Open Resources for Nursing (Open RN)
What Causes Sleep?
There are two internal biological mechanisms that work together to regulate wakefulness and sleep referred to as circadian rhythms and sleep-wake homeostasis.
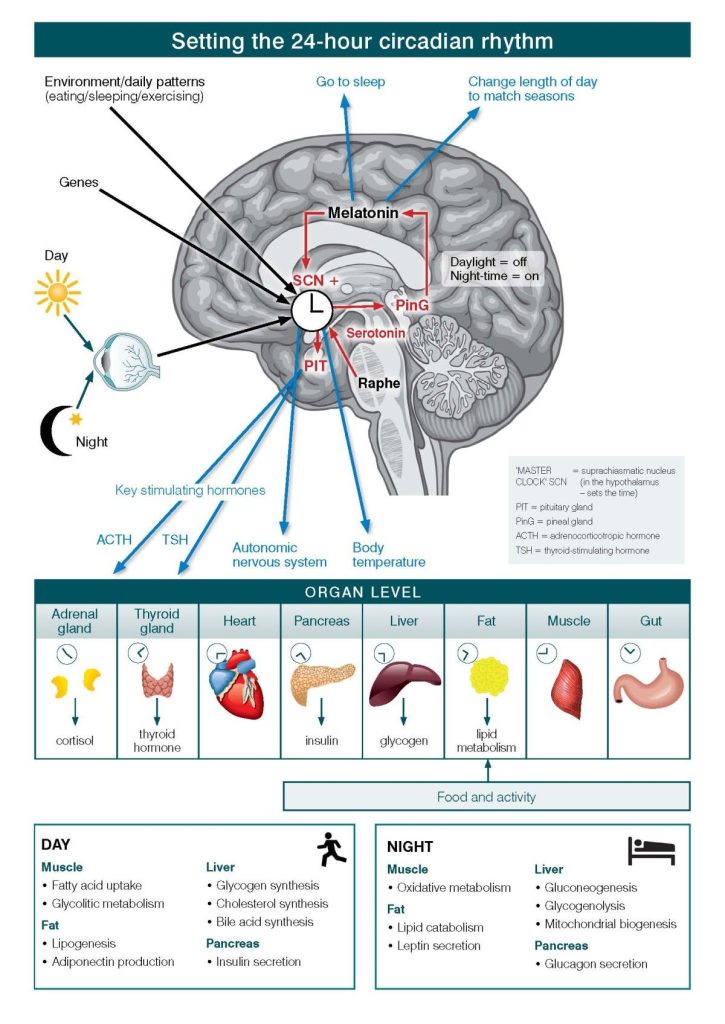
Circadian rhythms direct a wide variety of body functions, including wakefulness, core temperature, metabolism, and the release of hormones. They control the timing of sleep, causing a person to feel sleepy at night and creating a tendency to wake in the morning without an alarm. See Figure 12.1[1] for an illustration of circadian rhythms. Circadian rhythms are based roughly on a 24-hour clock and use environmental cues, such as light and temperature to determine the time of day.[2]
Sleep-wake homeostasis keeps track of a person’s need for sleep. A pressure to sleep builds with every hour that a person is awake, reaching a peak in the evening when most people fall asleep. The homeostatic sleep drive also regulates sleep intensity, causing a person to sleep longer and more deeply after a period of sleep deprivation.[3] Adenosine is linked to this drive for sleep. While awake, the level of adenosine in the brain continues to rise, with increased levels signaling a shift toward sleep. While sleeping, the body breaks down adenosine. When it gets dark, the body also releases a hormone called melatonin. Melatonin signals the body that it’s time to prepare for sleep and creates a feeling of drowsiness. The amount of melatonin in the bloodstream peaks as the evening wears on. A third hormone, cortisol, is released in the early morning hours and naturally prepares the body to wake up.[4]
Factors that influence a person’s sleep and wakefulness include medical conditions, medications, stress, sleep environment, and foods and fluids consumed, but the greatest influence is exposure to light. Specialized cells in the retina process light and provide messages to the brain to align the body clock with periods of day or night. Exposure to bright artificial light in the late evening can disrupt this process, making it hard to fall asleep. Examples of bright artificial light include the light from a TV screen, computer, or smartphone. Exposure to light can also make it difficult to return to sleep after being awakened.[5]
Night shift workers often have trouble falling asleep when they go to bed and may have trouble staying awake at work because their natural circadian rhythm and sleep-wake cycle are disrupted. Jet lag also disrupts circadian rhythms. When flying to a different time zone, a mismatch is created between a person’s internal clock and the actual time of day.[6]
The rhythm and timing of the body clock change with age. For example, teenagers fall asleep later at night than younger children and adults because melatonin is released and peaks later in the 24-hour cycle for teens. As a result, it’s natural for many teens to prefer later bedtimes at night and sleep later in the morning than adults.[7]
Individuals also need more sleep early in life, when they’re growing and developing. For example, newborns may sleep more than 16 hours a day, and preschool-aged children need to take naps. Young children tend to sleep more in the early evening whereas older adults tend to go to bed earlier and wake up earlier.[8]
Sleep Phases and Stages
When sleeping, individuals cycle through two phases of sleep: rapid eye movement (REM) and non-REM sleep. A full sleep cycle takes 80 to 100 minutes to complete, and most people typically cycle through four to six cycles per night. It is common to wake up briefly between cycles.[9]
Restoration takes place mostly during slow-wave non-REM sleep, during which the body’s temperature, heart rate, and brain oxygen consumption decrease. Brain activity decreases, so this stage is also referred to as slow-wave sleep and is observed during sleep studies. Non-REM sleep has these three stages:
- Stage 1: The transition between wakefulness and sleep.
- Stage 2: The initiation of the sleep phase.
- Stage 3: The deep sleep or slow-wave sleep stage based on a pattern that appears during measurements of brain activity. Individuals spend the most amount of sleep time in this stage during the early part of the night. (Note that the previously considered fourth stage of non-REM sleep is now included within Stage 3).[10]
During REM sleep, a person’s heart rate and respiratory rate increase. Eyes twitch as they rapidly move back and forth and the brain is active. Brain activity measured during REM sleep is similar to activity during waking hours. Dreaming occurs during REM sleep, and muscles normally become limp to prevent acting out one’s dreams. People typically experience more REM sleep as the night progresses. However, hot and cold environments can affect a person’s REM sleep because the body does not regulate temperature well during REM sleep.[11] See Figure 12.2[12] for an image illustrating stages of sleep with increased REM sleep through the night indicated in solid red lines.
