on the American Association of Colleges of Nursing’s End-of-Life-Care Curriculum web page.
- This work is a derivative of Nursing Care at the End of Life by Lowey and is licensed under CC BY-NC-SA 4.0 ↵
- This work is a derivative of Nursing Care at the End of Life by Lowey and is licensed under CC BY-NC-SA 4.0 ↵
- “Grief_and_loss_(16755561105).jpg” by Thomas8047 is licensed under CC BY 2.0 ↵
- This work is a derivative of Nursing Care at the End of Life by Lowey and is licensed under CC BY-NC-SA 4.0 ↵
- This work is a derivative of Nursing Care at the End of Life by Lowey and is licensed under CC BY-NC-SA 4.0 ↵
- Kübler-Ross, E. (1969). On death and dying. The Macmillan Company. ↵
- This work is a derivative of Nursing Care at the End of Life by Lowey and is licensed under CC BY-NC-SA 4.0 ↵
- “WWStoryRome.jpg” by Carptrash is licensed under CC BY-SA 3.0 ↵
- This work is a derivative of Nursing Care at the End of Life by Lowey and is licensed under CC BY-NC-SA 4.0 ↵
- This work is a derivative of Nursing Care at the End of Life by Lowey and is licensed under CC BY-NC-SA 4.0 ↵
- Shear, M. K. (2012). Grief and mourning gone awry: Pathway and course of complicated grief. Dialogues in Clinical Neuroscience, 14(2), 119-28. https://doi.org/10.31887/DCNS.2012.14.2/mshear. ↵
- This work is a derivative of Nursing Care at the End of Life by Lowey and is licensed under CC BY-NC-SA 4.0 ↵
- This work is a derivative of Nursing Care at the End of Life by Lowey and is licensed under CC BY-NC-SA 4.0 ↵
- American Nurses Association. (2015). Nursing: Scope and standards of practice (3rd ed.). American Nurses Association. ↵
- “Kubler-ross-grief-cycle-1-728.jpg” by U3173699 is licensed under CC BY-SA 4.0 ↵
- This work is a derivative of StatPearls by Oates & Maani and is licensed under CC BY 4.0 ↵
- Movieclips. (2014, February 5). Steel Magnolias (8/8) movie CLIP - I wanna know why (1989) HD [Video]. YouTube. All rights reserved. https://youtu.be/iZx1W6cHw-g ↵
- “Young-indian-with-disgusting-expression-showing-denial-with-hands-42509-pixahive.jpg” by Sukhjinder is licensed under CC0 ↵
- “Child%27s_Angry_Face.jpg” by Babyaimeesmom is licensed under CC BY-SA 4.0 ↵
- “Depressed_(4649749639).jpg” by Sander van der Wel is licensed under CC BY-SA 2.0 ↵
- “Contentment_at_its_best.jpg” by Neha Bhamburdekar is licensed under CC BY-SA 4.0 ↵
- This work is a derivative of Nursing Care at the End of Life by Lowey and is licensed under CC BY-NC-SA 4.0 ↵
- This work is a derivative of Nursing Care at the End of Life by Lowey and is licensed under CC BY-NC-SA 4.0 ↵
- World Health Organization. (2020). Palliative care. https://www.who.int/news-room/fact-sheets/detail/palliative-care ↵
- National Hospice and Palliative Care Organization. (2021). Explanation of palliative care. https://www.nhpco.org/palliative-care-overview/explanation-of-palliative-care/ ↵
- This work is a derivative of Nursing Care at the End of Life by Lowey and is licensed under CC BY-NC-SA 4.0 ↵
- This work is a derivative of Introduction to Sociology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/introduction-sociology-2e/pages/1-introduction-to-sociology ↵
- “hospice-1761276_1280.jpg” by truthseeker08 is licensed under CC0 ↵
- American Nurses Association. (2015). Code of ethics for nurses with interpretive statements. American Nurses Association. https://www.nursingworld.org/practice-policy/nursing-excellence/ethics/code-of-ethics-for-nurses/coe-view-only/ ↵
- National Institute on Aging. (2017, May 17). What are palliative care and hospice care? U.S. Department of Health & Human Services. https://www.nia.nih.gov/health/what-are-palliative-care-and-hospice-care ↵
- A.D.A.M. Medical Encyclopedia [Internet]. Atlanta (GA): A.D.A.M., Inc.; c1997-2021. Do-not-resuscitate order; [updated 2021, June 9].https://medlineplus.gov/ency/patientinstructions/000473.htm ↵
- Ouellette, L., Puro, A., Weatherhead, J., Shaheen, M., Chassee, T., Whalen, D., & Jones, J.. (2018). Public knowledge and perceptions about cardiopulmonary resuscitation (CPR): Results of a multicenter survey. American Journal of Emergency Medicine, 36(10), 1900-1901. https://doi: 10.1016/j.ajem.2018.01.103. ↵
- This work is a derivative of Nursing Care at the End of Life by Lowey and is licensed under CC BY-NC-SA 4.0 ↵
- This work is a derivative of Nursing Care at the End of Life by Lowey and is licensed under CC BY-NC-SA 4.0 ↵
- This work is a derivative of Nursing Care at the End of Life by Lowey and is licensed under CC BY-NC-SA 4.0 ↵
- “140305-M-KL110-002_(13063045524).jpg” by U.S. Department of Defense Current Photos is licensed under CC0 ↵
- This work is a derivative of Nursing Care at the End of Life by Lowey and is licensed under CC BY-NC-SA 4.0 ↵
- This work is a derivative of Nursing Care at the End of Life by Lowey and is licensed under CC BY-NC-SA 4.0 ↵
- American Association of Colleges of Nursing. (2021). End-of-life-care (ELNEC). https://www.aacnnursing.org/ELNEC ↵
- “Mourning_in_Shanghai_(1).jpg” by Medalofdead is licensed under CC BY-SA 4.0 ↵
- This work is a derivative of Nursing Care at the End of Life by Lowey and is licensed under CC BY-NC-SA 4.0 ↵
- Pasero, C., & MacCaffery, M. (2010). Pain assessment and pharmacological management (1st ed.). Mosby. ↵
- Pasero, C., & MacCaffery, M. (2010). Pain assessment and pharmacological management (1st ed.). Mosby. ↵
- Karnes, B. (2009). Gone from my sight: The dying experience. Barbara Karnes Books. ↵
- Karnes, B. (2009). Gone from my sight: The dying experience. Barbara Karnes Books. ↵
- This work is a derivative of Nursing Care at the End of Life by Lowey and is licensed under CC BY-NC-SA 4.0 ↵
- This work is a derivative of Nursing Care at the End of Life by Lowey and is licensed under CC BY-NC-SA 4.0 ↵
- “Mourning,_Lette_Valeska.jpg” by Lette Valeska is licensed under CC BY-SA 3.0 ↵
- This work is a derivative of Nursing Care at the End of Life by Lowey and is licensed under CC BY-NC-SA 4.0 ↵
- “meditation-1350599_960_720.jpg” by brenkee is licensed under CC0. ↵
- This work is a derivative of Nursing Care at the End of Life by Lowey and is licensed under CC BY-NC-SA 4.0 ↵
- “sad-72217_960_720.jpg” by PublicDomainPictures is licensed under CC0 ↵
- This work is a derivative of Nursing Care at the End of Life by Lowey and is licensed under CC BY-NC-SA 4.0 ↵
- This work is a derivative of Nursing Care at the End of Life by Lowey and is licensed under CC BY-NC-SA 4.0 ↵
- This work is a derivative of Nursing Care at the End of Life by Lowey and is licensed under CC BY-NC-SA 4.0 ↵
- This work is a derivative of Nursing Care at the End of Life by Lowey and is licensed under CC BY-NC-SA 4.0 ↵
- “Sarcophagus,_marble,_mourning_for_child,_100-200_AD,_AM_Agrigento,_121062.jpg” by Zde is licensed under CC BY-SA 4.0 ↵
- This work is a derivative of Nursing Care at the End of Life by Lowey and is licensed under CC BY-NC-SA 4.0 ↵
- This work is a derivative of Nursing Care at the End of Life by Lowey and is licensed under CC BY-NC-SA 4.0 ↵
- This work is a derivative of Nursing Care at the End of Life by Lowey and is licensed under CC BY-NC-SA 4.0 ↵
- “Candle_burning.jpg” by NCCo at English Wikipedia is licensed under CC BY-SA 3.0 ↵
- This work is a derivative of Nursing Care at the End of Life by Lowey and is licensed under CC BY-NC-SA 4.0 ↵
- “Burnout_At_Work_-_Occupational_Burnout.jpg” by Microbiz Mag is licensed under CC BY 2.0 ↵
- This work is a derivative of Nursing Care at the End of Life by Lowey and is licensed under CC BY-NC-SA 4.0 ↵
- This work is a derivative of Nursing Care at the End of Life by Lowey and is licensed under CC BY-NC-SA 4.0 ↵
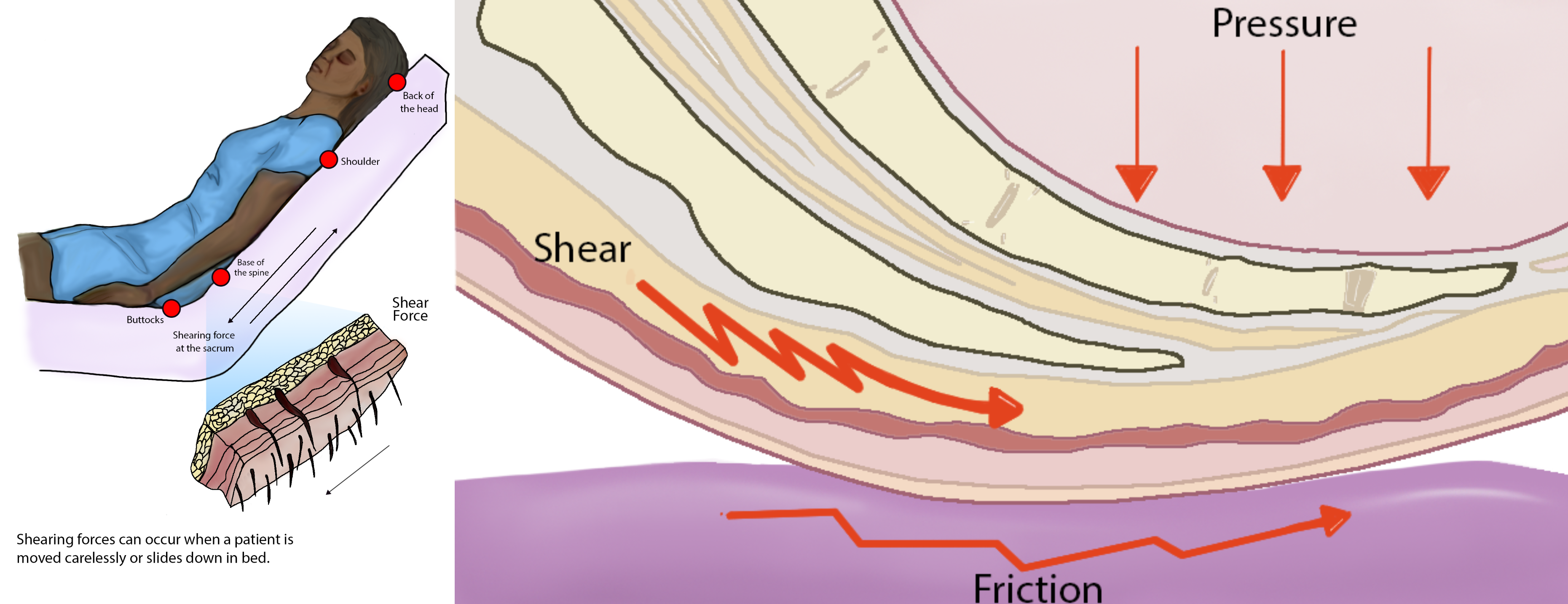
The remainder of this chapter will focus on applying the nursing process to a specific type of wound called a pressure injury. Pressure injuries are defined as, “Localized damage to the skin or underlying soft tissue, usually over a bony prominence, as a result of intense and prolonged pressure in combination with shear.” (Note that the 2016 NPUAP Pressure Injury Staging System now uses the term “pressure injury” instead of the historic term “pressure ulcer” because a pressure injury can occur without an ulcer present.) Pressure injuries commonly occur on the sacrum, heels, ischia, and coccyx and form when the skin layer of tissue gets caught between an external hard surface, such as a bed or chair, and the internal hard surface of a bone.
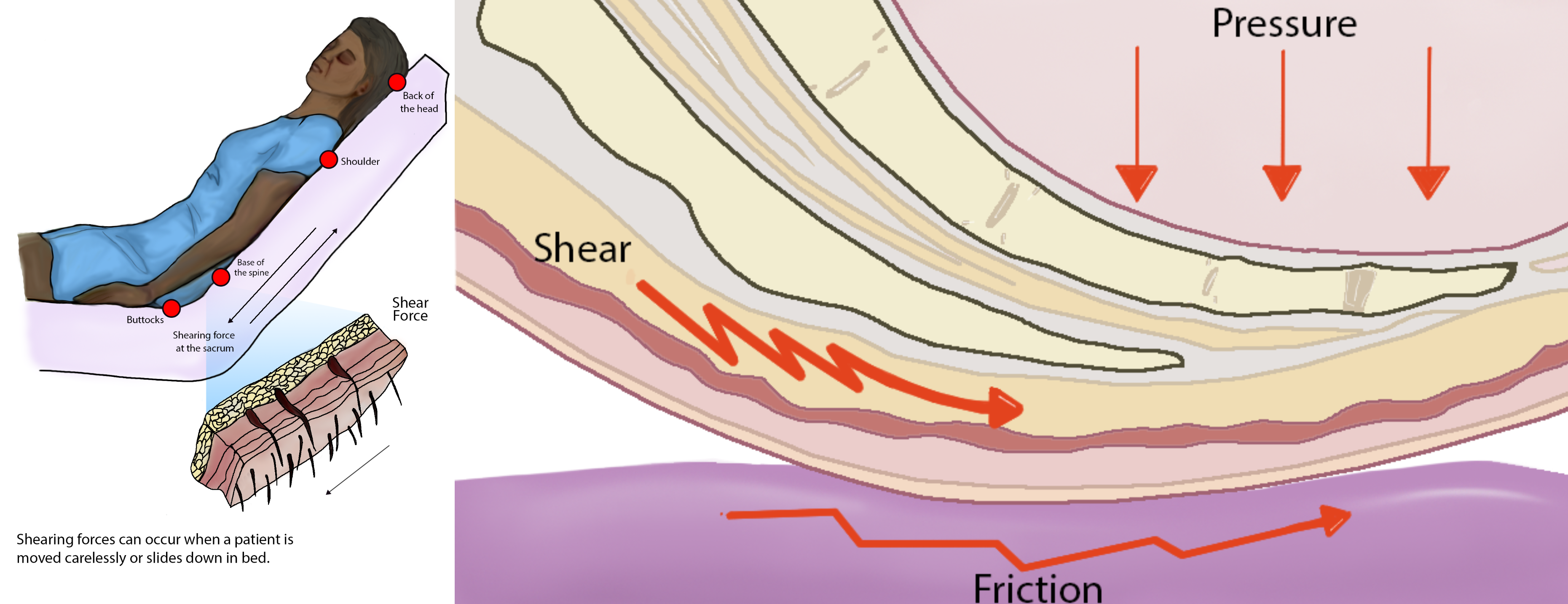
Shear occurs when tissue layers move over the top of each other, causing blood vessels to stretch and break as they pass through the subcutaneous tissue. For example, when a client slides down in bed, the outer layer of skin remains immobile because it remains attached to the sheets due to friction. However, the deeper layer of tissue (attached to bone) moves as the client slides down. This opposing movement of the outer layer of skin and the underlying tissues causes the capillaries to stretch and tear, which then causes decreased blood flow and oxygenation of the surrounding tissues resulting in a pressure injury.[1]
Friction refers to rubbing the skin against a hard object, such as the bed or the arm of a wheelchair. This rubbing causes heat, which can remove the top layer of skin and often results in skin damage. See Figure 10.13[2] for an illustration of shear and friction forces in the development of pressure injuries.
