Open Resources for Nursing (Open RN)
Phases of Wound Healing
When skin is injured, there are four phases of wound healing that take place: hemostasis, inflammatory, proliferative, and maturation.[1] See Figure 20.1[2] for an illustration of the phases of wound healing.
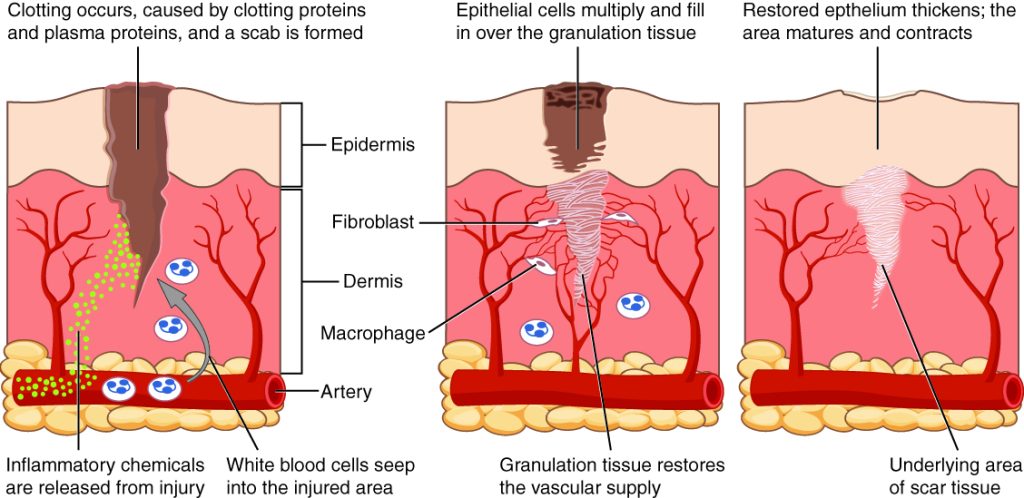
To illustrate the phases of wound healing, imagine that you accidentally cut your finger with a knife as you were slicing an apple. Immediately after the injury occurs, blood vessels constrict, and clotting factors are activated. This is referred to as the hemostasis phase. Clotting factors form clots that stop the bleeding and act as a barrier to prevent bacterial contamination. Platelets release growth factors that alert various cells to start the repair process at the wound location. The hemostasis phase lasts up to 60 minutes, depending on the severity of the injury.[3],[4]
After the hemostasis phase, the inflammatory phase begins. Vasodilation occurs so that white blood cells in the bloodstream can move into the wound to start cleaning the wound bed. The inflammatory process appears to the observer as edema (swelling), erythema (redness), and exudate. Exudate is fluid that oozes out of a wound, also commonly called pus.[5],[6]
The proliferative phase begins within a few days after the injury and includes four important processes: epithelialization, angiogenesis, collagen formation, and contraction. Epithelialization refers to the development of new epidermis and granulation tissue. Granulation tissue is new connective tissue with new, fragile, thin-walled capillaries. Collagen is formed to provide strength and integrity to the wound. At the end of the proliferation phase, the wound begins to contract in size.[7],[8]
Capillaries begin to develop within the wound 24 hours after injury during a process called angiogenesis. These capillaries bring more oxygen and nutrients to the wound for healing. When performing dressing changes, it is essential for the nurse to protect this granulation tissue and the associated new capillaries. Healthy granulation tissue appears pink due to the new capillary formation. It is also moist, painless to the touch, and may appear “bumpy.” Conversely, unhealthy granulation tissue is dark red and painful. It bleeds easily with minimal contact and may be covered by shiny white or yellow fibrous tissue referred to as biofilm that must be removed because it impedes healing. Unhealthy granulation tissue is often caused by an infection, so wound cultures should be obtained when infection is suspected. The provider can then prescribe appropriate antibiotic treatment based on the culture results.[9]
During the maturation phase, collagen continues to be created to strengthen the wound. Collagen contributes strength to the wound to prevent it from reopening. A wound typically heals within 4-5 weeks and often leaves behind a scar. The scar tissue is initially firm, red, and slightly raised from the excess collagen deposition. Over time, the scar begins to soften, flatten, and become pale in about nine months.[10]
Types of Wound Healing
There are three types of wound healing: primary intention, secondary intention, and tertiary intention. Healing by primary intention means that the wound is sutured, stapled, glued, or otherwise closed so the wound heals beneath the closure. This type of healing occurs with clean-edged lacerations or surgical incisions, and the closed edges are referred to as approximated. See Figure 20.2[11] for an image of a surgical wound healing by primary intention.