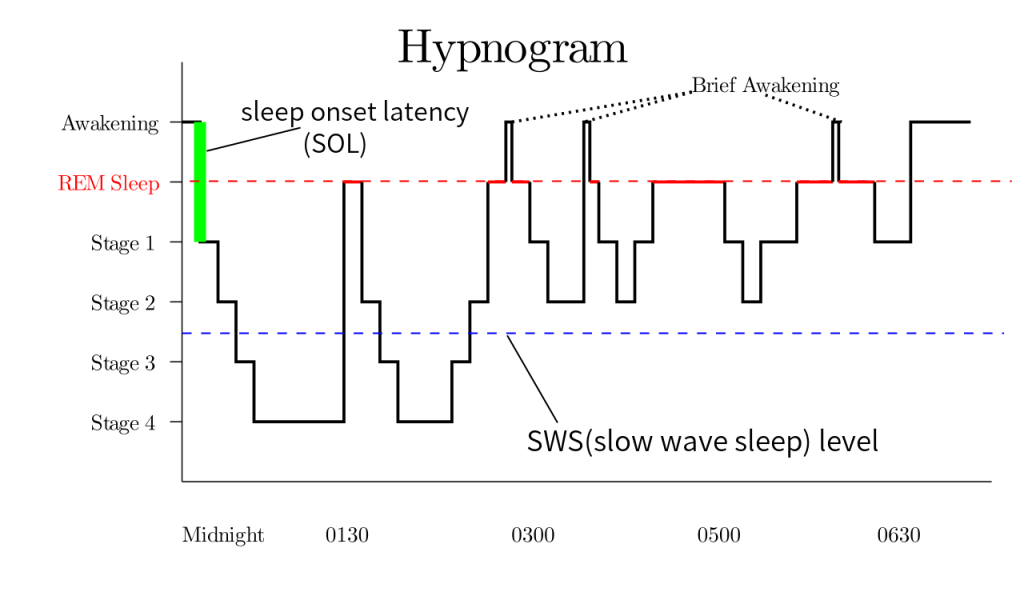
The patterns and types of sleep change as people mature. For example, newborns spend more time in REM sleep. The amount of slow-wave sleep peaks in early childhood and then drops sharply in the teenage years. Slow-wave sleep continues to decrease through adulthood, and older people may not have any slow-wave sleep at all.[13]
Why Is Sleep Important?
Sleep plays a vital role in good health and well-being. Getting enough quality sleep at the right times protects mental health and physical health. Lack of sleep affects daytime performance, quality of life, and safety. The way a person feels while awake depends on what happens while they are sleeping. During sleep, the body is working to support healthy brain function and maintain physical health. In children and teens, sleep also helps support growth and development.[14]
Healthy Brain Function and Emotional Well-Being
Sleep helps the brain work properly. While sleeping, the brain is forming new pathways to help a person learn and remember information. Studies show that a good night’s sleep improves learning and problem-solving skills. Sleep also helps a person pay attention, make decisions, and be creative. Conversely, sleep deficiency alters activity in some parts of the brain, causing difficulty in making decisions, solving problems, controlling emotions and behavior, and coping with change. Sleep deficiency has also been linked to depression, suicide, and risk-taking behavior.[15]
Physical Health
Sleep also plays an important role in physical health. For example, sleep is involved in healing and repairing the heart and blood vessels. Ongoing sleep deficiency is linked to an increased risk of heart disease, kidney disease, high blood pressure, diabetes, and stroke. Sleep helps maintain a healthy balance of the hormones that cause hunger (ghrelin) or a feeling of fullness (leptin). When a person doesn’t get enough sleep, the level of ghrelin increases and the level of leptin decreases, causing a person to feel hungry when sleep deprived. The way the body responds to insulin is also affected, causing increased blood sugar.[16]
Sleep supports healthy growth and development. Deep sleep triggers the body to release hormones that promote normal growth in children and teens. See Figure 12.3.[17] of a sleeping child. These hormones also boost muscle mass and help repair cells and tissues.[18]

Daytime Performance
Getting enough quality sleep at the right times also enhances functioning throughout the day. People who are sleep deficient are less productive at work and school. They take longer to finish tasks, have a slower reaction time, and make more mistakes. After several nights of losing sleep, even a loss of just one or two hours per night, the ability to function declines.[19] See Figure 12.4[20] for an image of a student demonstrating sleep deficiency while studying.
Lack of sleep can lead to microsleep. Microsleep refers to brief moments of sleep that occur when one is normally awake. You can’t control microsleep, and you might not be aware of it. For example, have you ever driven somewhere and then not remembered part of the trip? If so, you may have experienced microsleep. Even if you’re not driving, microsleep can affect how you function. If you’re listening to a lecture, for example, you might miss some of the information or feel as if you don’t understand the point. In reality, you may have slept through part of the lecture and not been aware of experiencing microsleep.[21]
Effects of Sleep Deficiency
The damage from sleep deficiency can occur in an instant. For example, drowsy drivers may feel capable of driving. Yet, studies show that sleep deficiency harms one’s driving ability as much as, or more than, being drunk. It is estimated that driver sleepiness is a factor in about 100,000 car accidents each year, resulting in about 1,500 deaths.[22]
Drivers aren’t the only ones affected by sleep deficiency. It can affect people in all lines of work, including health care workers, pilots, students, mechanics, and assembly line workers. As a result, sleep deficiency is harmful not only on a personal level, but also can cause large-scale damage. For example, sleep deficiency has played a role in human errors linked to tragic accidents, such as nuclear reactor meltdowns, grounding of large ships, and aviation accidents.[23]
Sleep deficiency can also cause long-term harm. It increases the risk of obesity. For example, one study of teenagers showed that with each hour of sleep lost, the odds of becoming obese went up. Sleep deficiency increases the risk of obesity in other age groups as well. Sleep also affects how your body reacts to insulin, the hormone that controls your blood glucose (sugar) level. Sleep deficiency results in a higher than normal blood sugar level, which may increase your risk for diabetes.[24] Ongoing sleep deficiency can also change the way in which your immune system responds. For example, if you’re sleep deficient, you may have trouble fighting common infections.[25] In addition, children and teens who are sleep deficient may have problems getting along with others. They may feel angry and impulsive, have mood swings, feel sad or depressed, or lack motivation. They also may have problems paying attention, and they may get lower grades and feel stressed.[26]
If a person routinely loses sleep or chooses to sleep less than needed, the sleep loss adds up. The total sleep lost is called sleep debt. For example, if you lose 2 hours of sleep each night, you’ll have a sleep debt of 14 hours after a week.[27] See Figure 12.5[28] of an individual feeling the effects of sleep debt on awakening.