Hospital-acquired or worsening pressure injuries during hospitalization are considered "never events," meaning they are a serious, preventable medical errors that should never occur and require reporting to The Joint Commission. Additionally, the Centers for Medicare and Medicaid Services (CMS) and many private insurers will no longer pay for additional costs associated with "never events."[3],[4] Pressure injuries can be prevented with diligent assessment and nursing interventions such as frequent repositioning and providing good skin care.
Staging
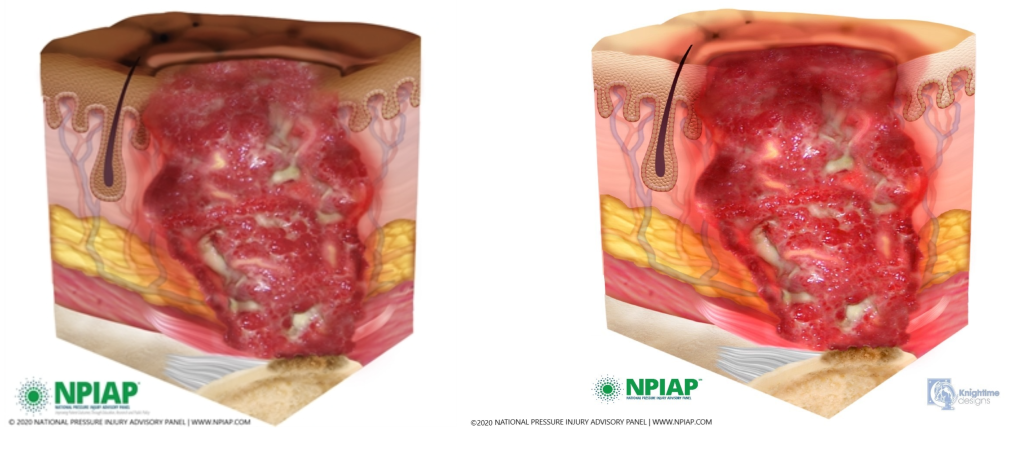
When assessed, pressure injuries are staged from 1 through 4 based on the extent of tissue damage. For example, Stage 1 pressure injuries have the least amount of tissue damage as evidenced by reddened, intact skin, whereas Stage 4 pressure injuries have the greatest amount of damage with deep, open ulcers affecting underlying tissue, muscle, ligaments, or tendons. See Figure 10.14[5] for images of four stages of pressure injuries.[6] Each stage is further described in the following subsections.

Stage 1 Pressure Injuries
Stage 1 pressure injuries are intact skin with a localized area of nonblanchable erythema where prolonged pressure has occurred. Nonblanchable erythema is a medical term used to describe an area of reddened skin that does not turn white when pressed. Nonblanchable erythema is an early sign of damage to underlying tissue caused by poor blood flow, ischemia, and damage to blood vessels in the area. Because damage is already present, there is a greater risk for Stage 1 pressure injuries to develop into worse pressure injuries if interventions to relieve pressure and not implemented. Skin with dark pigmentation may not demonstrate visible blanching, so it can be challenging to detect Stage 1 pressure injuries. For clients with dark pigmentation, nurses should assess for pain, firmness, softness, changes in temperature, or changes in color compared to surrounding areas.[7],[8]
See Figure 10.15[9] for an illustration of a Stage 1 pressure injury.
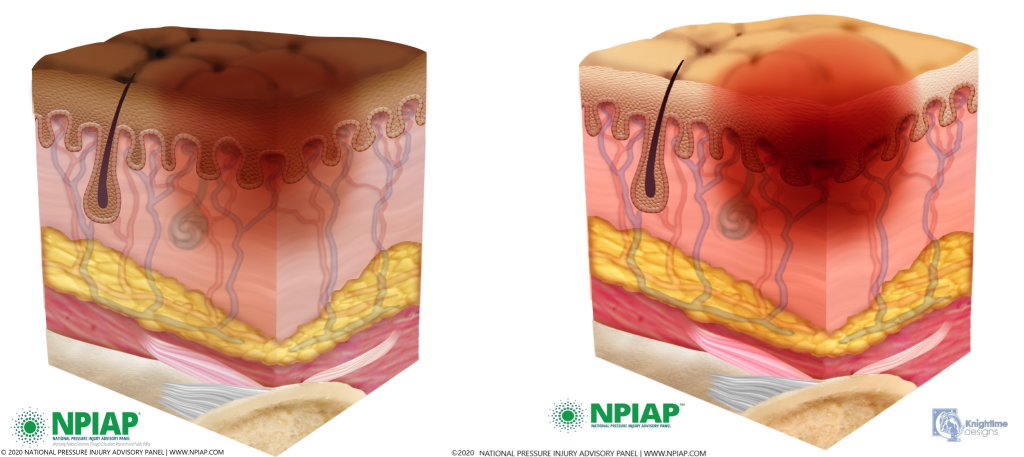
Stage 2 Pressure Injuries
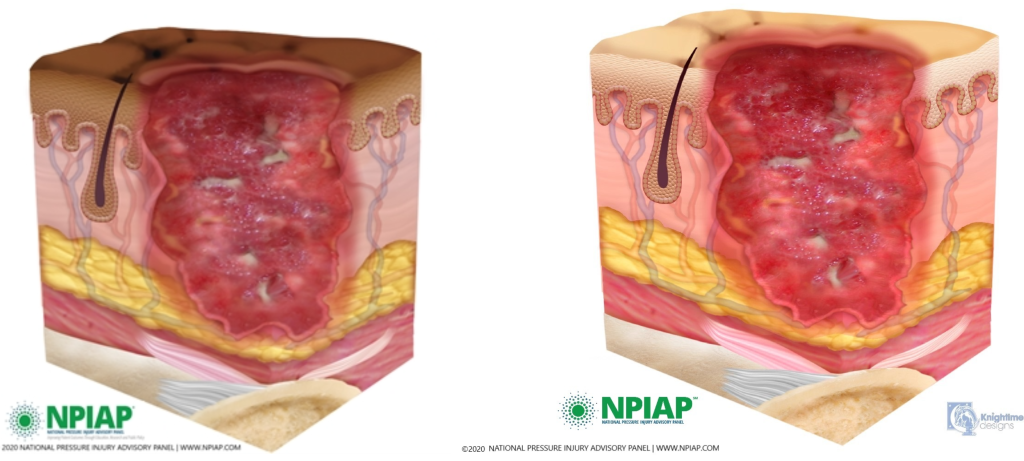
Stage 2 pressure injuries are partial-thickness loss of skin with exposed dermis. The wound has completely broken through the top layer of skin, and partly through the second layer, resulting in a shallow wound. The wound is shallow and generally open. The wound bed is viable and may appear like an intact or ruptured blister.[10] The wound area may be painful and the surrounding tissue may be swollen or discolored.[11] See Figure 10.16[12] for an illustration of a Stage 2 pressure injury.
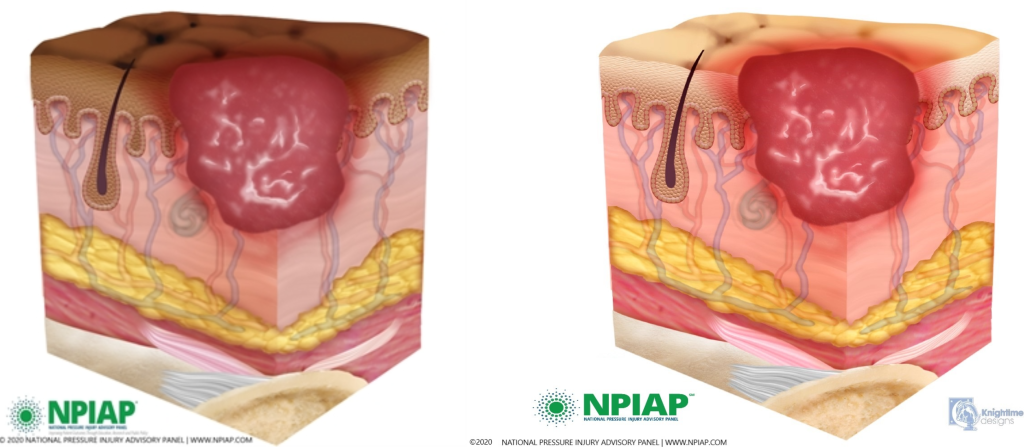
Stage 3 Pressure Injuries
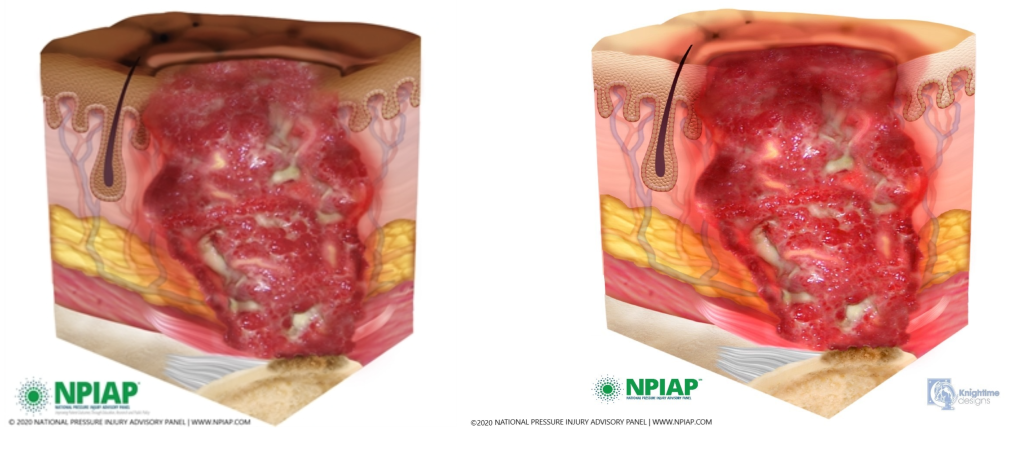
Stage 3 pressure injuries are full-thickness tissue loss in which fat is visible, but cartilage, tendon, ligament, muscle, and bone are not exposed. The depth of tissue damage varies by anatomical location. Because the wound extends through all skin layers, there is increased risk of infection in Stage 3 pressure injuries. There may be pus draining from the wound, tissue necrosis, pain, or fever, especially in the presence of an infection.[13] See Figure 10.17[14] for an illustration of a Stage 3 pressure injury.
Undermining and tunneling may occur in Stage 3 and 4 pressure injuries. Undermining occurs when the tissue under the wound edge becomes eroded, resulting in a pocket beneath the skin. Tunneling refers to passageways underneath the skin surface that extend from a wound and can take twists and turns.
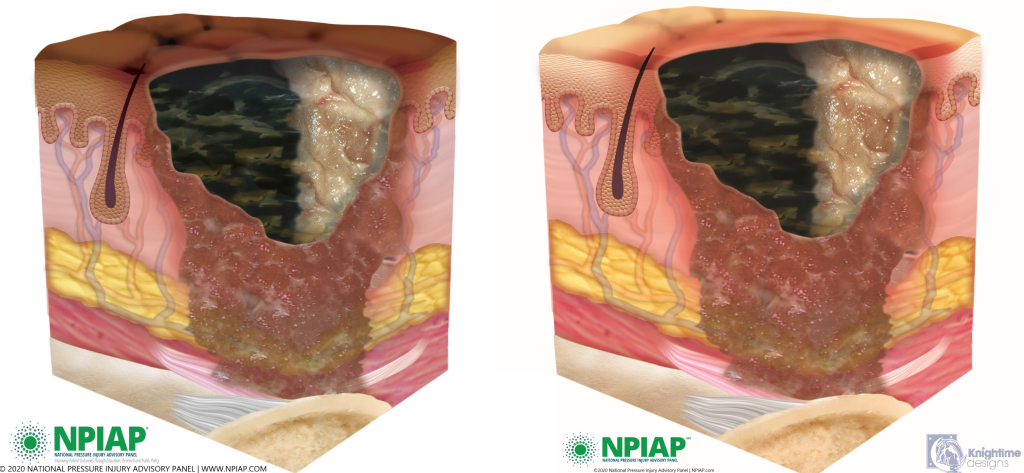
Slough and eschar may also be present in Stage 3 and 4 pressure injuries. Slough is inflammatory exudate that is usually light yellow, soft, and moist. Eschar is dark brown/black, dry, thick, and leathery dead tissue. If slough or eschar obscures the wound so that tissue loss cannot be assessed, the pressure injury is referred to as unstageable.[15] In most wounds, slough and eschar must be removed by debridement for accurate wound staging and for healing to occur. Removed of slough or eschar is surgically performed by specially trained health care providers. Nurses may apply prescribed chemical debridement agents or wet-to-dry dressings for mechanical debridement per provider orders.
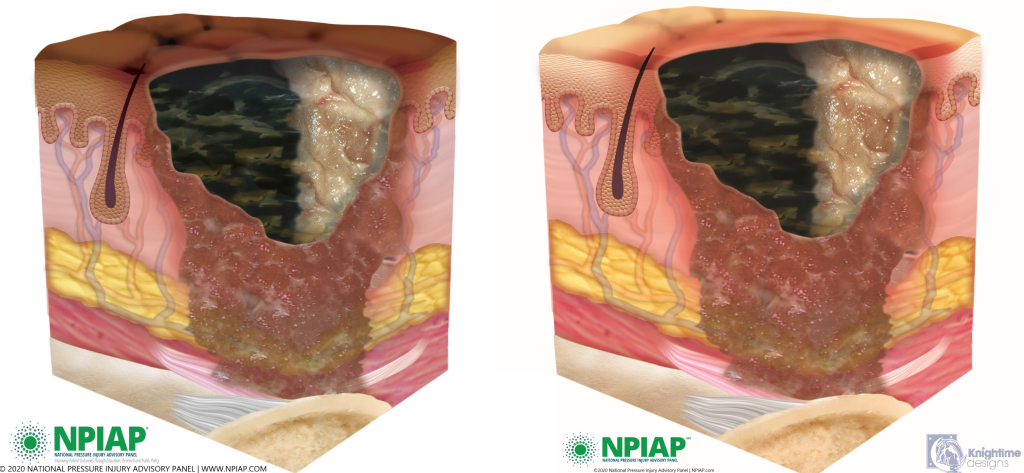
Stage 4 Pressure Injuries
Stage 4 pressure injuries are full-thickness tissue loss, like in Stage 3 pressure injuries, but also have exposed cartilage, tendon, ligament, muscle, or bone. Stage 4 pressure injuries are at an increased risk of infection because their depth goes through all skin layers. There may be pain associated with Stage 4 pressure ulcers, although they are often less painful because the wound damages nerve endings. There also at be firm or mushy texture at the site, discoloration, or necrosis to the wound. Because the wound often extends to the bone, thus exposing the bone to infectious agents in the environment, osteomyelitis (bone infection) may also be present. Osteomyelitis is a serious bone infection that may require amputation or cause death if not promptly treated aggressively with antibiotics.[16],[17]
See Figure 10.18[18] for an illustration of a Stage 4 pressure injury.
View images of different stages of pressure injuries on people with dark skin tones on the PPPIA Pressure Ulcers in People With Dark Skin Tones poster.
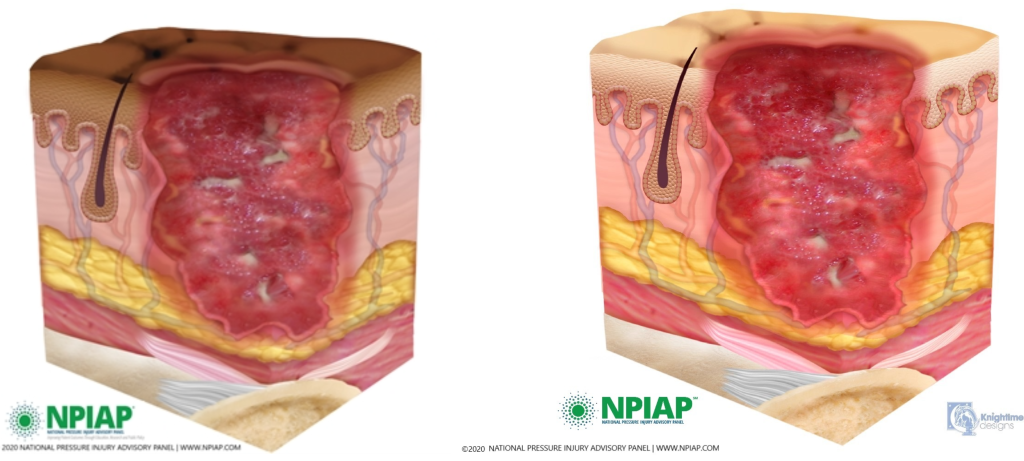
Unstageable Pressure Injuries
Unstageable pressure injuries are full-thickness skin and tissue loss in which the extent of tissue damage within the ulcer cannot be confirmed because it is obscured by slough or eschar. If slough or eschar were to be removed, a Stage 3 or Stage 4 pressure injury would likely be revealed. However, dry and adherent eschar on the heel or ischemic limb is not typically removed.[19] See Figure 10.19[20] for an illustration of an unstageable pressure ulcer due to the presence of eschar (on the left side of the wound) and slough (on the right side of the wound).