Secondary intention occurs when the edges of a wound cannot be approximated (brought together), so the wound fills in from the bottom up by the production of granulation tissue. Examples of wounds that heal by secondary intention are pressure injuries and chainsaw injuries. Wounds that heal by secondary intention are at higher risk for infection and must be protected from contamination. See Figure 20.3[12] for an image of a wound healing by secondary intention.

Tertiary intention refers to a wound that has had to remain open or has been reopened, often due to severe infection. The wound is typically closed at a later date when infection has resolved. Wounds that heal by secondary and tertiary intention have delayed healing times and increased scar tissue.
Wound Closures
Lacerations and surgical wounds are typically closed with sutures, staples, or dermabond to facilitate healing by primary intention. See Figure 20.4[13] for an image of sutures, Figure 20.5[14] for an image of staples, and Figure 20.6[15] for an image of a wound closed with dermabond, a type of sterile surgical glue. Based on agency policy, the nurse may remove sutures and staples based on a provider order. See Figure 20.7[16] for an image of a disposable staple remover. See the checklists in the subsections later in this chapter for procedures related to surgical and staple removal.




Common Types of Wounds
There are several different types of wounds. It is important to understand different types of wounds when providing wound care because each type of wound has different characteristics and treatments. Additionally, treatments that may be helpful for one type of wound can be harmful for another type. Common types of wounds include skin tears, venous ulcers, arterial ulcers, diabetic foot wounds, and pressure injuries.[17]
Skin Tears
Skin tears are wounds caused by mechanical forces such as shear, friction, or blunt force. They typically occur in the fragile, nonelastic skin of older adults or in patients undergoing long-term corticosteroid therapy. Skin tears can be caused by the simple mechanical force used to remove an adhesive bandage or from friction as the skin brushes against a surface. Skin tears occur in the epidermis and dermis but do not extend through the subcutaneous layer. The wound bases of skin tears are typically fragile and bleed easily.[18]
Venous Ulcers
Venous ulcers are caused by lack of blood return to the heart causing pooling of fluid in the veins of the lower legs. The resulting elevated hydrostatic pressure in the veins causes fluid to seep out, macerate the skin, and cause venous ulcerations. Maceration refers to the softening and wasting away of skin due to excess fluid. Venous ulcers typically occur on the medial lower leg and have irregular edges due to the maceration. There is often a dark-colored discoloration of the lower legs, due to blood pooling and leakage of iron into the skin called hemosiderin staining. For venous ulcers to heal, compression dressings must be used, along with multilayer bandage systems, to control edema and absorb large amounts of drainage.[19] See Figure 20.8[20] for an image of a venous ulcer.

Arterial Ulcers
Arterial ulcers are caused by lack of blood flow and oxygenation to tissues. They typically occur in the distal areas of the body such as the feet, heels, and toes. Arterial ulcers have well-defined borders with a “punched out” appearance where there is a localized lack of blood flow. They are typically painful due to the lack of oxygenation to the area. The wound base may become necrotic (black) due to tissue death from ischemia. Wound dressings must maintain a moist environment, and treatment must include the removal of necrotic tissue. In severe arterial ulcers, vascular surgery may be required to reestablish blood supply to the area.[21] See Figure 20.9[22] for an image of an arterial ulcer on a patient’s foot.