Some people nap as a way to deal with sleepiness. Naps can provide a short-term boost in alertness and performance. However, napping doesn’t provide restorative sleep. Some people sleep more on their days off than on workdays. They also may go to bed later and get up later on days off. Although extra sleep on days off might help a person feel better, it can upset the body’s sleep–wake rhythm.[29] See Figure 12.6[30] of an adult napping during the day.

Sleep deficiency can affect people even when they sleep the total number of hours recommended for their age group. For example, people whose sleep is out of sync with their body clocks (such as shift workers) or whose sleep is routinely interrupted (such as caregivers or emergency responders) often need to pay special attention to their sleep needs.[31] Individuals should also talk to a health care provider if they sleep more than eight hours a night, but don’t feel well-rested. This can indicate a sleep disorder or other health problem.[32]
Sleep Disorders
There are several sleep disorders that can cause sleep deficiency, such as insomnia, sleep apnea, and narcolepsy.
Insomnia
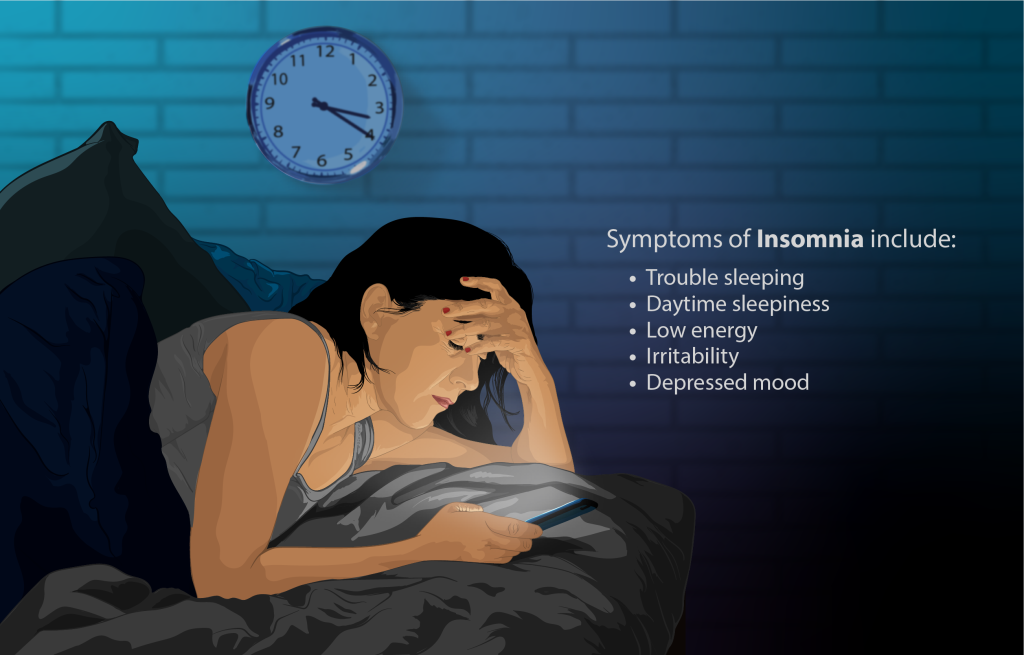
Insomnia is a common sleep disorder that causes trouble falling asleep, staying asleep, or getting good quality sleep. Insomnia interferes with daily activities and causes the person to feel unrested or sleepy during the day.[33] Short-term insomnia may be caused by stress or changes in one’s schedule or environment. It can last for a few days or weeks. Chronic insomnia occurs three or more nights a week, lasts more than three months, and cannot be fully explained by another health problem or a medication. Chronic insomnia raises the risk of high blood pressure, coronary heart disease, diabetes, and cancer.[34]
Symptoms of insomnia include the following:
- Lying awake for a long time before falling asleep. This is more common in younger adults.
- Sleeping for only short periods due to waking up often during the night or being awake for most of the night. This is the most common symptom and typically affects older adults.
- Waking up too early in the morning and not being able to get back to sleep.
- Having poor-quality of sleep that causes one to wake up feeling unrested. The person often feels sleepy during the day and has difficulty focusing on tasks. Insomnia can also cause irritability, anxiousness, and depression.[35]
See Figure 12.7[36] for an illustration of insomnia.
To diagnose insomnia, the health care provider asks about a person’s sleep habits and may request the person to keep a sleep diary for one to two weeks. A sleep diary records the time a person goes to sleep, wakes up, and takes naps each day. Timing of activities such as exercising and drinking caffeine or alcohol are also recorded, as well as feelings of sleepiness throughout the day.[37] A sleep study is a diagnostic test that monitors and records data during a client’s full night if sleep. It may be ordered to test for other sleep problems, such as circadian rhythm disorders, sleep apnea, and narcolepsy.
Treatment
Lifestyle changes often help improve short-term insomnia. The client should be educated about healthy sleep habits, such as the following:
- Make your bedroom sleep friendly. Sleep in a cool, quiet place. Avoid artificial light from the TV or electronic devices, as this can disrupt your sleep-wake cycle.
- Go to sleep and wake up around the same times each day, even on the weekends. If you can, avoid night shifts, irregular schedules, or other things that may disrupt your sleep schedule.