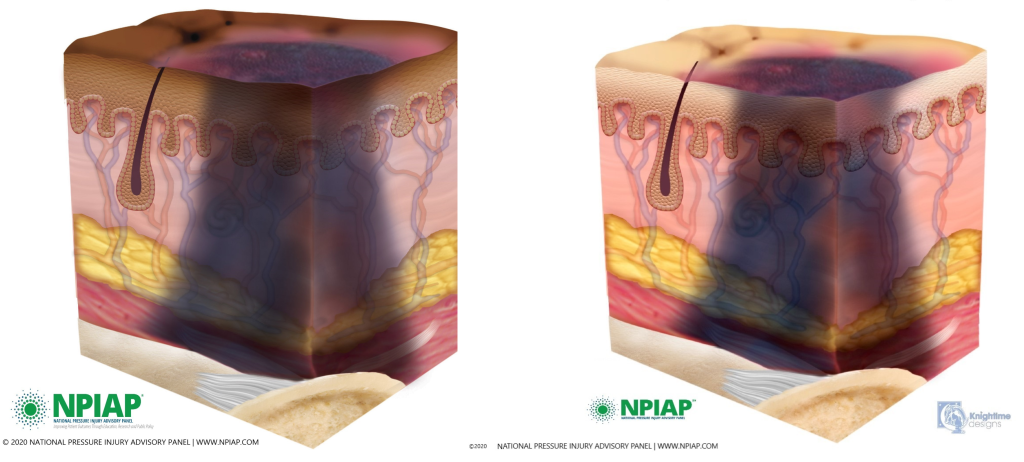
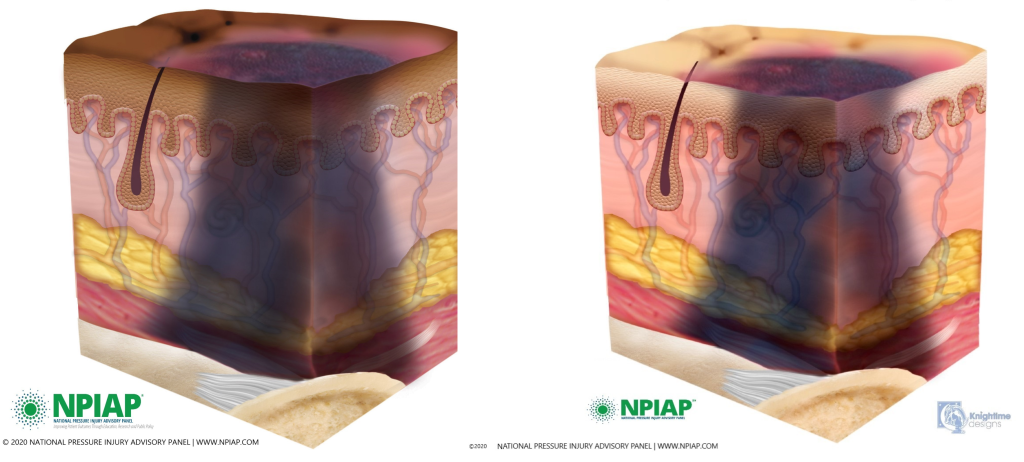
Deep Tissue Pressure Injuries
Deep tissue pressure injuries consist of persistent nonblanchable and deep red, maroon, or purple discoloration of an area. These discolorations typically reveal a dark wound bed or blood-filled blister. Be aware that the discoloration may appear differently in darkly pigmented skin. Deep tissue injury results from intense and/or prolonged pressure, as well as shear forces at the bone-muscle interface. The wound may evolve rapidly to reveal the actual extent of tissue injury, or it may resolve without tissue loss.[21],[22] See Figure 10.20 for an illustration of a deep tissue injury.
Video Review of Assessing Pressure Injuries[23]
The remainder of this chapter will focus on applying the nursing process to a specific type of wound called a pressure injury. Pressure injuries are defined as, “Localized damage to the skin or underlying soft tissue, usually over a bony prominence, as a result of intense and prolonged pressure in combination with shear.” (Note that the 2016 NPUAP Pressure Injury Staging System now uses the term “pressure injury” instead of the historic term “pressure ulcer” because a pressure injury can occur without an ulcer present.) Pressure injuries commonly occur on the sacrum, heels, ischia, and coccyx and form when the skin layer of tissue gets caught between an external hard surface, such as a bed or chair, and the internal hard surface of a bone.
Shear occurs when tissue layers move over the top of each other, causing blood vessels to stretch and break as they pass through the subcutaneous tissue. For example, when a client slides down in bed, the outer layer of skin remains immobile because it remains attached to the sheets due to friction. However, the deeper layer of tissue (attached to bone) moves as the client slides down. This opposing movement of the outer layer of skin and the underlying tissues causes the capillaries to stretch and tear, which then causes decreased blood flow and oxygenation of the surrounding tissues resulting in a pressure injury.[24]
Friction refers to rubbing the skin against a hard object, such as the bed or the arm of a wheelchair. This rubbing causes heat, which can remove the top layer of skin and often results in skin damage. See Figure 10.13[25] for an illustration of shear and friction forces in the development of pressure injuries.
Hospital-acquired or worsening pressure injuries during hospitalization are considered "never events," meaning they are a serious, preventable medical errors that should never occur and require reporting to The Joint Commission. Additionally, the Centers for Medicare and Medicaid Services (CMS) and many private insurers will no longer pay for additional costs associated with "never events."[26],[27] Pressure injuries can be prevented with diligent assessment and nursing interventions such as frequent repositioning and providing good skin care.
Staging
When assessed, pressure injuries are staged from 1 through 4 based on the extent of tissue damage. For example, Stage 1 pressure injuries have the least amount of tissue damage as evidenced by reddened, intact skin, whereas Stage 4 pressure injuries have the greatest amount of damage with deep, open ulcers affecting underlying tissue, muscle, ligaments, or tendons. See Figure 10.14[28] for images of four stages of pressure injuries.[29] Each stage is further described in the following subsections.

Stage 1 Pressure Injuries
Stage 1 pressure injuries are intact skin with a localized area of nonblanchable erythema where prolonged pressure has occurred. Nonblanchable erythema is a medical term used to describe an area of reddened skin that does not turn white when pressed. Nonblanchable erythema is an early sign of damage to underlying tissue caused by poor blood flow, ischemia, and damage to blood vessels in the area. Because damage is already present, there is a greater risk for Stage 1 pressure injuries to develop into worse pressure injuries if interventions to relieve pressure and not implemented. Skin with dark pigmentation may not demonstrate visible blanching, so it can be challenging to detect Stage 1 pressure injuries. For clients with dark pigmentation, nurses should assess for pain, firmness, softness, changes in temperature, or changes in color compared to surrounding areas.[30],[31]
See Figure 10.15[32] for an illustration of a Stage 1 pressure injury.
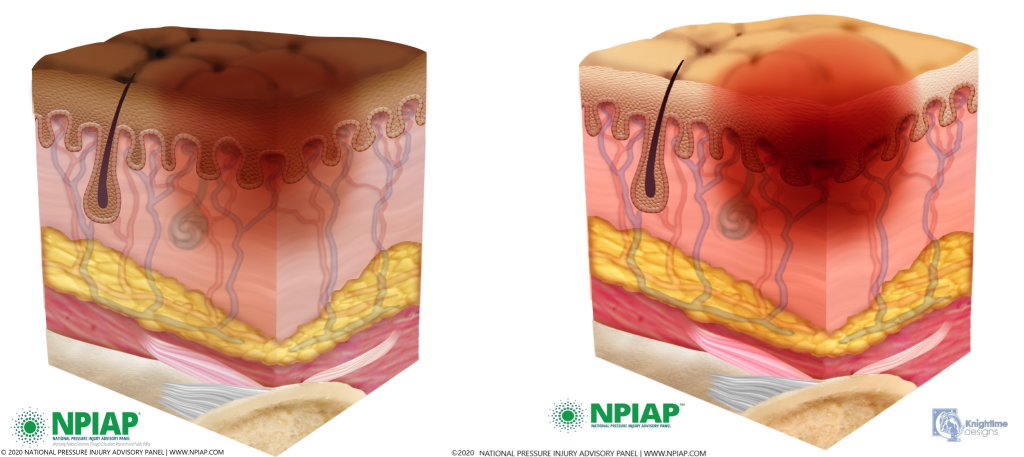
Stage 2 Pressure Injuries
Stage 2 pressure injuries are partial-thickness loss of skin with exposed dermis. The wound has completely broken through the top layer of skin, and partly through the second layer, resulting in a shallow wound. The wound is shallow and generally open. The wound bed is viable and may appear like an intact or ruptured blister.[33] The wound area may be painful and the surrounding tissue may be swollen or discolored.[34] See Figure 10.16[35] for an illustration of a Stage 2 pressure injury.
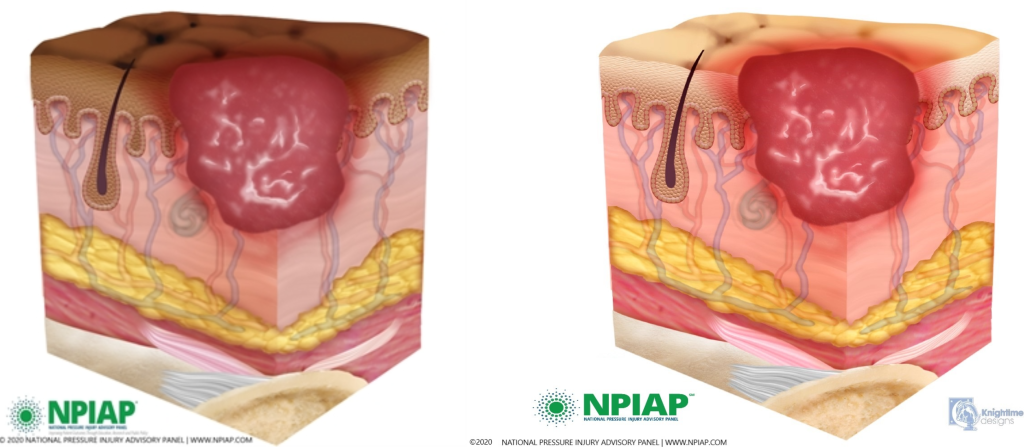
Stage 3 Pressure Injuries
Stage 3 pressure injuries are full-thickness tissue loss in which fat is visible, but cartilage, tendon, ligament, muscle, and bone are not exposed. The depth of tissue damage varies by anatomical location. Because the wound extends through all skin layers, there is increased risk of infection in Stage 3 pressure injuries. There may be pus draining from the wound, tissue necrosis, pain, or fever, especially in the presence of an infection.[36] See Figure 10.17[37] for an illustration of a Stage 3 pressure injury.
Undermining and tunneling may occur in Stage 3 and 4 pressure injuries. Undermining occurs when the tissue under the wound edge becomes eroded, resulting in a pocket beneath the skin. Tunneling refers to passageways underneath the skin surface that extend from a wound and can take twists and turns.
Slough and eschar may also be present in Stage 3 and 4 pressure injuries. Slough is inflammatory exudate that is usually light yellow, soft, and moist. Eschar is dark brown/black, dry, thick, and leathery dead tissue. If slough or eschar obscures the wound so that tissue loss cannot be assessed, the pressure injury is referred to as unstageable.[38] In most wounds, slough and eschar must be removed by debridement for accurate wound staging and for healing to occur. Removed of slough or eschar is surgically performed by specially trained health care providers. Nurses may apply prescribed chemical debridement agents or wet-to-dry dressings for mechanical debridement per provider orders.
Stage 4 Pressure Injuries
Stage 4 pressure injuries are full-thickness tissue loss, like in Stage 3 pressure injuries, but also have exposed cartilage, tendon, ligament, muscle, or bone. Stage 4 pressure injuries are at an increased risk of infection because their depth goes through all skin layers. There may be pain associated with Stage 4 pressure ulcers, although they are often less painful because the wound damages nerve endings. There also at be firm or mushy texture at the site, discoloration, or necrosis to the wound. Because the wound often extends to the bone, thus exposing the bone to infectious agents in the environment, osteomyelitis (bone infection) may also be present. Osteomyelitis is a serious bone infection that may require amputation or cause death if not promptly treated aggressively with antibiotics.[39],[40]
See Figure 10.18[41] for an illustration of a Stage 4 pressure injury.
View images of different stages of pressure injuries on people with dark skin tones on the PPPIA Pressure Ulcers in People With Dark Skin Tones poster.
Unstageable Pressure Injuries
Unstageable pressure injuries are full-thickness skin and tissue loss in which the extent of tissue damage within the ulcer cannot be confirmed because it is obscured by slough or eschar. If slough or eschar were to be removed, a Stage 3 or Stage 4 pressure injury would likely be revealed. However, dry and adherent eschar on the heel or ischemic limb is not typically removed.[42] See Figure 10.19[43] for an illustration of an unstageable pressure ulcer due to the presence of eschar (on the left side of the wound) and slough (on the right side of the wound).
Deep Tissue Pressure Injuries
Deep tissue pressure injuries consist of persistent nonblanchable and deep red, maroon, or purple discoloration of an area. These discolorations typically reveal a dark wound bed or blood-filled blister. Be aware that the discoloration may appear differently in darkly pigmented skin. Deep tissue injury results from intense and/or prolonged pressure, as well as shear forces at the bone-muscle interface. The wound may evolve rapidly to reveal the actual extent of tissue injury, or it may resolve without tissue loss.[44],[45] See Figure 10.20 for an illustration of a deep tissue injury.
Video Review of Assessing Pressure Injuries[46]
Several factors place a client at risk for developing a pressure injury, in addition to shear and friction. These factors include decreased sensory perception, increased moisture, decreased activity, impaired mobility, and inadequate nutrition. The Braden Scale is a standardized, evidence-based assessment tool commonly used in health care to assess and document a client’s risk for developing pressure injuries. See Figure 10.21[47] for an image of a Braden Scale. Risk factors are rated on a scale from 1 to 4, with 1 being “completely limited” and 4 being “no impairment.” The scores from the six categories are added, and the total score indicates a client’s risk for developing a pressure injury based on these ranges:
- Mild risk: 15-18
- Moderate risk: 13-14
- High risk: 10-12
- Severe risk: less than 9
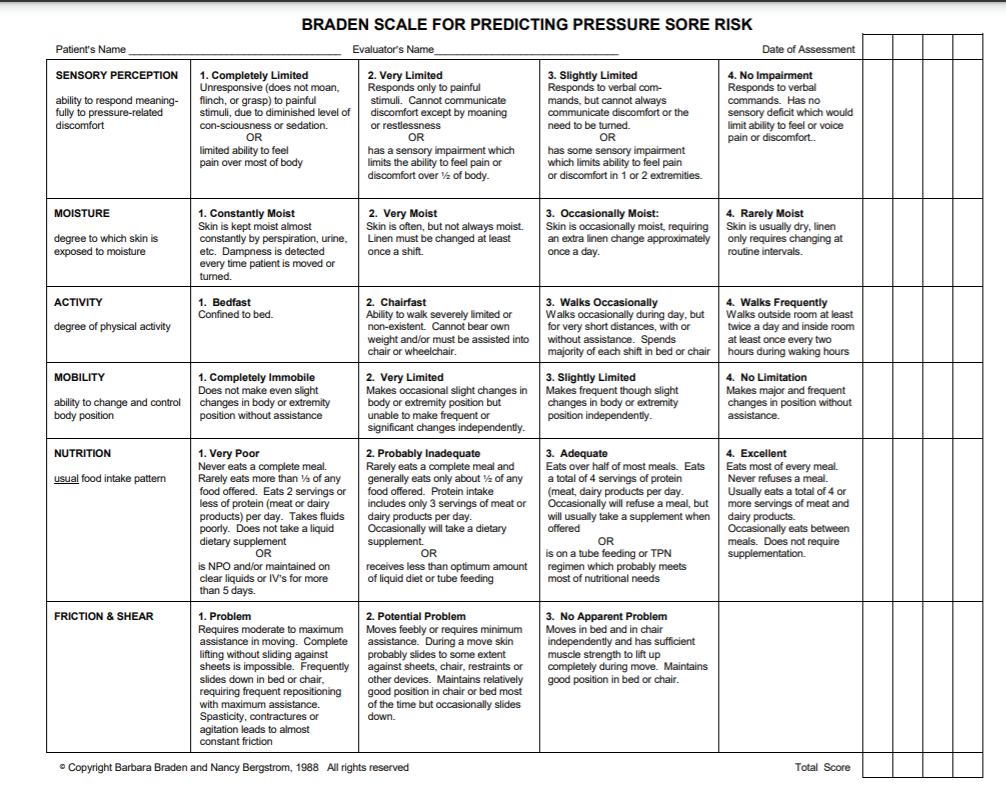
How to Score the Braden Scale
Each risk factor on the Braden Scale is rated from 1 to 4 based on the client’s assessment findings. When using the Braden Scale, start with the first category and review each description listed across the row for each of the ratings from 1 to 4, and choose the one that best describes the client’s current status. Continue this process for all rows. Add all six numbers to determine a total score, and then use the total score to determine if the client is at mild, moderate, high, or severe risk for developing a pressure injury. The lower the score, the higher the risk of developing a pressure injury. Additionally, customized nursing interventions are implemented based on the rating in each category. The lower the score, the more aggressive actions are taken to prevent or heal a pressure injury. Descriptions of the ratings from 1-4 for each risk factor, along with targeted interventions for each rating, are further described in the following subsections.
Sensory Perception
The sensory perception risk factor is defined as the ability to respond meaningfully to pressure-related discomfort. If a client is unable to feel pressure-related discomfort and respond to it appropriately by moving or reporting pain, they are at high risk of developing a pressure injury. This risk category describes two different issues that affect sensory perception. The first description refers to the client’s level of consciousness, and the second description refers to the client’s ability to feel cutaneous sensation. See Table 10.5a for a description of each level of risk from 1-4 with associated interventions for each level.[48]
Table 10.5a Descriptions and Interventions by Level of Risk for Sensory Perception
| Assessment Category | Rating Description | Interventions |
|---|---|---|
| Sensory Perception | 4--No Impairment
Responds to verbal commands. Has no sensory deficit that would limit ability to feel or voice pain or discomfort. |
|
| Sensory Perception | 3--Slightly Limited
Responds to verbal commands but cannot always communicate discomfort or the need to be turned. OR Has some sensory impairment that limits ability to feel pain or discomfort in 1 or 2 extremities. |
|
| Sensory Perception | 2--Very Limited
Responds only to painful stimuli. Cannot communicate discomfort except by moaning or restlessness. OR Has a sensory impairment that limits the ability to feel pain or discomfort over half of the body. |
All interventions mentioned in 3--Slightly Limited plus:
|
| Sensory Perception | 1--Completely Limited
Unresponsive (does not moan, flinch, or grasp) to painful stimuli, due to diminished level of consciousness or sedation. OR Limited ability to feel pain over most of the body. |
All interventions mentioned in 2--Very Limited plus:
|
Moisture
The moisture risk factor is defined as the degree to which skin is exposed to moisture. Prolonged exposure to moisture increases the probability of skin breakdown. Moisture can come from several sources, such as perspiration, urine incontinence, stool incontinence, or wound drainage. Frequent surveillance, removal of wet or soiled linens, and use of protective skin barriers greatly reduce this risk factor. See Table 10.5b for specific interventions for each level of risk.[49]
Table 10.5b Interventions by Level of Risk for Moisture
| Rating Description | Interventions | |
|---|---|---|
| Moisture
|
4--Rarely Moist
Skin is usually dry; linen only requires changing at routine intervals. |
|
| Moisture
|
3--Occasionally Moist
Skin is occasionally moist, requiring an extra linen change approximately once per day. |
All interventions mentioned in 4--Rarely Moist plus:
|
| Moisture
|
2--Often Moist
Skin is often but not always moist. Linen must be changed at least once per shift. |
All interventions mentioned in 3--Occasionally Moist plus:
|
| Moisture
|
1--Constantly Moist
Skin is kept moist almost constantly by perspiration, urine, etc. Dampness is detected every time the client is moved or turned. |
All interventions mentioned in 2--Often Moist plus:
|
Activity
The activity risk factor is defined as the degree of physical activity. For example, walking or moving from a bed to a chair reduces a client’s risk of developing a pressure injury by redistributing pressure points and increasing blood and oxygen flow to areas at risk.
Level of activity is defined by how frequently the client is able to get out of bed, move into a chair, or ambulate with or without help. See Table 10.5c for a description of each level of risk from 1-4 with associated interventions for each.[50]
Table 10.5c Descriptions and Interventions by Level of Risk for Activity[51]
| Assessment Category | Rating Description | Interventions |
|---|---|---|
| Activity
|
4--Walks Frequently
Walks outside the room at least twice a day and inside the room at least once every two hours during waking hours. |
|
| Activity
|
3--Walks Occasionally
Walks occasionally during the day, but for very short distances, with or without assistance. Spends the majority of each shift in bed or chair. |
|
| Activity
|
2--Chair Fast
Ability to walk is severely limited or nonexistent. Cannot bear their own weight and/or must be assisted into chair or wheelchair. |
|
| Activity
|
1--Bedfast
Confined to bed. |
|
Mobility
The mobility risk factor is defined as the client’s ability to change or control their body position. For example, healthy people frequently change body position by rolling over in bed, shifting weight in a chair after sitting too long, or by moving their extremities. However, tissue damage will occur if a client is unable to reposition on their own power unless caregivers frequently change their position. See Table 10.5d for interventions for each level of risk from 1-4.[52]
Table 10.5d Interventions by Level of Risk for Mobility[53]
| Assessment Category | Rating Description | Interventions |
|---|---|---|
| Mobility
|
4--No Limitations
Makes major and frequent changes in position without assistance. |
|
| Mobility
|
3--Slightly Limited
Makes frequent though slight changes in body or extremity position independently. |
|
| Mobility
|
2--Very Limited
Makes occasional slight changes in body or extremity position but unable to make frequent or significant changes independently. |
|
| Mobility
|
1-Completely Immobile
Does not make even slight changes in body or extremity position without assistance. |
Same interventions as for 2--Very Limited |
Nutrition
Adequate nutrition and fluid intake are vital for maintaining healthy skin. Protein intake, in particular, is very important for healthy skin and wound healing. The nutrition risk factor is defined by two categories of descriptions. The first category measures the amount and type of oral intake. The second category is used for clients receiving tube feeding, total parenteral nutrition (TPN), or are prescribed clear liquid diets or nothing by mouth (NPO). See Table 10.5e for interventions for each level of risk from 1-4.[54]
Table 10.5e Interventions by Level of Risk for Nutrition[55]
| Assessment Category | Rating Description | Interventions |
|---|---|---|
| Nutrition
|
4--Excellent
Eats most of every meal. Never refuses a meal. Usually eats a total of 4 or more servings of meat and dairy products. Occasionally eats between meals. Does not require supplementation. |
|
| Nutrition
|
3--Adequate
Eats over half of most meals. Eats a total of 4 servings of protein (meat and dairy products) each day. Occasionally refuses a meal, but will take a supplement if offered OR Is on a tube feeding or TPN regimen that most likely meets most of nutritional needs |
|
| Nutrition
|
2--Probably Inadequate
Rarely eats a complete meal and generally eats only about half of any food offered. Protein intake includes only 3 servings of meat or dairy products per day. Occasionally will take a dairy supplement OR Receives less than optimum amount of liquid diet or tube feeding. |
All interventions mentioned in 3--Adequate plus:
|
| Nutrition
|
1--Very Poor
Never eats a complete meal. Rarely eats more than one third of any food offered. Eats two servings of protein (meat or dairy products) per day. Takes fluids poorly. Does not take a liquid dietary supplement OR Is NPO and/or maintained on clear liquids or IV for more than 5 days. |
All interventions mentioned in 2--Probably Inadequate plus:
|
Friction/Shear
Friction and shear are significant risk factors for producing pressure injuries. This category only has three ratings, unlike the other categories that have four ratings, and is rated by whether the client has a problem, potential problem, or no apparent problem in this area. See Table 10.5f for interventions for each level of risk.[56]
Table 10.5f Descriptions and Interventions by Level of Risk for Friction/Shear[57]
| Assessment Category | Rating Description | Interventions |
|---|---|---|
| Friction/Shear
|
3--No Apparent Problem
Moves in bed and chair independently and has sufficient muscle strength to lift up completely during move. Maintains good position in bed or chair at all times. |
Keep bed linens clean, dry, and wrinkle free. |
| Friction/Shear
|
2--Potential Problem
Moves feebly or requires minimal assistance. During a move, skin probably slides to some extent against sheets, chair, restraints, or other devices. Maintains a relatively good position in a chair or bed most of the time but occasionally slides down. |
All interventions mentioned in 3--No Apparent Problem plus:
|
| Friction/Shear
|
1--Problem
Requires moderate to maximum assistance in moving. Complete lifting without sliding against sheets is impossible. Frequently slides down in bed or chair, requiring frequent repositioning with maximum assistance. Spasticity, contractures, or agitation leads to almost constant friction. |
All interventions mentioned in 2--Potential Problem plus:
|
Team Member Roles to Prevent Pressure Injuries
Each member of the health care team has an important role in preventing the development of pressure injuries in at-risk clients. A registered nurse can delegate many interventions for preventing and treating a pressure injury to a licensed practical nurse (LPN) or to unlicensed assistive personnel such as a certified nursing assistant (CNA). See Table 10.5g for an explanation of the role of the RN in preventing pressure injuries, as well as tasks that can be delegated to LPNs and CNAs.
Table 10.5g Team Member Roles in Preventing Pressure Injuries[58]
| Role | Tasks |
|---|---|
| RN |
|
| LPN |
|
| CNA |
|
Several factors place a client at risk for developing a pressure injury, in addition to shear and friction. These factors include decreased sensory perception, increased moisture, decreased activity, impaired mobility, and inadequate nutrition. The Braden Scale is a standardized, evidence-based assessment tool commonly used in health care to assess and document a client’s risk for developing pressure injuries. See Figure 10.21[59] for an image of a Braden Scale. Risk factors are rated on a scale from 1 to 4, with 1 being “completely limited” and 4 being “no impairment.” The scores from the six categories are added, and the total score indicates a client’s risk for developing a pressure injury based on these ranges:
- Mild risk: 15-18
- Moderate risk: 13-14
- High risk: 10-12
- Severe risk: less than 9
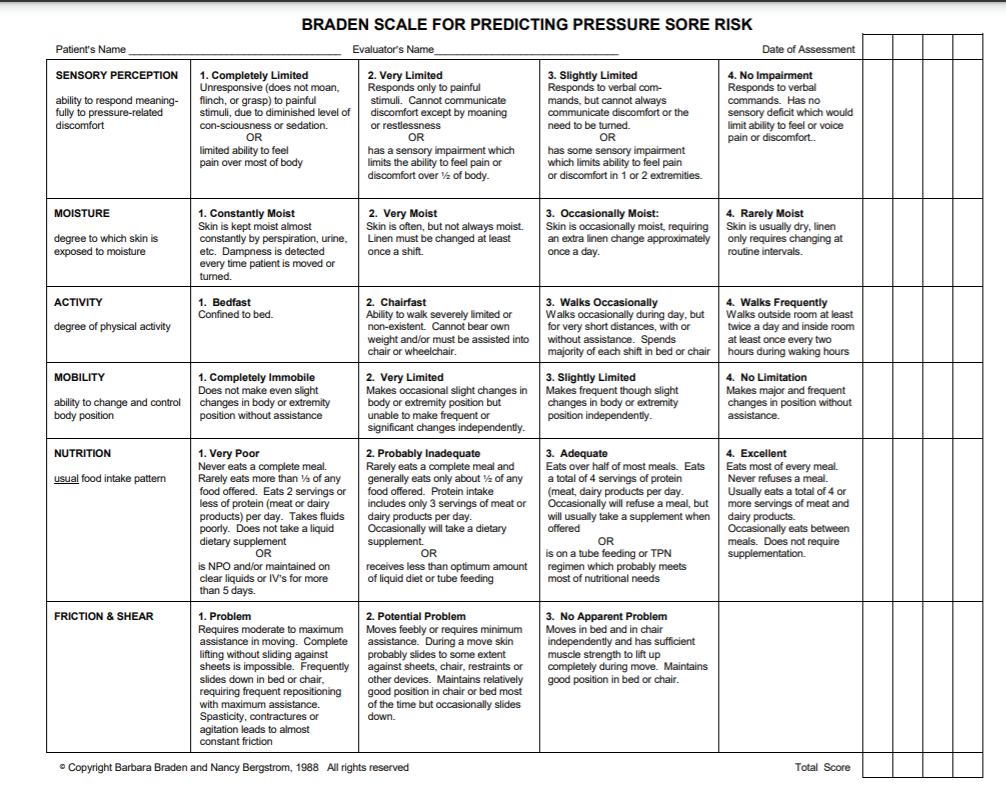
How to Score the Braden Scale
Each risk factor on the Braden Scale is rated from 1 to 4 based on the client’s assessment findings. When using the Braden Scale, start with the first category and review each description listed across the row for each of the ratings from 1 to 4, and choose the one that best describes the client’s current status. Continue this process for all rows. Add all six numbers to determine a total score, and then use the total score to determine if the client is at mild, moderate, high, or severe risk for developing a pressure injury. The lower the score, the higher the risk of developing a pressure injury. Additionally, customized nursing interventions are implemented based on the rating in each category. The lower the score, the more aggressive actions are taken to prevent or heal a pressure injury. Descriptions of the ratings from 1-4 for each risk factor, along with targeted interventions for each rating, are further described in the following subsections.
Sensory Perception
The sensory perception risk factor is defined as the ability to respond meaningfully to pressure-related discomfort. If a client is unable to feel pressure-related discomfort and respond to it appropriately by moving or reporting pain, they are at high risk of developing a pressure injury. This risk category describes two different issues that affect sensory perception. The first description refers to the client’s level of consciousness, and the second description refers to the client’s ability to feel cutaneous sensation. See Table 10.5a for a description of each level of risk from 1-4 with associated interventions for each level.[60]
Table 10.5a Descriptions and Interventions by Level of Risk for Sensory Perception
| Assessment Category | Rating Description | Interventions |
|---|---|---|
| Sensory Perception | 4--No Impairment
Responds to verbal commands. Has no sensory deficit that would limit ability to feel or voice pain or discomfort. |
|
| Sensory Perception | 3--Slightly Limited
Responds to verbal commands but cannot always communicate discomfort or the need to be turned. OR Has some sensory impairment that limits ability to feel pain or discomfort in 1 or 2 extremities. |
|
| Sensory Perception | 2--Very Limited
Responds only to painful stimuli. Cannot communicate discomfort except by moaning or restlessness. OR Has a sensory impairment that limits the ability to feel pain or discomfort over half of the body. |
All interventions mentioned in 3--Slightly Limited plus:
|
| Sensory Perception | 1--Completely Limited
Unresponsive (does not moan, flinch, or grasp) to painful stimuli, due to diminished level of consciousness or sedation. OR Limited ability to feel pain over most of the body. |
All interventions mentioned in 2--Very Limited plus:
|
Moisture
The moisture risk factor is defined as the degree to which skin is exposed to moisture. Prolonged exposure to moisture increases the probability of skin breakdown. Moisture can come from several sources, such as perspiration, urine incontinence, stool incontinence, or wound drainage. Frequent surveillance, removal of wet or soiled linens, and use of protective skin barriers greatly reduce this risk factor. See Table 10.5b for specific interventions for each level of risk.[61]
Table 10.5b Interventions by Level of Risk for Moisture
| Rating Description | Interventions | |
|---|---|---|
| Moisture
|
4--Rarely Moist
Skin is usually dry; linen only requires changing at routine intervals. |
|
| Moisture
|
3--Occasionally Moist
Skin is occasionally moist, requiring an extra linen change approximately once per day. |
All interventions mentioned in 4--Rarely Moist plus:
|
| Moisture
|
2--Often Moist
Skin is often but not always moist. Linen must be changed at least once per shift. |
All interventions mentioned in 3--Occasionally Moist plus:
|
| Moisture
|
1--Constantly Moist
Skin is kept moist almost constantly by perspiration, urine, etc. Dampness is detected every time the client is moved or turned. |
All interventions mentioned in 2--Often Moist plus:
|
Activity
The activity risk factor is defined as the degree of physical activity. For example, walking or moving from a bed to a chair reduces a client’s risk of developing a pressure injury by redistributing pressure points and increasing blood and oxygen flow to areas at risk.