- Avoid caffeine, nicotine, and alcohol before bedtime. Although alcohol can make it easier to fall asleep, it triggers sleep that tends to be lighter than normal. This makes it more likely that you will wake up during the night. The effect of caffeine can last as long as eight hours.
- Get regular physical activity during the daytime (at least five to six hours before going to bed). Exercising close to bedtime can make it harder to fall asleep.
- Avoid daytime naps, especially in the afternoon. This may help you sleep longer at night.
- Eat meals on a regular schedule and avoid late-night dinners to maintain a regular sleep-wake cycle.
- Limit how much fluid you drink close to bedtime. This may help you sleep longer without having to use the bathroom.
- Learn new ways to manage stress. Follow a routine that helps you wind down and relax before bed. For example, read a book, listen to soothing music, or take a hot bath. Your doctor may also recommend massage therapy, meditation, or yoga to help you relax. Acupuncture may also help improve insomnia, especially in older adults.
- Avoid certain over-the-counter and prescription medicines that can disrupt sleep (for example, some cold and allergy medicines).[38]
A type of counseling called cognitive behavioral therapy for insomnia is usually the first treatment recommended for chronic insomnia. Several prescription medications may also be prescribed to treat insomnia. Some are meant for short-term use while others are meant for long-term use. Some insomnia medications can be habit-forming, and they all can cause dizziness, drowsiness, or worsening of depression or suicidal thoughts.[39] Common medications prescribed to treat insomnia are as follows:
- Benzodiazepines, such as lorazepam (Ativan). Benzodiazepines can be habit-forming and should be taken for only a few weeks. They can interfere with REM sleep.
- Benzodiazepine-receptor agonists, such as zolpidem (Ambien). Side effects may include anxiety. Rare side effects may include a severe allergic reaction or unintentionally doing activities while asleep such as walking, eating, or driving.
- Melatonin-receptor agonists, such as ramelteon (Rozerem). Rare side effects may include doing activities while asleep, such as walking, eating, or driving, or a severe allergic reaction.
- Orexin-receptor antagonists, such as suvorexant (Belsomra). This medicine is not recommended for people who have narcolepsy. Rare side effects may include doing activities while asleep, such as walking, eating, or driving, or not being able to move or speak for several minutes while going to sleep or waking up.[40]
Some clients use over-the-counter (OTC) products as sleep aids. Many contain antihistamines that cause sleepiness. However, they can be unsafe for some people and may not be the best treatment for insomnia. Melatonin supplements are lab-made versions of the sleep hormone melatonin. Many people take melatonin supplements to improve their sleep. However, research has not proven that melatonin is an effective treatment for insomnia. Side effects of melatonin may include daytime sleepiness, headaches, upset stomach, and worsening depression. It can also affect the body’s control of blood pressure, causing high or low blood pressure.[41]
Obstructive Sleep Apnea
Obstructive sleep apnea (OSA) is a common sleep condition that occurs when the upper airway becomes repeatedly blocked during sleep, reducing or completely stopping airflow. If the brain does not send the signals needed to breathe, the condition may be called central sleep apnea.[42]
Obstructive sleep apnea can be caused by a person’s physical structure or other medical conditions. Risk factors include obesity (causing fat deposits in the neck), large tonsils (that narrow the airway), thyroid disorders, neuromuscular disorders, heart or kidney failure (causing fluid buildup in the neck that narrows the airway), genetic syndromes (such as cleft lip or Down’s syndrome), and premature birth (before 37 weeks’ gestation).[43]
Common signs and symptoms of obstructive sleep apnea include the following:
- Reduced or absent breathing, known as apnea events
- Frequent loud snoring
- Gasping for air during sleep
- Excessive daytime sleepiness and fatigue
- Decreases in attention, vigilance, concentration, motor skills, and verbal and visuospatial memory
- Dry mouth or headaches when waking
- Sexual dysfunction or decreased libido
- Waking up often during the night to urinate[44]
Obstructive sleep apnea is diagnosed by a health care provider based on the person’s medical history, a physical exam, and results from a sleep study. During sleep studies, the number of episodes of slowed or stopped breathing events are recorded, along with documentation of oxygen levels in the blood during these events.[45]
Treatment
A breathing device, such as a CPAP machine, is a common treatment for clients with obstructive sleep apnea. CPAP stands for continuous positive airway pressure therapy. It uses mild air pressure to keep the airways open. See Figure 12.8[46] for an illustration of a CPAP.