Level of activity is defined by how frequently the client is able to get out of bed, move into a chair, or ambulate with or without help. See Table 10.5c for a description of each level of risk from 1-4 with associated interventions for each.[62]
Table 10.5c Descriptions and Interventions by Level of Risk for Activity[63]
| Assessment Category | Rating Description | Interventions |
|---|---|---|
| Activity
|
4--Walks Frequently
Walks outside the room at least twice a day and inside the room at least once every two hours during waking hours. |
|
| Activity
|
3--Walks Occasionally
Walks occasionally during the day, but for very short distances, with or without assistance. Spends the majority of each shift in bed or chair. |
|
| Activity
|
2--Chair Fast
Ability to walk is severely limited or nonexistent. Cannot bear their own weight and/or must be assisted into chair or wheelchair. |
|
| Activity
|
1--Bedfast
Confined to bed. |
|
Mobility
The mobility risk factor is defined as the client’s ability to change or control their body position. For example, healthy people frequently change body position by rolling over in bed, shifting weight in a chair after sitting too long, or by moving their extremities. However, tissue damage will occur if a client is unable to reposition on their own power unless caregivers frequently change their position. See Table 10.5d for interventions for each level of risk from 1-4.[64]
Table 10.5d Interventions by Level of Risk for Mobility[65]
| Assessment Category | Rating Description | Interventions |
|---|---|---|
| Mobility
|
4--No Limitations
Makes major and frequent changes in position without assistance. |
|
| Mobility
|
3--Slightly Limited
Makes frequent though slight changes in body or extremity position independently. |
|
| Mobility
|
2--Very Limited
Makes occasional slight changes in body or extremity position but unable to make frequent or significant changes independently. |
|
| Mobility
|
1-Completely Immobile
Does not make even slight changes in body or extremity position without assistance. |
Same interventions as for 2--Very Limited |
Nutrition
Adequate nutrition and fluid intake are vital for maintaining healthy skin. Protein intake, in particular, is very important for healthy skin and wound healing. The nutrition risk factor is defined by two categories of descriptions. The first category measures the amount and type of oral intake. The second category is used for clients receiving tube feeding, total parenteral nutrition (TPN), or are prescribed clear liquid diets or nothing by mouth (NPO). See Table 10.5e for interventions for each level of risk from 1-4.[66]
Table 10.5e Interventions by Level of Risk for Nutrition[67]
| Assessment Category | Rating Description | Interventions |
|---|---|---|
| Nutrition
|
4--Excellent
Eats most of every meal. Never refuses a meal. Usually eats a total of 4 or more servings of meat and dairy products. Occasionally eats between meals. Does not require supplementation. |
|
| Nutrition
|
3--Adequate
Eats over half of most meals. Eats a total of 4 servings of protein (meat and dairy products) each day. Occasionally refuses a meal, but will take a supplement if offered OR Is on a tube feeding or TPN regimen that most likely meets most of nutritional needs |
|
| Nutrition
|
2--Probably Inadequate
Rarely eats a complete meal and generally eats only about half of any food offered. Protein intake includes only 3 servings of meat or dairy products per day. Occasionally will take a dairy supplement OR Receives less than optimum amount of liquid diet or tube feeding. |
All interventions mentioned in 3--Adequate plus:
|
| Nutrition
|
1--Very Poor
Never eats a complete meal. Rarely eats more than one third of any food offered. Eats two servings of protein (meat or dairy products) per day. Takes fluids poorly. Does not take a liquid dietary supplement OR Is NPO and/or maintained on clear liquids or IV for more than 5 days. |
All interventions mentioned in 2--Probably Inadequate plus:
|
Friction/Shear
Friction and shear are significant risk factors for producing pressure injuries. This category only has three ratings, unlike the other categories that have four ratings, and is rated by whether the client has a problem, potential problem, or no apparent problem in this area. See Table 10.5f for interventions for each level of risk.[68]
Table 10.5f Descriptions and Interventions by Level of Risk for Friction/Shear[69]
| Assessment Category | Rating Description | Interventions |
|---|---|---|
| Friction/Shear
|
3--No Apparent Problem
Moves in bed and chair independently and has sufficient muscle strength to lift up completely during move. Maintains good position in bed or chair at all times. |
Keep bed linens clean, dry, and wrinkle free. |
| Friction/Shear
|
2--Potential Problem
Moves feebly or requires minimal assistance. During a move, skin probably slides to some extent against sheets, chair, restraints, or other devices. Maintains a relatively good position in a chair or bed most of the time but occasionally slides down. |
All interventions mentioned in 3--No Apparent Problem plus:
|
| Friction/Shear
|
1--Problem
Requires moderate to maximum assistance in moving. Complete lifting without sliding against sheets is impossible. Frequently slides down in bed or chair, requiring frequent repositioning with maximum assistance. Spasticity, contractures, or agitation leads to almost constant friction. |
All interventions mentioned in 2--Potential Problem plus:
|
Team Member Roles to Prevent Pressure Injuries
Each member of the health care team has an important role in preventing the development of pressure injuries in at-risk clients. A registered nurse can delegate many interventions for preventing and treating a pressure injury to a licensed practical nurse (LPN) or to unlicensed assistive personnel such as a certified nursing assistant (CNA). See Table 10.5g for an explanation of the role of the RN in preventing pressure injuries, as well as tasks that can be delegated to LPNs and CNAs.
Table 10.5g Team Member Roles in Preventing Pressure Injuries[70]
| Role | Tasks |
|---|---|
| RN |
|
| LPN |
|
| CNA |
|
Assessment
Subjective Assessment
During a subjective assessment of a client’s integumentary system, begin by asking about current symptoms such as itching, rashes, or wounds. If a client has a wound, it is important to determine if a client has pain associated with the wound so that pain management can be implemented. For clients with chronic wounds, it is also important to identify factors that delay wound healing, such as nutrition, decreased oxygenation, infection, stress, diabetes, obesity, medications, alcohol use, and smoking.[71] See Table 10.6a for a list of suggested interview questions to use when assessing a client with a wound.
If a client has a chronic wound or is experiencing delayed wound healing, it is important for the nurse to assess the impact of the wound on their quality of life. Reasons for this may include the frequency and regularity of dressing changes, which affect daily routine; a feeling of continued fatigue due to lack of sleep; restricted mobility; pain; odor; and the side effects of multiple medications. The loss of independence associated with functional decline can also lead to changes in overall health and well-being. These changes include altered eating habits, depression, social isolation, and a gradual reduction in activity levels.
Table 10.6a Interview Questions Related to Integumentary Disorders
| Symptoms | Questions | Follow-up Questions |
|---|---|---|
| Current Symptoms | Are you currently experiencing any skin symptoms such as itching, rashes, or an unusual mole? | Please describe. |
| Wounds | Do you have any current wounds such as a surgical incision, skin tear, arterial ulcer, venous ulcer, diabetic or neuropathic ulcer, or a pressure injury?
If a wound is present:
|
Please describe.
Use the PQRSTU method to comprehensively assess pain. Read more about the PQRSTU method in the "Pain Assessment Methods" section of the "Comfort" chapter. |
| Medical History | Have you ever been diagnosed with a wound related to diabetes, heart disease, or peripheral vascular disease? | Please describe. |
| If chronic wounds or wounds with delayed healing are present: | ||
| Medications | Are you taking any medications that can affect wound healing, such as oral steroids to treat inflammation or help you breathe? | Please describe. |
| Treatments | What have you used to try to treat this wound? | What was successful? Unsuccessful? |
| Symptoms of Infection (pain, purulent drainage, etc.) | Are you experiencing any symptoms of infection related to this wound such as increased pain or yellow/green drainage? | Please describe. |
| Stress | Have you experienced any recent stressors such as surgery, hospitalization, or a change in life circumstances? | How do you cope with stress in your life? |
| Smoking | Do you smoke? | How many cigarettes do you smoke a day? How long have you smoked? Have you considered quitting smoking? |
| Quality of Life | Has this wound impacted your quality of life? | Have you had any changes in eating habits, feelings of depression or social isolation, or a reduction in your usual activity levels? |
Objective Assessment
When performing an objective integumentary assessment on a client receiving inpatient care, it is important to perform a thorough exam on admission to check for existing wounds, as well as to evaluate their risk of skin breakdown using the Braden Scale. Agencies are not reimbursed for care of pressure injuries received during a client’s stay, so existing wounds on admission must be well-documented. Routine skin assessment should continue throughout a client’s stay, usually on a daily or shift-by-shift basis based on the client’s condition. If a wound is present, it is assessed during every dressing change for signs of healing. See Table 10.6b for components to include in a wound assessment. See Figure 10.22[72] for an image of a common tool used to document the location of a skin concern found during assessment.
Read more information about performing an overall integumentary assessment in the “Integumentary Assessment” chapter in Open RN Nursing Skills, 2e.
For additional discussion regarding assessing wounds, go to the “Assessing Wounds” section of the “Wound Care” chapter in Open RN Nursing Skills, 2e.
There are many common skin disorders that a nurse may find during assessment. Read more about common skin disorders in the “Common Integumentary Conditions” section of the “Integumentary Assessment” chapter in Open RN Nursing Skills, 2e.
Table 10.6b Wound Assessment
| Wound Assessment | |
|---|---|
| Type | Types of wounds may include abrasions, lacerations, burns, surgical incisions, pressure injuries, skin tears, arterial ulcers, or venous ulcers. It is important to understand the type of wound present to select appropriate interventions. |
| Location | The location of the wound should be documented precisely. A body diagram template is helpful to demonstrate exactly where the wound is located. |
| Size | Wound size should be measured regularly to determine if the wound is increasing or decreasing in size. Length is measured using the head-to-toe axis, and width is measured laterally. If tunneling or undermining is present, their depth should be assessed using a sterile, cotton-tipped applicator and documented using the clock method. |
| Degree of Tissue Injury | Wounds are classified as partial-thickness (meaning the epidermis and dermis are affected) or full-thickness (meaning the subcutaneous and deeper layers are affected). See Figure 10.1 in the “Basic Concepts” section for an image of the layers of skin.
For pressure injuries, it is important to assess the stage of the injury (see information on staging in the “Pressure Injuries” section). |
| Color of Wound Base | Assess the base of the wound for the presence of healthy, pink/red granulation tissue. Note the unhealthy appearance of dark red granulation tissue, white or yellow slough, or brown or black necrotic tissue. |
| Drainage | The color, consistency, and amount of exudate (drainage) should be assessed and documented at every dressing change. Drainage from wounds is often described as scant, small/minimal, moderate, and large/copious amounts. Use the following descriptions to select the appropriate terms:[73]
The type of wound drainage should be described using medical terms such as serosanguinous, sanguineous, serous, or purulent:
|
| Tubes or Drains | Check for patency and if they are attached correctly. |
| Signs and Symptoms of Infection | Assess for signs and symptoms of infection, which include the following:
|
| Wound Edges and Periwound | Assess the surrounding skin for maceration or signs of infection. |
| Pain | Assess for pain in the wound or during dressing changes. If pain is present, use the PQRSTU or OLDCARTES method to obtain a comprehensive pain assessment. |

See Table 10.6c for a comparison of expected versus unexpected findings on integumentary assessment.
Table 10.6c Expected Versus Unexpected Findings
| Assessment | Expected Findings | Unexpected Findings |
|---|---|---|
| Skin | Color: appropriate for ethnicity
Temperature: warm to touch Texture: smooth, soft, and supple Turgor: resilient Integrity: no wounds or lesions noted Sensory: no pain or itching noted |
Color: pale, white, red, yellow, purple, black and blue
Temperature: cool or hot to touch Texture: rough, scaly or thick; thin and easily torn; dry and cracked Turgor: tenting noted Integrity: rashes, lesions, abrasions, burns, lacerations, surgical wounds, pressure injuries noted Pain or pruritus (itching) present |
| Hair | Full distribution of hair on the head, axilla, and genitalia | Alopecia (hair loss), hirsutism (excessive hair growth over body), lice and/or nits, or lesions under hair |
| Nails | Smooth, well-shaped, and firm but flexible | Cracked, chipped, or splitting nail; excessively thick; presence of clubbing; ingrown nails |
| Skin Integrity | Skin intact with no wounds or pressure injuries. Braden Scale is 23 | A wound or pressure injury is present, or there is risk of developing a pressure injury with a Braden scale score of less than 23 |
Diagnostic and Lab Work
When a chronic wound is not healing as expected, laboratory test results can provide additional clues for the delayed healing. See Table 10.6d for a summary of lab results that offer clues to systemic issues causing delayed wound healing.
Table 10.6d Lab Values Associated with Delayed Wound Healing[79]
| Abnormal Lab Value | Rationale |
|---|---|
| Low hemoglobin | Low hemoglobin indicates less oxygen is transported to the wound site. |
| Elevated white blood cells (WBC) | Increased WBC indicates infection is occurring. |
| Low platelets | Platelets have an important role in the creation of granulation tissue. |
| Low albumin | Low albumin indicates decreased protein levels. Protein is required for effective wound healing. |
| Elevated blood glucose or hemoglobin A1C | Elevated blood glucose and hemoglobin A1C levels indicate poor management of diabetes mellitus, a disease that negatively impacts wound healing. |
| Elevated serum BUN and creatinine | BUN and creatinine levels are indicators of kidney function, with elevated levels indicating worsening kidney function. Elevated BUN (blood urea nitrogen) levels impact wound healing because it can indicate increased breakdown of the body's protein stores due to deficient protein in the diet. |
| Positive wound culture | Positive wound cultures indicate an infection is present and provide additional information including the type and number of bacteria present, as well as identifying antibiotics the bacteria is susceptible to. The nurse reviews this information when administering antibiotics to ensure the prescribed therapy is effective for the type of bacteria present. |
Life Span and Cultural Considerations
Newborns and Infants
Newborn skin is thin and sensitive. It tends to be easy to scratch and bruise and is susceptible to rashes and irritation. Common rashes seen in newborns and infants include diaper rash (contact dermatitis), cradle cap (seborrheic dermatitis), newborn acne, and prickly heat.
Toddlers and Preschoolers
Because of high levels of activity and increasing mobility, this age group is more prone to accidents. Issues like lacerations, abrasions, burns, and sunburns can occur frequently. It is important to be highly aware of the potential for accidents and implement safety precautions as needed.
School-Aged Children and Adolescents
Skin rashes tend to affect skin within this age group. Impetigo, scabies, and head lice are commonly seen and may keep children home from school. Acne vulgaris typically begins during adolescence and can alter physical appearance, which can be very upsetting to this age group. Another change during adolescence is the appearance of axillary, pubic, and other body hair. Also, as these children spend more time out of doors, sunburns are more common, and care should be given to encourage sunscreen and discourage the use of tanning beds.
Adults and Older Adults
As skin ages, many changes take place. Because aging increases the loss of subcutaneous fat and collagen breakdown, skin becomes thinner and wrinkles deepen. Decreased sweat gland activity leads to drier skin and pruritus (itching). Wound healing is slowed because of reduced circulation and the inability of proteins and proper nutrients to arrive at injury sites. Hair loses pigmentation and turns gray or white. Nails become thicker and are more difficult to cut. Age or liver spots become darker and more noticeable. The number of skin growths increases and includes skin tags and keratoses.