A mouthpiece may be prescribed for clients with mild obstructive sleep apnea or if the apnea occurs only when lying on their back. Mouthpieces, or oral appliances, are custom-fit devices that are worn while sleeping. See Figure 12.9[47] for examples of mouthpieces used to treat sleep apnea. Mouthpieces are custom-fit by a dentist or an orthodontist to the client’s mouth and jaw. There are two types of mouthpieces that work differently to open the upper airway. Mandibular repositioning mouthpieces are devices that cover the upper and lower teeth and hold the jaw in a position that prevents it from blocking the upper airway. Tongue-retaining devices are mouthpieces that hold the tongue in a forward position to prevent it from blocking the upper airway.[48]

Narcolepsy
Narcolepsy is an uncommon sleep disorder that causes periods of extreme daytime sleepiness and sudden, brief episodes of deep sleep during the day. Signs and symptoms of narcolepsy include extreme daytime sleepiness; falling asleep without warning, called sleep attacks; difficulty focusing or staying awake; and waking frequently at night. Individuals may experience hallucinations while falling asleep or waking up or sleep paralysis, a feeling of being awake but being unable to move for several minutes. Narcolepsy is diagnosed based on medical history, family history, a physical exam, and a sleep study. The sleep study looks at daytime naps to identify disturbed sleep or a quick onset of rapid eye movement (REM) sleep. Treatment for narcolepsy combines medications and behavior changes. Medications used to treat narcolepsy include stimulants such as modafinil, CNS depressants such as sodium oxybate, and sedatives to improve nighttime sleep. Daytime sleepiness is often improved by promoting good quality sleep at night with scheduled naps during the day.[49]
- “The_master_circadian_clock_in_the_human_brain.jpg” by Ian B. Hickie, Sharon L. Naismith, Rébecca Robillard, Elizabeth M. Scott, and Daniel F. Hermens is licensed under CC BY 3.0 ↵
- National Institute of Neurological Disorders and Stroke. (2019, August 13). Understanding sleep. U.S. Department of Health & Human Services. https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Understanding-Sleep ↵
- National Institute of Neurological Disorders and Stroke. (2019, August 13). Understanding sleep. U.S. Department of Health & Human Services. https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Understanding-Sleep ↵
- National Heart, Lung, and Blood Institute. (n.d). Sleep deprivation and deficiency. U.S. Department of Health & Human Services. https://www.nhlbi.nih.gov/health-topics/sleep-deprivation-and-deficiency ↵
- National Heart, Lung, and Blood Institute. (n.d). Sleep deprivation and deficiency. U.S. Department of Health & Human Services. https://www.nhlbi.nih.gov/health-topics/sleep-deprivation-and-deficiency ↵
- National Institute of Neurological Disorders and Stroke. (2019, August 13). Understanding sleep. U.S. Department of Health & Human Services. https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Understanding-Sleep ↵
- National Heart, Lung, and Blood Institute. (n.d). Sleep deprivation and deficiency. U.S. Department of Health & Human Services. https://www.nhlbi.nih.gov/health-topics/sleep-deprivation-and-deficiency ↵
- National Heart, Lung, and Blood Institute. (n.d). Sleep deprivation and deficiency. U.S. Department of Health & Human Services. https://www.nhlbi.nih.gov/health-topics/sleep-deprivation-and-deficiency ↵
- National Heart, Lung, and Blood Institute. (n.d). How sleep works. U.S. Department of Health & Human Services. https://www.nhlbi.nih.gov/health-topics/how-sleep-works ↵
- National Heart, Lung, and Blood Institute. (n.d). How sleep works. U.S. Department of Health & Human Services. https://www.nhlbi.nih.gov/health-topics/how-sleep-works ↵
- National Heart, Lung, and Blood Institute. (n.d). How sleep works. U.S. Department of Health & Human Services. https://www.nhlbi.nih.gov/health-topics/how-sleep-works ↵
- “The_master_circadian_clock_in_the_human_brain.jpg” by Ian B. Hickie, Sharon L. Naismith, Rébecca Robillard, Elizabeth M. Scott, and Daniel F. Hermens is licensed under CC BY 3.0 ↵
- National Heart, Lung, and Blood Institute. (n.d). How sleep works. U.S. Department of Health & Human Services. https://www.nhlbi.nih.gov/health-topics/how-sleep-works ↵
- National Heart, Lung, and Blood Institute. (n.d). Sleep deprivation and deficiency. U.S. Department of Health & Human Services. https://www.nhlbi.nih.gov/health-topics/sleep-deprivation-and-deficiency ↵
- National Heart, Lung, and Blood Institute. (n.d). Sleep deprivation and deficiency. U.S. Department of Health & Human Services. https://www.nhlbi.nih.gov/health-topics/sleep-deprivation-and-deficiency ↵
- National Heart, Lung, and Blood Institute. (n.d). Sleep deprivation and deficiency. U.S. Department of Health & Human Services. https://www.nhlbi.nih.gov/health-topics/sleep-deprivation-and-deficiency ↵
- “6041578611_f2c9e4d164_k.jpg” by rachel CALAMUSA is licensed under CC BY-SA 2.0 ↵
- National Heart, Lung, and Blood Institute. (n.d). Sleep deprivation and deficiency. U.S. Department of Health & Human Services. https://www.nhlbi.nih.gov/health-topics/sleep-deprivation-and-deficiency ↵
- National Heart, Lung, and Blood Institute. (n.d). Sleep deprivation and deficiency. U.S. Department of Health & Human Services. https://www.nhlbi.nih.gov/health-topics/sleep-deprivation-and-deficiency ↵
- “Study_sleep.jpg” by Nic Ashman, Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- National Heart, Lung, and Blood Institute. (n.d). Sleep deprivation and deficiency. U.S. Department of Health & Human Services. https://www.nhlbi.nih.gov/health-topics/sleep-deprivation-and-deficiency ↵
- National Heart, Lung, and Blood Institute. (n.d). Sleep deprivation and deficiency. U.S. Department of Health & Human Services. https://www.nhlbi.nih.gov/health-topics/sleep-deprivation-and-deficiency ↵
- National Heart, Lung, and Blood Institute. (n.d). Sleep deprivation and deficiency. U.S. Department of Health & Human Services. https://www.nhlbi.nih.gov/health-topics/sleep-deprivation-and-deficiency ↵
- National Heart, Lung, and Blood Institute. (n.d). Sleep deprivation and deficiency. U.S. Department of Health & Human Services. https://www.nhlbi.nih.gov/health-topics/sleep-deprivation-and-deficiency ↵
- National Heart, Lung, and Blood Institute. (n.d). Sleep deprivation and deficiency. U.S. Department of Health & Human Services. https://www.nhlbi.nih.gov/health-topics/sleep-deprivation-and-deficiency ↵
- National Heart, Lung, and Blood Institute. (n.d). Sleep deprivation and deficiency. U.S. Department of Health & Human Services. https://www.nhlbi.nih.gov/health-topics/sleep-deprivation-and-deficiency ↵
- National Heart, Lung, and Blood Institute. (n.d). Sleep deprivation and deficiency. U.S. Department of Health & Human Services. https://www.nhlbi.nih.gov/health-topics/sleep-deprivation-and-deficiency ↵
- “8609141689_ff923d2934_k.jpg” by Navy_NADAP is licensed under CC BY-NC-ND 2.0 ↵
- National Heart, Lung, and Blood Institute. (n.d). Sleep deprivation and deficiency. U.S. Department of Health & Human Services. https://www.nhlbi.nih.gov/health-topics/sleep-deprivation-and-deficiency ↵
- “Sleeping_man_J2.jpg” by Jamain is licensed under CC BY-SA 3.0 ↵
- National Heart, Lung, and Blood Institute. (n.d). Sleep deprivation and deficiency. U.S. Department of Health & Human Services. https://www.nhlbi.nih.gov/health-topics/sleep-deprivation-and-deficiency ↵
- National Heart, Lung, and Blood Institute. (n.d). Sleep deprivation and deficiency. U.S. Department of Health & Human Services. https://www.nhlbi.nih.gov/health-topics/sleep-deprivation-and-deficiency ↵
- National Heart, Lung, and Blood Institute. (n.d). Insomnia. U.S. Department of Health & Human Services. https://www.nhlbi.nih.gov/health-topics/insomnia ↵
- National Heart, Lung, and Blood Institute. (n.d). Insomnia. U.S. Department of Health & Human Services. https://www.nhlbi.nih.gov/health-topics/insomnia ↵
- National Heart, Lung, and Blood Institute. (n.d). Insomnia. U.S. Department of Health & Human Services. https://www.nhlbi.nih.gov/health-topics/insomnia ↵
- “Depiction_of_a_person_suffering_from_Insomnia_(sleeplessness).png” by https://www.myupchar.com/en is licensed under CC BY-SA 4.0 ↵
- National Heart, Lung, and Blood Institute. (n.d). Insomnia. U.S. Department of Health & Human Services. https://www.nhlbi.nih.gov/health-topics/insomnia ↵
- National Heart, Lung, and Blood Institute. (n.d). Insomnia. U.S. Department of Health & Human Services. https://www.nhlbi.nih.gov/health-topics/insomnia ↵
- National Heart, Lung, and Blood Institute. (n.d). Insomnia. U.S. Department of Health & Human Services. https://www.nhlbi.nih.gov/health-topics/insomnia ↵
- National Heart, Lung, and Blood Institute. (n.d). Insomnia. U.S. Department of Health & Human Services. https://www.nhlbi.nih.gov/health-topics/insomnia ↵
- National Heart, Lung, and Blood Institute. (n.d). Insomnia. U.S. Department of Health & Human Services. https://www.nhlbi.nih.gov/health-topics/insomnia ↵
- National Heart, Lung, and Blood Institute. (n.d). Sleep apnea. U.S. Department of Health & Human Services. https://www.nhlbi.nih.gov/health-topics/sleep-apnea ↵
- National Heart, Lung, and Blood Institute. (n.d). Sleep apnea. U.S. Department of Health & Human Services. https://www.nhlbi.nih.gov/health-topics/sleep-apnea ↵
- National Heart, Lung, and Blood Institute. (n.d). Sleep apnea. U.S. Department of Health & Human Services. https://www.nhlbi.nih.gov/health-topics/sleep-apnea ↵
- National Heart, Lung, and Blood Institute. (n.d). Sleep apnea. U.S. Department of Health & Human Services. https://www.nhlbi.nih.gov/health-topics/sleep-apnea ↵
- “Depiction_of_a_Sleep_Apnea_patient_using_a_CPAP_machine.png” by https://www.myupchar.com/en is licensed under CC BY-SA 4.0 ↵
- “Orthoapnea_,_oral_appliance.jpg” by Orthoapnea is licensed under CC BY-SA 3.0 and “3D_printed_mouthpeace.jpg” by unknown author is licensed under CC BY 3.0 ↵
- National Heart, Lung, and Blood Institute. (n.d). Sleep apnea. U.S. Department of Health & Human Services. https://www.nhlbi.nih.gov/health-topics/sleep-apnea ↵
- National Heart, Lung, and Blood Institute. (n.d). Narcolepsy. U.S. Department of Health & Human Services. https://www.nhlbi.nih.gov/health-topics/narcolepsy ↵
The capacity to determine one’s own actions through independent choice, including demonstration of competence.
Metabolism is the sum of all biochemical processes that occur within the body to maintain life, including the conversion of food into energy, the synthesis of essential molecules, and the elimination of waste products. The endocrine system, composed of glands that secrete hormones, plays a critical role in regulating metabolism. Hormones such as insulin, thyroid hormones, and parathyroid hormone (PTH) are essential for maintaining metabolic homeostasis. This chapter focuses on key metabolic and endocrine disorders, including diabetes mellitus, thyroid disease, and parathyroid disease. Understanding these conditions, their pathophysiology, clinical manifestations, and treatment options is vital for providing effective nursing care and managing these chronic conditions.
Overview of Metabolism
Metabolism encompasses all the chemical reactions that occur within the body’s cells. These reactions are divided into two categories:
- Catabolism: The breakdown of complex molecules into simpler ones, releasing energy. This process provides the energy required for various cellular functions.
- Anabolism: The synthesis of complex molecules from simpler ones, requiring energy. Anabolism supports cell growth, repair, and the storage of energy for future use.
Hormones regulate these metabolic processes, ensuring that the body maintains a balance between energy production and energy consumption.
Metabolic and endocrine disorders such as diabetes mellitus, thyroid disease, and parathyroid disease have significant impacts on overall health and require comprehensive management. Nurses play a critical role in educating patients, managing symptoms, and coordinating care for individuals with these conditions. Understanding the pathophysiology, clinical manifestations, and treatment options for these disorders is essential for providing high-quality nursing care and improving patient outcomes. Effective management of these conditions involves a multidisciplinary approach that includes lifestyle modifications, pharmacological therapy, and regular monitoring to prevent complications and promote optimal health.
The act or process of pleading for, supporting, or recommending a cause or course of action.
Diabetes mellitus is a group of metabolic disorders characterized by chronic hyperglycemia (high blood sugar) resulting from defects in insulin secretion, insulin action, or both. Diabetes is a leading cause of morbidity and mortality worldwide, and its complications can affect multiple organ systems.
- Pathophysiology
- Insulin and Glucose Metabolism: Insulin, a hormone produced by the pancreas, plays a key role in glucose metabolism. It facilitates the uptake of glucose by cells for energy production and storage as glycogen. In diabetes, insulin production is insufficient (Type 1 diabetes) or the body's cells are resistant to insulin's effects (Type 2 diabetes), leading to elevated blood glucose levels.
- Types of Diabetes:
- Type 1 Diabetes: An autoimmune condition where the immune system attacks and destroys insulin-producing beta cells in the pancreas, leading to an absolute deficiency of insulin. It typically presents in childhood or adolescence.
- Type 2 Diabetes: Characterized by insulin resistance and relative insulin deficiency. It is more common in adults and is strongly associated with obesity, physical inactivity, and genetic factors.