Diagnoses
There are several NANDA-I nursing diagnoses related to clients experiencing skin alterations or those at risk of developing a skin injury. See Table 10.6e for common NANDA-I nursing diagnoses and their definitions.[80]
Table 10.6e Common NANDA-I Nursing Diagnoses Related to Integumentary Disorders[81]
| Risk for Pressure Injury: “Susceptible to localized injury to the skin and/or underlying tissue usually over a bony prominence as a result of pressure, or pressure in combination with shear.” |
| Impaired Skin Integrity: “Altered epidermis and/or dermis.” |
| Risk for Impaired Skin Integrity: “Susceptible to alteration in epidermis and/or dermis, which may compromise health.” |
| Impaired Tissue Integrity: “Damage to the mucous membrane, cornea, integumentary system, muscular fascia, muscle, tendon, bone, cartilage, joint capsule, and/or ligament.” |
| Risk for Impaired Tissue Integrity: “Susceptible to damage to the mucous membrane, cornea, integumentary system, muscular fascia, muscle, tendon, bone, cartilage, joint capsule, and/or ligament, which may compromise health.” |
A commonly used NANDA-I nursing diagnosis for clients experiencing alterations in the integumentary system is Impaired Tissue Integrity, defined as, “Damage to the mucous membrane, cornea, integumentary system, muscular fascia, muscle, tendon, bone, cartilage, joint capsule, and/or ligament.”
To verify accuracy of this diagnosis for a client, the nurse compares assessment findings with defining characteristics of that diagnosis. Defining characteristics for Impaired Tissue Integrity include the following:
- Acute pain
- Bleeding
- Destroyed tissue
- Hematoma
- Localized area hot to touch
- Redness
- Tissue damage
A sample NANDA-I diagnosis in current PES format would be: “Impaired Tissue Integrity related to insufficient knowledge about protecting tissue integrity as evidenced by redness and tissue damage.”
Outcome Identification
An example of a broad goal for a client experiencing alterations in tissue integrity is:
- The client will experience tissue healing.
A sample SMART expected outcome for a client with a wound is:
- The client’s wound will decrease in size and have increased granulation tissue within two weeks.
Planning Interventions
In addition to the interventions outlined under the “Braden Scale” section to prevent and treat pressure injury, see the following box for a list of interventions to prevent and treat impaired skin integrity. As always, consult a current, evidence-based nurse care planning resource for additional interventions when planning client care.
Selected Interventions to Prevent and Treat Impaired Skin Integrity [82],[83],[84]
- Assess and document the client’s skin status routinely. (Frequency is determined based on the client’s status.)
- Use the Braden Scale to identify clients at risk for skin breakdown. Customize interventions to prevent and treat skin breakdown according to client needs.
- If a wound is present, evaluate the healing process at every dressing change. Note and document characteristics of the wound, including size, appearance, staging (if applicable), and drainage. Notify the provider of new signs of infection or lack of progress in healing.
- Provide wound care treatments, as prescribed by the provider or wound care specialist, and monitor the client's response toward expected outcomes.
- Cleanse the wound per facility protocol or as ordered.
- Maintain non-touch or aseptic technique when performing wound dressing changes, as indicated. (Read more details about using aseptic technique and the non-touch method in the "Aseptic Technique" chapter of the Open RN Nursing Skills,2e textbook.)
- Change wound dressings as needed to keep them clean and dry and prevent bacterial reservoir.
- Monitor for signs of infection in an existing wound (as indicated by redness, warmth, edema, increased pain, reddened appearance of surrounding skin, fever, increased white blood cell count, changes in wound drainage, or sudden change in client’s level of consciousness).
- Apply lotion to dry areas to prevent cracking.
- Apply lubricant to moisten lips and oral mucosa, as needed.
- Keep skin free of excess moisture. Use moisture barrier ointments (protective skin barriers) or incontinence products in skin areas subject to increased moisture and risk of skin breakdown.
- Educate the client and/or family caregivers on caring for the wound and request return demonstrations, as appropriate.
- Administer medications, as prescribed, and monitor for expected effects.
- Consult with a wound specialist, as needed.
- Obtain specimens of wound drainage for wound culture, as indicated, and monitor results.
- Advocate for pressure-relieving devices in clients at risk for pressure injuries, such as elbow protectors, heel protectors, chair cushions, and specialized mattresses and monitor the client's response.
- Promote adequate nutrition and hydration intake, unless contraindicated.
- Use a minimum of two-person assistance and a draw sheet to pull a client up in bed to minimize shear and friction.
- Reposition the client frequently to prevent skin breakdown and to promote healing. Turn the immobilized client at least every two hours, according to a specific schedule.
- Maintain a client’s position at 30 degrees or less, as appropriate, to prevent shear.
- Keep bed linens clean, dry, and wrinkle free.
Implementation
Before implementing interventions, it is important to assess the current status of the skin and risk factors present for skin breakdown and modify interventions based on the client’s current status. For example, if a client's rash has resolved, some interventions may no longer be appropriate (such as applying topical creams). However, if a wound is showing signs of worsening or delayed healing, additional interventions may be required. As always, if the client demonstrates new signs of localized or systemic infection, the provider should be notified.
Evaluation
It is important to evaluate for healing when performing wound care. Use the following expected outcomes when evaluating wound healing:
- Resolution of periwound redness in 1 week
- 50% reduction in wound dimensions in 2 weeks
- Reduction in volume of exudate
- 25% reduction in amount of necrotic tissue/eschar in 1 week
- Decreased pain intensity during dressing changes[85]
If a client is experiencing delayed wound healing or has a chronic wound, it is helpful to advocate for a referral to a wound care nurse specialist.
Read a sample nursing care plan for a client with impaired skin integrity.
Assessment
Subjective Assessment
During a subjective assessment of a client’s integumentary system, begin by asking about current symptoms such as itching, rashes, or wounds. If a client has a wound, it is important to determine if a client has pain associated with the wound so that pain management can be implemented. For clients with chronic wounds, it is also important to identify factors that delay wound healing, such as nutrition, decreased oxygenation, infection, stress, diabetes, obesity, medications, alcohol use, and smoking.[86] See Table 10.6a for a list of suggested interview questions to use when assessing a client with a wound.
If a client has a chronic wound or is experiencing delayed wound healing, it is important for the nurse to assess the impact of the wound on their quality of life. Reasons for this may include the frequency and regularity of dressing changes, which affect daily routine; a feeling of continued fatigue due to lack of sleep; restricted mobility; pain; odor; and the side effects of multiple medications. The loss of independence associated with functional decline can also lead to changes in overall health and well-being. These changes include altered eating habits, depression, social isolation, and a gradual reduction in activity levels.
Table 10.6a Interview Questions Related to Integumentary Disorders
| Symptoms | Questions | Follow-up Questions |
|---|---|---|
| Current Symptoms | Are you currently experiencing any skin symptoms such as itching, rashes, or an unusual mole? | Please describe. |
| Wounds | Do you have any current wounds such as a surgical incision, skin tear, arterial ulcer, venous ulcer, diabetic or neuropathic ulcer, or a pressure injury?
If a wound is present:
|
Please describe.
Use the PQRSTU method to comprehensively assess pain. Read more about the PQRSTU method in the "Pain Assessment Methods" section of the "Comfort" chapter. |
| Medical History | Have you ever been diagnosed with a wound related to diabetes, heart disease, or peripheral vascular disease? | Please describe. |
| If chronic wounds or wounds with delayed healing are present: | ||
| Medications | Are you taking any medications that can affect wound healing, such as oral steroids to treat inflammation or help you breathe? | Please describe. |
| Treatments | What have you used to try to treat this wound? | What was successful? Unsuccessful? |
| Symptoms of Infection (pain, purulent drainage, etc.) | Are you experiencing any symptoms of infection related to this wound such as increased pain or yellow/green drainage? | Please describe. |
| Stress | Have you experienced any recent stressors such as surgery, hospitalization, or a change in life circumstances? | How do you cope with stress in your life? |
| Smoking | Do you smoke? | How many cigarettes do you smoke a day? How long have you smoked? Have you considered quitting smoking? |
| Quality of Life | Has this wound impacted your quality of life? | Have you had any changes in eating habits, feelings of depression or social isolation, or a reduction in your usual activity levels? |
Objective Assessment
When performing an objective integumentary assessment on a client receiving inpatient care, it is important to perform a thorough exam on admission to check for existing wounds, as well as to evaluate their risk of skin breakdown using the Braden Scale. Agencies are not reimbursed for care of pressure injuries received during a client’s stay, so existing wounds on admission must be well-documented. Routine skin assessment should continue throughout a client’s stay, usually on a daily or shift-by-shift basis based on the client’s condition. If a wound is present, it is assessed during every dressing change for signs of healing. See Table 10.6b for components to include in a wound assessment. See Figure 10.22[87] for an image of a common tool used to document the location of a skin concern found during assessment.
Read more information about performing an overall integumentary assessment in the “Integumentary Assessment” chapter in Open RN Nursing Skills, 2e.
For additional discussion regarding assessing wounds, go to the “Assessing Wounds” section of the “Wound Care” chapter in Open RN Nursing Skills, 2e.
There are many common skin disorders that a nurse may find during assessment. Read more about common skin disorders in the “Common Integumentary Conditions” section of the “Integumentary Assessment” chapter in Open RN Nursing Skills, 2e.
Table 10.6b Wound Assessment
| Wound Assessment | |
|---|---|
| Type | Types of wounds may include abrasions, lacerations, burns, surgical incisions, pressure injuries, skin tears, arterial ulcers, or venous ulcers. It is important to understand the type of wound present to select appropriate interventions. |
| Location | The location of the wound should be documented precisely. A body diagram template is helpful to demonstrate exactly where the wound is located. |
| Size | Wound size should be measured regularly to determine if the wound is increasing or decreasing in size. Length is measured using the head-to-toe axis, and width is measured laterally. If tunneling or undermining is present, their depth should be assessed using a sterile, cotton-tipped applicator and documented using the clock method. |
| Degree of Tissue Injury | Wounds are classified as partial-thickness (meaning the epidermis and dermis are affected) or full-thickness (meaning the subcutaneous and deeper layers are affected). See Figure 10.1 in the “Basic Concepts” section for an image of the layers of skin.
For pressure injuries, it is important to assess the stage of the injury (see information on staging in the “Pressure Injuries” section). |
| Color of Wound Base | Assess the base of the wound for the presence of healthy, pink/red granulation tissue. Note the unhealthy appearance of dark red granulation tissue, white or yellow slough, or brown or black necrotic tissue. |
| Drainage | The color, consistency, and amount of exudate (drainage) should be assessed and documented at every dressing change. Drainage from wounds is often described as scant, small/minimal, moderate, and large/copious amounts. Use the following descriptions to select the appropriate terms:[88]
The type of wound drainage should be described using medical terms such as serosanguinous, sanguineous, serous, or purulent:
|
| Tubes or Drains | Check for patency and if they are attached correctly. |
| Signs and Symptoms of Infection | Assess for signs and symptoms of infection, which include the following:
|
| Wound Edges and Periwound | Assess the surrounding skin for maceration or signs of infection. |
| Pain | Assess for pain in the wound or during dressing changes. If pain is present, use the PQRSTU or OLDCARTES method to obtain a comprehensive pain assessment. |

See Table 10.6c for a comparison of expected versus unexpected findings on integumentary assessment.
Table 10.6c Expected Versus Unexpected Findings
| Assessment | Expected Findings | Unexpected Findings |
|---|---|---|
| Skin | Color: appropriate for ethnicity
Temperature: warm to touch Texture: smooth, soft, and supple Turgor: resilient Integrity: no wounds or lesions noted Sensory: no pain or itching noted |
Color: pale, white, red, yellow, purple, black and blue
Temperature: cool or hot to touch Texture: rough, scaly or thick; thin and easily torn; dry and cracked Turgor: tenting noted Integrity: rashes, lesions, abrasions, burns, lacerations, surgical wounds, pressure injuries noted Pain or pruritus (itching) present |
| Hair | Full distribution of hair on the head, axilla, and genitalia | Alopecia (hair loss), hirsutism (excessive hair growth over body), lice and/or nits, or lesions under hair |
| Nails | Smooth, well-shaped, and firm but flexible | Cracked, chipped, or splitting nail; excessively thick; presence of clubbing; ingrown nails |
| Skin Integrity | Skin intact with no wounds or pressure injuries. Braden Scale is 23 | A wound or pressure injury is present, or there is risk of developing a pressure injury with a Braden scale score of less than 23 |
Diagnostic and Lab Work
When a chronic wound is not healing as expected, laboratory test results can provide additional clues for the delayed healing. See Table 10.6d for a summary of lab results that offer clues to systemic issues causing delayed wound healing.
Table 10.6d Lab Values Associated with Delayed Wound Healing[94]
| Abnormal Lab Value | Rationale |
|---|---|
| Low hemoglobin | Low hemoglobin indicates less oxygen is transported to the wound site. |
| Elevated white blood cells (WBC) | Increased WBC indicates infection is occurring. |
| Low platelets | Platelets have an important role in the creation of granulation tissue. |
| Low albumin | Low albumin indicates decreased protein levels. Protein is required for effective wound healing. |
| Elevated blood glucose or hemoglobin A1C | Elevated blood glucose and hemoglobin A1C levels indicate poor management of diabetes mellitus, a disease that negatively impacts wound healing. |
| Elevated serum BUN and creatinine | BUN and creatinine levels are indicators of kidney function, with elevated levels indicating worsening kidney function. Elevated BUN (blood urea nitrogen) levels impact wound healing because it can indicate increased breakdown of the body's protein stores due to deficient protein in the diet. |
| Positive wound culture | Positive wound cultures indicate an infection is present and provide additional information including the type and number of bacteria present, as well as identifying antibiotics the bacteria is susceptible to. The nurse reviews this information when administering antibiotics to ensure the prescribed therapy is effective for the type of bacteria present. |
Life Span and Cultural Considerations
Newborns and Infants
Newborn skin is thin and sensitive. It tends to be easy to scratch and bruise and is susceptible to rashes and irritation. Common rashes seen in newborns and infants include diaper rash (contact dermatitis), cradle cap (seborrheic dermatitis), newborn acne, and prickly heat.
Toddlers and Preschoolers
Because of high levels of activity and increasing mobility, this age group is more prone to accidents. Issues like lacerations, abrasions, burns, and sunburns can occur frequently. It is important to be highly aware of the potential for accidents and implement safety precautions as needed.
School-Aged Children and Adolescents
Skin rashes tend to affect skin within this age group. Impetigo, scabies, and head lice are commonly seen and may keep children home from school. Acne vulgaris typically begins during adolescence and can alter physical appearance, which can be very upsetting to this age group. Another change during adolescence is the appearance of axillary, pubic, and other body hair. Also, as these children spend more time out of doors, sunburns are more common, and care should be given to encourage sunscreen and discourage the use of tanning beds.
Adults and Older Adults
As skin ages, many changes take place. Because aging increases the loss of subcutaneous fat and collagen breakdown, skin becomes thinner and wrinkles deepen. Decreased sweat gland activity leads to drier skin and pruritus (itching). Wound healing is slowed because of reduced circulation and the inability of proteins and proper nutrients to arrive at injury sites. Hair loses pigmentation and turns gray or white. Nails become thicker and are more difficult to cut. Age or liver spots become darker and more noticeable. The number of skin growths increases and includes skin tags and keratoses.
Diagnoses
There are several NANDA-I nursing diagnoses related to clients experiencing skin alterations or those at risk of developing a skin injury. See Table 10.6e for common NANDA-I nursing diagnoses and their definitions.[95]
Table 10.6e Common NANDA-I Nursing Diagnoses Related to Integumentary Disorders[96]
| Risk for Pressure Injury: “Susceptible to localized injury to the skin and/or underlying tissue usually over a bony prominence as a result of pressure, or pressure in combination with shear.” |
| Impaired Skin Integrity: “Altered epidermis and/or dermis.” |
| Risk for Impaired Skin Integrity: “Susceptible to alteration in epidermis and/or dermis, which may compromise health.” |
| Impaired Tissue Integrity: “Damage to the mucous membrane, cornea, integumentary system, muscular fascia, muscle, tendon, bone, cartilage, joint capsule, and/or ligament.” |
| Risk for Impaired Tissue Integrity: “Susceptible to damage to the mucous membrane, cornea, integumentary system, muscular fascia, muscle, tendon, bone, cartilage, joint capsule, and/or ligament, which may compromise health.” |
A commonly used NANDA-I nursing diagnosis for clients experiencing alterations in the integumentary system is Impaired Tissue Integrity, defined as, “Damage to the mucous membrane, cornea, integumentary system, muscular fascia, muscle, tendon, bone, cartilage, joint capsule, and/or ligament.”