- Gestational Diabetes: A form of diabetes that occurs during pregnancy and typically resolves after delivery, though it increases the risk of developing Type 2 diabetes later in life.
- Clinical Manifestations
- Hyperglycemia: Persistent high blood sugar levels are the hallmark of diabetes and may cause symptoms such as excessive thirst (polydipsia), frequent urination (polyuria), and increased hunger (polyphagia).
- Fatigue and Weakness: Due to the body’s inability to use glucose efficiently for energy.
- Blurred Vision: Resulting from osmotic changes in the lens of the eye due to high blood glucose levels.
- Weight Loss: Particularly in Type 1 diabetes, where the body breaks down fat and muscle for energy due to the lack of insulin.
- Diagnosis
- The diagnosis of diabetes is primarily based on laboratory tests that measure blood glucose levels. Several tests are available, each with specific criteria for diagnosing diabetes.
- Fasting Plasma Glucose (FPG) Test
- Description: The FPG test measures blood glucose levels after an individual has fasted for at least 8 hours.
- Diagnostic Criteria:
-
- Normal: FPG < 100 mg/dL (5.6 mmol/L)
- Prediabetes: FPG 100–125 mg/dL (5.6–6.9 mmol/L)
- Diabetes: FPG ≥ 126 mg/dL (7.0 mmol/L) on two separate occasions
-
- Clinical Significance: The FPG test is a simple and widely used screening tool for diabetes. Elevated fasting glucose levels indicate impaired insulin function and the presence of hyperglycemia, a hallmark of diabetes.
- Oral Glucose Tolerance Test (OGTT)
- Description: The OGTT measures blood glucose levels before and 2 hours after the ingestion of a 75-gram glucose solution.
- Diagnostic Criteria:
- Normal: 2-hour plasma glucose < 140 mg/dL (7.8 mmol/L)
- Prediabetes: 2-hour plasma glucose 140–199 mg/dL (7.8–11.0 mmol/L)
- Diabetes: 2-hour plasma glucose ≥ 200 mg/dL (11.1 mmol/L)
- Diagnostic Criteria:
- Clinical Significance: The OGTT is particularly useful in diagnosing gestational diabetes and assessing glucose tolerance in individuals with impaired fasting glucose (IFG). It provides a more comprehensive assessment of the body's ability to handle glucose.
- Description: The OGTT measures blood glucose levels before and 2 hours after the ingestion of a 75-gram glucose solution.
- Glycated Hemoglobin (HbA1c) Test
- Description: The HbA1c test measures the percentage of hemoglobin that is glycated (bound to glucose) over the past 2 to 3 months.
- Diagnostic Criteria:
- Normal: HbA1c < 5.7%
- Prediabetes: HbA1c 5.7%–6.4%
- Diabetes: HbA1c ≥ 6.5% on two separate occasions
- Clinical Significance: The HbA1c test provides an overview of long-term blood glucose control and is a key diagnostic and monitoring tool in diabetes management. It reflects average blood glucose levels over a period, offering insight into the effectiveness of treatment strategies.
- Random Plasma Glucose Test
- Description: This test measures blood glucose levels at any time of the day, regardless of fasting status.
- Diagnostic Criteria:
- Diabetes: Random plasma glucose ≥ 200 mg/dL (11.1 mmol/L) with symptoms of hyperglycemia (e.g., polyuria, polydipsia, unexplained weight loss)
- Clinical Significance: The random plasma glucose test is often used in the presence of classic diabetes symptoms to confirm a diagnosis quickly, especially in emergency settings.
- Monitoring Glycemic Control
- Once diabetes is diagnosed, ongoing monitoring of blood glucose levels is essential to assess the effectiveness of treatment and prevent complications. Several tests are commonly used for this purpose.
- Self-Monitoring of Blood Glucose (SMBG)
- Description: SMBG involves patients using a glucometer to measure their blood glucose levels at various times throughout the day.
- Clinical Significance: SMBG is crucial for patients on insulin therapy, providing immediate feedback on blood glucose levels and allowing for real-time adjustments in insulin dosing, diet, and physical activity. It helps in preventing both hyperglycemia and hypoglycemia.
- Continuous Glucose Monitoring (CGM)
- Description: CGM systems use a sensor placed under the skin to continuously measure glucose levels in interstitial fluid, providing real-time glucose readings every few minutes.
- Clinical Significance: CGM offers a more comprehensive picture of glucose trends throughout the day and night, identifying patterns and fluctuations that may not be captured by SMBG alone. CGM is particularly useful for patients with Type 1 diabetes and those experiencing frequent hypoglycemia.
- Management of Diabetes Mellitus
- Lifestyle Modifications: Diet and exercise are foundational to diabetes management. Patients are advised to follow a balanced diet with controlled carbohydrate intake and engage in regular physical activity.
- Pharmacological Treatment:
- Insulin Therapy: Essential for patients with Type 1 diabetes and some patients with advanced Type 2 diabetes.
- Oral Hypoglycemic Agents: Such as metformin, sulfonylureas, and DPP-4 inhibitors, are used to manage blood glucose levels in Type 2 diabetes.
- Continuous Glucose Monitoring (CGM): Technology that provides real-time data on blood glucose levels, allowing for more precise management.
- Patient Education: Nurses play a critical role in educating patients about blood glucose monitoring, medication adherence, recognizing signs of hypo- and hyperglycemia, and the importance of regular follow-up.
- Complications of Diabetes Mellitus
- Acute Complications: Include diabetic ketoacidosis (DKA) in Type 1 diabetes, characterized by severe hyperglycemia, ketonemia, and metabolic acidosis, and hyperosmolar hyperglycemic state (HHS) in Type 2 diabetes, marked by extreme hyperglycemia without significant ketosis.
- Chronic Complications: Long-term complications of poorly managed diabetes include cardiovascular disease, neuropathy, nephropathy, retinopathy, and increased susceptibility to infections.
Assessing and Monitoring Complications
Diabetes can lead to various complications, including cardiovascular disease, nephropathy, retinopathy, and neuropathy. Laboratory and diagnostic tests are essential for the early detection and monitoring of these complications.