To verify accuracy of this diagnosis for a client, the nurse compares assessment findings with defining characteristics of that diagnosis. Defining characteristics for Impaired Tissue Integrity include the following:
- Acute pain
- Bleeding
- Destroyed tissue
- Hematoma
- Localized area hot to touch
- Redness
- Tissue damage
A sample NANDA-I diagnosis in current PES format would be: “Impaired Tissue Integrity related to insufficient knowledge about protecting tissue integrity as evidenced by redness and tissue damage.”
Outcome Identification
An example of a broad goal for a client experiencing alterations in tissue integrity is:
- The client will experience tissue healing.
A sample SMART expected outcome for a client with a wound is:
- The client’s wound will decrease in size and have increased granulation tissue within two weeks.
Planning Interventions
In addition to the interventions outlined under the “Braden Scale” section to prevent and treat pressure injury, see the following box for a list of interventions to prevent and treat impaired skin integrity. As always, consult a current, evidence-based nurse care planning resource for additional interventions when planning client care.
Selected Interventions to Prevent and Treat Impaired Skin Integrity [97],[98],[99]
- Assess and document the client’s skin status routinely. (Frequency is determined based on the client’s status.)
- Use the Braden Scale to identify clients at risk for skin breakdown. Customize interventions to prevent and treat skin breakdown according to client needs.
- If a wound is present, evaluate the healing process at every dressing change. Note and document characteristics of the wound, including size, appearance, staging (if applicable), and drainage. Notify the provider of new signs of infection or lack of progress in healing.
- Provide wound care treatments, as prescribed by the provider or wound care specialist, and monitor the client's response toward expected outcomes.
- Cleanse the wound per facility protocol or as ordered.
- Maintain non-touch or aseptic technique when performing wound dressing changes, as indicated. (Read more details about using aseptic technique and the non-touch method in the "Aseptic Technique" chapter of the Open RN Nursing Skills,2e textbook.)
- Change wound dressings as needed to keep them clean and dry and prevent bacterial reservoir.
- Monitor for signs of infection in an existing wound (as indicated by redness, warmth, edema, increased pain, reddened appearance of surrounding skin, fever, increased white blood cell count, changes in wound drainage, or sudden change in client’s level of consciousness).
- Apply lotion to dry areas to prevent cracking.
- Apply lubricant to moisten lips and oral mucosa, as needed.
- Keep skin free of excess moisture. Use moisture barrier ointments (protective skin barriers) or incontinence products in skin areas subject to increased moisture and risk of skin breakdown.
- Educate the client and/or family caregivers on caring for the wound and request return demonstrations, as appropriate.
- Administer medications, as prescribed, and monitor for expected effects.
- Consult with a wound specialist, as needed.
- Obtain specimens of wound drainage for wound culture, as indicated, and monitor results.
- Advocate for pressure-relieving devices in clients at risk for pressure injuries, such as elbow protectors, heel protectors, chair cushions, and specialized mattresses and monitor the client's response.
- Promote adequate nutrition and hydration intake, unless contraindicated.
- Use a minimum of two-person assistance and a draw sheet to pull a client up in bed to minimize shear and friction.
- Reposition the client frequently to prevent skin breakdown and to promote healing. Turn the immobilized client at least every two hours, according to a specific schedule.
- Maintain a client’s position at 30 degrees or less, as appropriate, to prevent shear.
- Keep bed linens clean, dry, and wrinkle free.
Implementation
Before implementing interventions, it is important to assess the current status of the skin and risk factors present for skin breakdown and modify interventions based on the client’s current status. For example, if a client's rash has resolved, some interventions may no longer be appropriate (such as applying topical creams). However, if a wound is showing signs of worsening or delayed healing, additional interventions may be required. As always, if the client demonstrates new signs of localized or systemic infection, the provider should be notified.
Evaluation
It is important to evaluate for healing when performing wound care. Use the following expected outcomes when evaluating wound healing:
- Resolution of periwound redness in 1 week
- 50% reduction in wound dimensions in 2 weeks
- Reduction in volume of exudate
- 25% reduction in amount of necrotic tissue/eschar in 1 week
- Decreased pain intensity during dressing changes[100]
If a client is experiencing delayed wound healing or has a chronic wound, it is helpful to advocate for a referral to a wound care nurse specialist.
Read a sample nursing care plan for a client with impaired skin integrity.
Review the following example of applying the nursing process to a client with a pressure injury.
Client Scenario

Ms. Betty Pruitt is a 92-year-old female admitted to a skilled nursing facility after a fall at her daughter’s home while transferring the client from her bed to a wheelchair. See Figure 10.24 for an image of Ms. Pruitt.[101] Although no injury was sustained, it became clear to the family that they could no longer provide adequate care at home.
Ms. Pruitt’s past medical history includes congestive heart failure, hypertension, hypercholesterolemia, and moderate stage Alzheimer's disease. Her cognitive ability has significantly declined over the last six months. Her speech continues to be mostly clear and at times coherent, but she tends to be quiet and does not express her needs adequately, even with prompting. She no longer has the ability to ambulate but can stand for short periods of time, requiring two people to transfer. She rarely changes body position without encouragement and assistance, spending most of her days in a recliner or bed. Ms. Pruitt is 69 inches tall and currently weighs 122 pounds, having lost 22 pounds over the last three months. BMI is 18. Her family reports her appetite is poor, and she eats only in small amounts at mealtimes with feeding assistance. She does take liquids well and shows no swallowing difficulties at this time. Ms. Pruitt is incontinent of urine and stool most of the time but will use the toilet if offered and given transfer help. A skin assessment revealed a Stage III pressure injury on her coccyx area that is unknown to the family. The wound measures 4 cm long, 4 cm wide, and 3 cm deep, with adipose tissue visible but no undermining or tunneling visible. There is a scant amount of yellowish purulent drainage noted with a slight foul odor, redness, and increased heat around the wound present.
A Braden Scale Risk Assessment was completed and revealed a total score of 12 (High Risk) with the following category scores: Sensory Perception-3, Moisture-2, Activity-2, Mobility-2, Nutrition-2, Friction & Shear-1.
Applying the Nursing Process
Based on this information, the following nursing care plan was implemented for Ms. Pruitt.
Nursing Diagnosis: Impaired Tissue Integrity related to imbalanced nutritional state and associated with impaired mobility as evidenced by damaged tissue, redness, area hot to touch.
Overall Goal: The client will experience wound healing demonstrated by decreased wound size and increased granulation tissue.
SMART Expected Outcome: Ms. Pruitt will have a 50% reduction in wound dimensions (from 4 cm in diameter to 2 cm) within two weeks.
Planned Nursing Interventions With Rationale: See Table 10.7 for a list of planned nursing interventions with rationale.
Table 10.7 Selected Interventions and Rationale for Ms. Pruitt
| Interventions | Rationale |
|---|---|
| 1. Assess and document wound characteristics every shift, including size (length x width x depth), stage (I-IV), location, exudate, presence of granulation tissue, and epithelization. | Consistent and accurate documentation of wounds is important in determining the progression of wound healing and effectiveness of treatments. |
| 2. Monitor for signs of infection (color, temperature, edema, moisture, pain, and appearance of surrounding skin). | Frequent monitoring for possible wound infection provides the ability to intervene quickly if changes in the wound are noted. |
| 3. Offer PRN pain medications prior to dressing changes if pain is present. | Dressing changes may be painful for clients. PRN pain medications should be offered in advance of the procedure for effective pain management. |
| 4. Cleanse wound and periwound area (skin around the wound) per facility protocol or as ordered. | Removal of exudate, dirt, and slough promotes wound healing. Decreasing the number of microorganisms around the wound may decrease the chance of wound infection. |
| 5. Apply and change wound dressings, per facility protocol or wound orders. | Dressings that maintain moisture in the wound keep periwound skin dry, absorb drainage, and pad the wound to protect from further injury assist in healing. |
| 6. Turn/reposition the client every two hours and position with pillows as needed. | Frequent repositioning relieves pressure point areas from damage. Avoid positioning the client directly on an injured area if possible. |
| 7. Consider the use of a specialty mattress, bed, or chair pad. | Specialty mattresses, beds, or pads offer added padding and support, while decreasing pressure areas. |
| 8. Use moisture barrier ointments (protective skin barriers). | Moisture barrier ointments can significantly decrease skin breakdown and pressure injury formation. |
| 9. Check incontinence pads frequently (every two to three hours) and change as needed to keep dry. | Frequent changing of soiled pads will prevent exposure to chemicals in urine and stool that erode the skin. |
| 10. Monitor nutritional status and obtain order for dietary consult if needed. | Optimizing nutritional intake, including calories, protein, and vitamins, is essential to promote wound healing. |
| 11. Offer nutritional supplements and water. | Nutritional supplements, such as protein shakes, can provide additional calories and protein without a large volume of intake needed. Water intake is essential for proper tissue hydration. |
| 12. Keep bed linens clean, dry, and wrinkle free. | Soiled, wet, or wrinkled sheets may contribute to skin breakdown. |
| 13. Use a minimum of two-person assistance and a draw sheet to pull the client up in bed. | Carefully transferring clients avoids adverse effects of external mechanical forces (pressure, friction, and shear) from causing skin or tissue damage. |
Interventions Implemented:
After the admission assessment was completed, Ms. Pruitt became settled in her new room. The wound was assessed, documented, and cleansed. A specimen for wound culture was obtained and a wound dressing applied per protocol. The health care provider was notified of the wound. Requests were made for a wound culture, referrals to a wound care nurse specialist and a dietician, and a pressure-relieving mattress for the bed. A two-hour turning schedule was implemented, and the CNA was reminded to use two-person assistance with a lift sheet when repositioning the client. A barrier cream was applied to protect the peri-area whenever a new incontinence pad was placed. The following documentation note was entered in the client chart.
Sample Documentation:
7/1/2024 1030: On admission, a Stage III pressure injury was discovered on the client’s coccyx area. The wound measured 4 cm long, 4 cm wide, 3 cm deep, with adipose tissue visible. No undermining, tunneling, bone, muscle, or tendons visible. A small amount of yellow purulent drainage noted. Slight foul odor, with redness, and increased heat around the wound present. Wound was cleansed with normal saline and packed with moist gauze and covered with hydrogel dressing. Client tolerated the procedure well and gave no evidence of pain. A pressure-relieving mattress was placed on the client’s bed and a two-hour turning schedule was implemented. Client voided x 1 and the pad was changed. Barrier cream was applied to the perineal area. Client encouraged to rest until lunchtime and is resting comfortably at this time. -S. Jones, RN
Evaluation:
After two weeks, the measurements of the wound were compared to those on admission and the wound decreased in size to less than 2 cm. The expected outcome was "met." A new expected outcome was established, "Ms. Pruitt's wound will resolve within the next 2 weeks." The same planned interventions were continued to be implemented.
Review the following example of applying the nursing process to a client with a pressure injury.
Client Scenario

Ms. Betty Pruitt is a 92-year-old female admitted to a skilled nursing facility after a fall at her daughter’s home while transferring the client from her bed to a wheelchair. See Figure 10.24 for an image of Ms. Pruitt.[102] Although no injury was sustained, it became clear to the family that they could no longer provide adequate care at home.
Ms. Pruitt’s past medical history includes congestive heart failure, hypertension, hypercholesterolemia, and moderate stage Alzheimer's disease. Her cognitive ability has significantly declined over the last six months. Her speech continues to be mostly clear and at times coherent, but she tends to be quiet and does not express her needs adequately, even with prompting. She no longer has the ability to ambulate but can stand for short periods of time, requiring two people to transfer. She rarely changes body position without encouragement and assistance, spending most of her days in a recliner or bed. Ms. Pruitt is 69 inches tall and currently weighs 122 pounds, having lost 22 pounds over the last three months. BMI is 18. Her family reports her appetite is poor, and she eats only in small amounts at mealtimes with feeding assistance. She does take liquids well and shows no swallowing difficulties at this time. Ms. Pruitt is incontinent of urine and stool most of the time but will use the toilet if offered and given transfer help. A skin assessment revealed a Stage III pressure injury on her coccyx area that is unknown to the family. The wound measures 4 cm long, 4 cm wide, and 3 cm deep, with adipose tissue visible but no undermining or tunneling visible. There is a scant amount of yellowish purulent drainage noted with a slight foul odor, redness, and increased heat around the wound present.
A Braden Scale Risk Assessment was completed and revealed a total score of 12 (High Risk) with the following category scores: Sensory Perception-3, Moisture-2, Activity-2, Mobility-2, Nutrition-2, Friction & Shear-1.
Applying the Nursing Process
Based on this information, the following nursing care plan was implemented for Ms. Pruitt.
Nursing Diagnosis: Impaired Tissue Integrity related to imbalanced nutritional state and associated with impaired mobility as evidenced by damaged tissue, redness, area hot to touch.
Overall Goal: The client will experience wound healing demonstrated by decreased wound size and increased granulation tissue.
SMART Expected Outcome: Ms. Pruitt will have a 50% reduction in wound dimensions (from 4 cm in diameter to 2 cm) within two weeks.
Planned Nursing Interventions With Rationale: See Table 10.7 for a list of planned nursing interventions with rationale.
Table 10.7 Selected Interventions and Rationale for Ms. Pruitt
| Interventions | Rationale |
|---|---|
| 1. Assess and document wound characteristics every shift, including size (length x width x depth), stage (I-IV), location, exudate, presence of granulation tissue, and epithelization. | Consistent and accurate documentation of wounds is important in determining the progression of wound healing and effectiveness of treatments. |
| 2. Monitor for signs of infection (color, temperature, edema, moisture, pain, and appearance of surrounding skin). | Frequent monitoring for possible wound infection provides the ability to intervene quickly if changes in the wound are noted. |
| 3. Offer PRN pain medications prior to dressing changes if pain is present. | Dressing changes may be painful for clients. PRN pain medications should be offered in advance of the procedure for effective pain management. |
| 4. Cleanse wound and periwound area (skin around the wound) per facility protocol or as ordered. | Removal of exudate, dirt, and slough promotes wound healing. Decreasing the number of microorganisms around the wound may decrease the chance of wound infection. |
| 5. Apply and change wound dressings, per facility protocol or wound orders. | Dressings that maintain moisture in the wound keep periwound skin dry, absorb drainage, and pad the wound to protect from further injury assist in healing. |
| 6. Turn/reposition the client every two hours and position with pillows as needed. | Frequent repositioning relieves pressure point areas from damage. Avoid positioning the client directly on an injured area if possible. |
| 7. Consider the use of a specialty mattress, bed, or chair pad. | Specialty mattresses, beds, or pads offer added padding and support, while decreasing pressure areas. |
| 8. Use moisture barrier ointments (protective skin barriers). | Moisture barrier ointments can significantly decrease skin breakdown and pressure injury formation. |
| 9. Check incontinence pads frequently (every two to three hours) and change as needed to keep dry. | Frequent changing of soiled pads will prevent exposure to chemicals in urine and stool that erode the skin. |
| 10. Monitor nutritional status and obtain order for dietary consult if needed. | Optimizing nutritional intake, including calories, protein, and vitamins, is essential to promote wound healing. |
| 11. Offer nutritional supplements and water. | Nutritional supplements, such as protein shakes, can provide additional calories and protein without a large volume of intake needed. Water intake is essential for proper tissue hydration. |
| 12. Keep bed linens clean, dry, and wrinkle free. | Soiled, wet, or wrinkled sheets may contribute to skin breakdown. |
| 13. Use a minimum of two-person assistance and a draw sheet to pull the client up in bed. | Carefully transferring clients avoids adverse effects of external mechanical forces (pressure, friction, and shear) from causing skin or tissue damage. |
Interventions Implemented:
After the admission assessment was completed, Ms. Pruitt became settled in her new room. The wound was assessed, documented, and cleansed. A specimen for wound culture was obtained and a wound dressing applied per protocol. The health care provider was notified of the wound. Requests were made for a wound culture, referrals to a wound care nurse specialist and a dietician, and a pressure-relieving mattress for the bed. A two-hour turning schedule was implemented, and the CNA was reminded to use two-person assistance with a lift sheet when repositioning the client. A barrier cream was applied to protect the peri-area whenever a new incontinence pad was placed. The following documentation note was entered in the client chart.