- Lipid Profile
- Description: The lipid profile measures total cholesterol, low-density lipoprotein (LDL), high-density lipoprotein (HDL), and triglycerides.
- Clinical Significance: Diabetes is associated with an increased risk of cardiovascular disease. Regular monitoring of lipid levels is important for managing this risk. LDL is typically targeted for reduction to prevent atherosclerosis, while HDL and triglycerides are also important markers of cardiovascular health.
- Urine Albumin-to-Creatinine Ratio (UACR)
- Description: The UACR test measures the amount of albumin in the urine, relative to creatinine, to assess kidney function.
- Clinical Significance: Microalbuminuria (30–299 mg/g creatinine) is an early indicator of diabetic nephropathy. Regular UACR testing helps in detecting kidney damage at an early stage, allowing for timely interventions to prevent progression to end-stage renal disease (ESRD).
- Serum Creatinine and Estimated Glomerular Filtration Rate (eGFR)
- Description: Serum creatinine is used to estimate glomerular filtration rate (eGFR), a measure of kidney function.
- Clinical Significance: Monitoring eGFR provides insight into the severity of kidney impairment. A declining eGFR may indicate the progression of diabetic nephropathy, necessitating adjustments in treatment to protect kidney function.
- Retinal Examination
- Description: Regular retinal examinations, often performed using fundus photography or optical coherence tomography (OCT), are essential for detecting diabetic retinopathy.
- Clinical Significance: Diabetic retinopathy is a leading cause of blindness in adults. Early detection through regular eye exams allows for timely interventions, such as laser therapy or intravitreal injections, to prevent vision loss.
- Nerve Conduction Studies (NCS) and Electromyography (EMG)
- Description: NCS and EMG are used to assess nerve function and detect peripheral neuropathy.
- Clinical Significance: Diabetic neuropathy can lead to significant morbidity, including pain, loss of sensation, and an increased risk of foot ulcers. Nerve conduction studies help in diagnosing neuropathy early, allowing for interventions to manage symptoms and prevent complications.
Advanced Diagnostic Techniques
- In addition to standard laboratory tests, advanced diagnostic techniques are increasingly being used to assess and manage diabetes and its complications.
- Insulin and C-Peptide Levels
- Description: Measuring insulin and C-peptide levels helps differentiate between Type 1 and Type 2 diabetes and assess beta-cell function.
- Clinical Significance: Low insulin and C-peptide levels are indicative of Type 1 diabetes, while elevated levels suggest insulin resistance, as seen in Type 2 diabetes. These tests can guide treatment decisions, particularly in atypical cases.
- Genetic Testing
- Description: Genetic testing can identify specific mutations associated with monogenic forms of diabetes, such as MODY (Maturity-Onset Diabetes of the Young).
- Clinical Significance: Identifying the genetic basis of diabetes can lead to personalized treatment approaches and a better understanding of disease risk in family members.
- Advanced Imaging Techniques
- Description: Techniques such as coronary artery calcium (CAC) scoring, cardiac MRI, and Doppler ultrasound are used to assess cardiovascular risk and complications in diabetic patients.
- Clinical Significance: Diabetes significantly increases the risk of cardiovascular disease. Advanced imaging techniques provide detailed information on cardiovascular health, allowing for more targeted and effective interventions.
Humble and respectful attitude towards individuals of other cultures and an approach to learning about other cultures as a lifelong goal and process.
The bioethical principle of benefiting others by preventing harm, removing harmful conditions, or affirmatively acting to benefit another or others, often going beyond what is required by law.
A moral obligation to act on the basis of equality and equity and a standard linked to fairness for all in society.
Parathyroid Disease
The parathyroid glands, located behind the thyroid gland, produce parathyroid hormone (PTH), which regulates calcium levels in the blood. Disorders of the parathyroid glands can lead to significant metabolic imbalances.
- Hyperparathyroidism
- Pathophysiology: Hyperparathyroidism is characterized by the overproduction of PTH, leading to elevated calcium levels in the blood (hypercalcemia). This condition can be primary (due to a parathyroid adenoma or hyperplasia) or secondary (as a response to chronic hypocalcemia, often seen in chronic kidney disease).
- Clinical Manifestations:
- Hypercalcemia: Elevated calcium levels can cause symptoms such as muscle weakness, fatigue, constipation, and polyuria.
- Bone Pain and Fractures: Excess PTH causes bone resorption, leading to osteoporosis and an increased risk of fractures.
- Kidney Stones: High calcium levels can lead to the formation of kidney stones.
- Psychiatric Symptoms: Patients may experience depression, confusion, or memory problems.
- Diagnosis: Elevated serum calcium and PTH levels confirm the diagnosis. Bone density tests and imaging studies may be used to assess the extent of bone involvement.
- Management:
- Surgical Removal: Parathyroidectomy is the definitive treatment for primary hyperparathyroidism.
- Medications: Calcimimetics and bisphosphonates may be used to manage hypercalcemia and protect bone density.
- Monitoring: Regular monitoring of calcium and PTH levels is essential, along with bone density assessments.
- Hypoparathyroidism
- Pathophysiology: Hypoparathyroidism is characterized by insufficient production of PTH, leading to low calcium levels in the blood (hypocalcemia). It can occur after thyroid or parathyroid surgery or be idiopathic.
- Clinical Manifestations:
- Hypocalcemia: Symptoms include muscle cramps, tetany (muscle spasms), numbness, and tingling in the fingers and toes.
- Chvostek’s and Trousseau’s Signs: Positive Chvostek’s sign (twitching of facial muscles when tapped) and Trousseau’s sign (carpal spasm with blood pressure cuff inflation) indicate hypocalcemia.
- Seizures: Severe hypocalcemia can lead to seizures.
- Diagnosis: Low serum calcium and PTH levels confirm the diagnosis. Phosphate levels may be elevated due to the lack of PTH.
- Management:
- Calcium and Vitamin D Supplements: These are the mainstays of treatment to maintain normal calcium levels.
- PTH Replacement: In some cases, synthetic PTH (teriparatide) may be used to manage chronic hypoparathyroidism.
- Monitoring: Regular monitoring of calcium levels is necessary to prevent complications of hypocalcemia.