Sample Documentation:
7/1/2024 1030: On admission, a Stage III pressure injury was discovered on the client’s coccyx area. The wound measured 4 cm long, 4 cm wide, 3 cm deep, with adipose tissue visible. No undermining, tunneling, bone, muscle, or tendons visible. A small amount of yellow purulent drainage noted. Slight foul odor, with redness, and increased heat around the wound present. Wound was cleansed with normal saline and packed with moist gauze and covered with hydrogel dressing. Client tolerated the procedure well and gave no evidence of pain. A pressure-relieving mattress was placed on the client’s bed and a two-hour turning schedule was implemented. Client voided x 1 and the pad was changed. Barrier cream was applied to the perineal area. Client encouraged to rest until lunchtime and is resting comfortably at this time. -S. Jones, RN
Evaluation:
After two weeks, the measurements of the wound were compared to those on admission and the wound decreased in size to less than 2 cm. The expected outcome was "met." A new expected outcome was established, "Ms. Pruitt's wound will resolve within the next 2 weeks." The same planned interventions were continued to be implemented.
Learning Activities
(Answers to "Learning Activities" can be found in the "Answer Key" at the end of the book. Answers to interactive activity elements will be provided within the element as immediate feedback.)
You are a nurse working in a long-term care facility. You have been assigned to care for Mr. Johns, a 74-year-old client recently diagnosed with a urinary tract infection, resulting in frequent incontinence. Mr. Johns suffered a cerebrovascular accident (stroke) six months ago and has difficulties ambulating and attending to his own needs because of weakness on his right side. Mr. Johns is alert and oriented to person, place, and time, but has decreased sensation on his entire right side. He spends most of his time in bed or sitting at his bedside in a wheelchair due to his difficulty with ambulation. He eats about 50% of his meals. While assessing Mr. Johns, you note that he is thin for his height, incontinent of foul-smelling urine, and has a red area of skin on his sacrum.
- What additional information, including lab work, would you like to gather to further assess Mr. Johns' potential for pressure injury development?
- What factors make him particularly vulnerable to the development of pressure injuries?

Test your knowledge using this NCLEX Next Generation-style bowtie question. You may reset and resubmit your answers to this question an unlimited number of times.[103]
Learning Activities
(Answers to "Learning Activities" can be found in the "Answer Key" at the end of the book. Answers to interactive activity elements will be provided within the element as immediate feedback.)
You are a nurse working in a long-term care facility. You have been assigned to care for Mr. Johns, a 74-year-old client recently diagnosed with a urinary tract infection, resulting in frequent incontinence. Mr. Johns suffered a cerebrovascular accident (stroke) six months ago and has difficulties ambulating and attending to his own needs because of weakness on his right side. Mr. Johns is alert and oriented to person, place, and time, but has decreased sensation on his entire right side. He spends most of his time in bed or sitting at his bedside in a wheelchair due to his difficulty with ambulation. He eats about 50% of his meals. While assessing Mr. Johns, you note that he is thin for his height, incontinent of foul-smelling urine, and has a red area of skin on his sacrum.
- What additional information, including lab work, would you like to gather to further assess Mr. Johns' potential for pressure injury development?
- What factors make him particularly vulnerable to the development of pressure injuries?

Test your knowledge using this NCLEX Next Generation-style bowtie question. You may reset and resubmit your answers to this question an unlimited number of times.[104]
Angiogenesis: The process of wound healing when new capillaries begin to develop within the wound 24 hours after injury to bring in more oxygen and nutrients for healing. (Chapter 10.3)
Approximated edges: The well-closed edges of a wound healing by primary intention. (Chapter 10.3)
Arterial insufficiency: A condition caused by lack of adequately oxygenated blood supply to specific tissues. (Chapter 10.2)
Braden Scale: A standardized assessment tool used to assess and document a client’s risk factors for developing pressure injuries. (Chapter 10.5)
Deep tissue pressure injuries: Persistent; non-blanchable; deep red, maroon, or purple discoloration of intact or nonintact skin revealing a dark wound bed or blood-filled blister. Pain and temperature change often precede skin color changes. Discoloration may appear differently in darkly pigmented skin. (Chapter 10.4)
Dehiscence: The separation of a surgical incision. (Chapter 10.2)
Dermis: The layer of skin underneath under the epidermis, containing hair follicles, sebaceous glands, blood vessels, endocrine sweat glands, and nerve endings. (Chapter 10.2)
Edema: Swelling. (Chapter 10.3)
Epidermis: The very thin, top layer of the skin that contains openings of the sweat gland ducts and the visible part of hair known as the hair shaft. (Chapter 10.2)
Epithelialization: The development of new epidermis and granulation tissue in a healing wound. (Chapter 10.3)
Erythema: Redness. (Chapter 10.3)
Eschar: Dark brown/black, dry, thick, and leathery dead tissue in wounds. (Chapter 10.4)
Excoriation: Redness and removal of the surface of the topmost layer of skin, often due to maceration or itching. (Chapter 10.2)
Exudate: Fluid that oozes from a wound. (Chapter 10.3)
Friction: The rubbing of skin against a hard object, such as the bed or the arm of a wheelchair. This rubbing causes heat that can remove the top layer of skin and often results in skin damage. (Chapter 10.4)
Granulation tissue: New connective tissue in a healing wound with new, fragile, thin-walled capillaries. (Chapter 10.3)
Hemostasis phase of wound healing: The first stage of wound healing when clotting factors are released to form clots to stop the bleeding. (Chapter 10.3)
Hypodermis: The bottom layer of skin, also referred to as the subcutaneous layer, consisting mainly of adipose tissue or fat, along with some blood vessels and nerve endings. Beneath this layer lies muscles, tendons, ligaments, and bones. (Chapter 10.2)
Impaired skin integrity: Altered epidermis and/or dermis. (Chapter 10.2)
Impaired tissue integrity: Damage to deeper layers of the skin or other integumentary structures. The NANDA-I definition of impaired tissue integrity is, “Damage to the mucous membrane, cornea, integumentary system, muscular fascia, muscle, tendon, bone, cartilage, joint capsule, and/or ligament.” (Chapter 10.2)
Inflammatory phase of wound healing: The second stage of healing when vasodilation occurs to move white blood cells into the wound to start cleaning the wound bed. (Chapter 10.3)
Maceration: A condition that occurs when skin has been exposed to moisture for too long causing it to appear soggy, wrinkled, or whiter than usual. (Chapter 10.2)
Maturation phase of wound healing: The final stage of wound healing when collagen continues to be created to strengthen the wound and prevent it from reopening. (Chapter 10.3)
Necrosis: Tissue death. (Chapter 10.2)
Necrotic: Dead tissue that is black. (Chapter 10.2)
Nonblanchable erythema: Skin redness that does not turn white when pressed. (Chapter 10.4)
Pressure injuries: Localized damage to the skin or underlying soft tissue, usually over a bony prominence, as a result of intense and prolonged pressure in combination with shear. (Chapter 10.4)
Primary intention: A type of wound that is sutured, stapled, glued, or otherwise closed so the wound heals beneath the closure. (Chapter 10.3)
Proliferative phase of wound healing: The third stage of wound healing that begins a few days after injury and includes four processes: epithelialization, angiogenesis, collagen formation, and contraction. (Chapter 10.3)
Purulent: Drainage that is thick; opaque; tan, yellow, green, or brown in color. New purulent drainage should always be reported to the health care provider. (Chapter 10.6)
Sanguineous: Drainage from a wound that is fresh bleeding. (Chapter 10.6)
Secondary intention: A type of healing that occurs when the edges of a wound cannot be brought together, so the wound fills in from the bottom up by the production of granulation tissue. An example of a wound healing by secondary intention is a pressure ulcer. (Chapter 10.3)
Serosanguineous: Serous drainage with small amounts of blood present. (Chapter 10.6)
Serous: Drainage from a wound that is clear, thin, watery plasma. It’s normal during the inflammatory stage of wound healing, and small amounts are considered normal wound drainage. (Chapter 10.6)
Shear: Damage that occurs when tissue layers move over the top of each other, causing blood vessels to stretch and break as they pass through the subcutaneous tissue. (Chapter 10.4)
Slough: Inflammatory exudate in wounds that is usually light yellow, soft, and moist. (Chapter 10.4)
Stage 1 pressure injuries: Intact skin with a localized area of nonblanchable erythema where prolonged pressure has occurred. (Chapter 10.4)
Stage 2 pressure injuries: Partial-thickness loss of skin with exposed dermis. The wound bed is viable and may appear like an intact or ruptured blister. (Chapter 10.4)
Stage 3 pressure injuries: Full-thickness tissue loss in which fat is visible, but cartilage, tendon, ligament, muscle, and bone are not exposed. The depth of tissue damage varies by anatomical location. Undermining and tunneling may be present. If slough or eschar obscures the wound so that tissue loss cannot be assessed, the pressure injury is referred to as unstageable. (Chapter 10.4)
Stage 4 pressure injuries: Full-thickness tissue loss like Stage 3 pressure injuries but also have exposed cartilage, tendon, ligament, muscle, or bone. (Chapter 10.4)
Tertiary intention: The healing of a wound that has had to remain open or has been reopened, often due to severe infection or swelling. (Chapter 10.3)
Tunneling: Passageways underneath the surface of the skin that extend from a wound and can take twists and turns. (Chapter 10.4)
Undermining: A condition that occurs in wounds when the tissue under the wound edges becomes eroded, resulting in a pocket beneath the skin at the wound's edge. (Chapter 10.4)
Unstageable pressure injuries: Full-thickness skin and tissue loss in which the extent of tissue damage within the ulcer cannot be confirmed because it is obscured by slough or eschar. (Chapter 10.4)
Venous insufficiency: A condition that occurs when the cardiovascular system cannot adequately return blood and fluid from the extremities to the heart. (Chapter 10.2)
Angiogenesis: The process of wound healing when new capillaries begin to develop within the wound 24 hours after injury to bring in more oxygen and nutrients for healing. (Chapter 10.3)
Approximated edges: The well-closed edges of a wound healing by primary intention. (Chapter 10.3)
Arterial insufficiency: A condition caused by lack of adequately oxygenated blood supply to specific tissues. (Chapter 10.2)
Braden Scale: A standardized assessment tool used to assess and document a client’s risk factors for developing pressure injuries. (Chapter 10.5)
Deep tissue pressure injuries: Persistent; non-blanchable; deep red, maroon, or purple discoloration of intact or nonintact skin revealing a dark wound bed or blood-filled blister. Pain and temperature change often precede skin color changes. Discoloration may appear differently in darkly pigmented skin. (Chapter 10.4)
Dehiscence: The separation of a surgical incision. (Chapter 10.2)
Dermis: The layer of skin underneath under the epidermis, containing hair follicles, sebaceous glands, blood vessels, endocrine sweat glands, and nerve endings. (Chapter 10.2)
Edema: Swelling. (Chapter 10.3)
Epidermis: The very thin, top layer of the skin that contains openings of the sweat gland ducts and the visible part of hair known as the hair shaft. (Chapter 10.2)
Epithelialization: The development of new epidermis and granulation tissue in a healing wound. (Chapter 10.3)
Erythema: Redness. (Chapter 10.3)
Eschar: Dark brown/black, dry, thick, and leathery dead tissue in wounds. (Chapter 10.4)
Excoriation: Redness and removal of the surface of the topmost layer of skin, often due to maceration or itching. (Chapter 10.2)
Exudate: Fluid that oozes from a wound. (Chapter 10.3)
Friction: The rubbing of skin against a hard object, such as the bed or the arm of a wheelchair. This rubbing causes heat that can remove the top layer of skin and often results in skin damage. (Chapter 10.4)
Granulation tissue: New connective tissue in a healing wound with new, fragile, thin-walled capillaries. (Chapter 10.3)
Hemostasis phase of wound healing: The first stage of wound healing when clotting factors are released to form clots to stop the bleeding. (Chapter 10.3)
Hypodermis: The bottom layer of skin, also referred to as the subcutaneous layer, consisting mainly of adipose tissue or fat, along with some blood vessels and nerve endings. Beneath this layer lies muscles, tendons, ligaments, and bones. (Chapter 10.2)
Impaired skin integrity: Altered epidermis and/or dermis. (Chapter 10.2)
Impaired tissue integrity: Damage to deeper layers of the skin or other integumentary structures. The NANDA-I definition of impaired tissue integrity is, “Damage to the mucous membrane, cornea, integumentary system, muscular fascia, muscle, tendon, bone, cartilage, joint capsule, and/or ligament.” (Chapter 10.2)
Inflammatory phase of wound healing: The second stage of healing when vasodilation occurs to move white blood cells into the wound to start cleaning the wound bed. (Chapter 10.3)
Maceration: A condition that occurs when skin has been exposed to moisture for too long causing it to appear soggy, wrinkled, or whiter than usual. (Chapter 10.2)
Maturation phase of wound healing: The final stage of wound healing when collagen continues to be created to strengthen the wound and prevent it from reopening. (Chapter 10.3)
Necrosis: Tissue death. (Chapter 10.2)
Necrotic: Dead tissue that is black. (Chapter 10.2)
Nonblanchable erythema: Skin redness that does not turn white when pressed. (Chapter 10.4)
Pressure injuries: Localized damage to the skin or underlying soft tissue, usually over a bony prominence, as a result of intense and prolonged pressure in combination with shear. (Chapter 10.4)
Primary intention: A type of wound that is sutured, stapled, glued, or otherwise closed so the wound heals beneath the closure. (Chapter 10.3)
Proliferative phase of wound healing: The third stage of wound healing that begins a few days after injury and includes four processes: epithelialization, angiogenesis, collagen formation, and contraction. (Chapter 10.3)
Purulent: Drainage that is thick; opaque; tan, yellow, green, or brown in color. New purulent drainage should always be reported to the health care provider. (Chapter 10.6)
Sanguineous: Drainage from a wound that is fresh bleeding. (Chapter 10.6)
Secondary intention: A type of healing that occurs when the edges of a wound cannot be brought together, so the wound fills in from the bottom up by the production of granulation tissue. An example of a wound healing by secondary intention is a pressure ulcer. (Chapter 10.3)
Serosanguineous: Serous drainage with small amounts of blood present. (Chapter 10.6)
Serous: Drainage from a wound that is clear, thin, watery plasma. It’s normal during the inflammatory stage of wound healing, and small amounts are considered normal wound drainage. (Chapter 10.6)
Shear: Damage that occurs when tissue layers move over the top of each other, causing blood vessels to stretch and break as they pass through the subcutaneous tissue. (Chapter 10.4)
Slough: Inflammatory exudate in wounds that is usually light yellow, soft, and moist. (Chapter 10.4)
Stage 1 pressure injuries: Intact skin with a localized area of nonblanchable erythema where prolonged pressure has occurred. (Chapter 10.4)
Stage 2 pressure injuries: Partial-thickness loss of skin with exposed dermis. The wound bed is viable and may appear like an intact or ruptured blister. (Chapter 10.4)
Stage 3 pressure injuries: Full-thickness tissue loss in which fat is visible, but cartilage, tendon, ligament, muscle, and bone are not exposed. The depth of tissue damage varies by anatomical location. Undermining and tunneling may be present. If slough or eschar obscures the wound so that tissue loss cannot be assessed, the pressure injury is referred to as unstageable. (Chapter 10.4)
Stage 4 pressure injuries: Full-thickness tissue loss like Stage 3 pressure injuries but also have exposed cartilage, tendon, ligament, muscle, or bone. (Chapter 10.4)
Tertiary intention: The healing of a wound that has had to remain open or has been reopened, often due to severe infection or swelling. (Chapter 10.3)
Tunneling: Passageways underneath the surface of the skin that extend from a wound and can take twists and turns. (Chapter 10.4)
Undermining: A condition that occurs in wounds when the tissue under the wound edges becomes eroded, resulting in a pocket beneath the skin at the wound's edge. (Chapter 10.4)
Unstageable pressure injuries: Full-thickness skin and tissue loss in which the extent of tissue damage within the ulcer cannot be confirmed because it is obscured by slough or eschar. (Chapter 10.4)
Venous insufficiency: A condition that occurs when the cardiovascular system cannot adequately return blood and fluid from the extremities to the heart. (Chapter 10.2)