Diabetic Ulcers
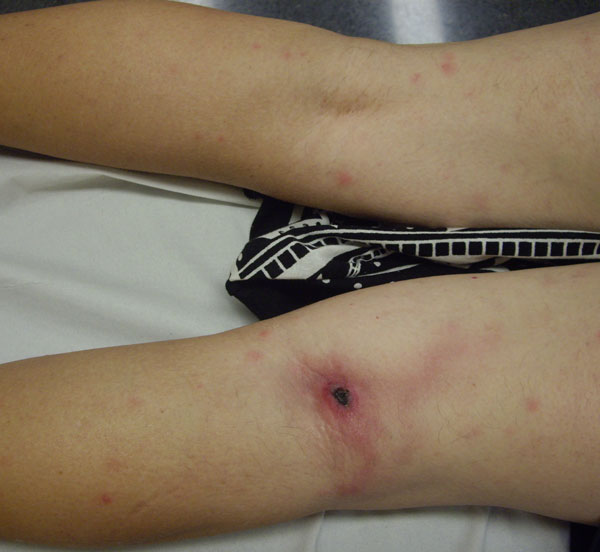
Diabetic ulcers are also called neuropathic ulcers because peripheral neuropathy is commonly present in patients with diabetes. Peripheral neuropathy is a medical condition that causes decreased sensation of pain and pressure, especially in the lower extremities. Diabetic ulcers typically develop on the plantar aspect of the feet and toes of a patient with diabetes due to lack of sensation of pressure or injury. See Figure 20.10[23] for an image of a diabetic ulcer. Wound healing is compromised in patients with diabetes due to the disease process. In addition, there is a higher risk of developing an infection that can reach the bone requiring amputation of the area. To prevent diabetic ulcers from occurring, it is vital for nurses to teach meticulous foot care to patients with diabetes and encourage the use of well-fitting shoes.[24]

Pressure Injuries
Pressure injuries are defined as “localized damage to the skin or underlying soft tissue, usually over a bony prominence, as a result of intense and prolonged pressure in combination with shear.”[25] Shear occurs when tissue layers move over the top of each other, causing blood vessels to stretch and break as they pass through the subcutaneous tissue. For example, when a patient slides down in bed, the outer skin remains immobile because it remains attached to the sheets due to friction, but deeper tissue attached to the bone moves as the patient slides down. This opposing movement of the outer layer of skin and the underlying tissues causes the capillaries to stretch and tear, which then impacts the blood flow and oxygenation of the surrounding tissues.
Braden Scale
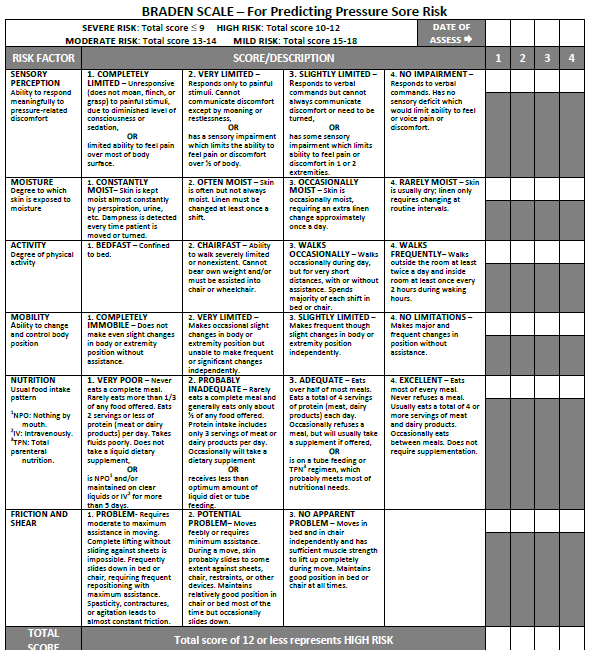
Several factors place a patient at risk for developing pressure injuries, including nutrition, mobility, sensation, and moisture. The Braden Scale is a tool commonly used in health care to provide an objective assessment of a patient’s risk for developing pressure injuries. See Figure 20.11[26] for an image of a Braden Scale. The six risk factors included on the Braden Scale are sensory perception, moisture, activity, mobility, nutrition, and friction/shear, and these factors are rated on a scale from 1-4 with 1 being “completely limited” to 4 being “no impairment.” The scores from the six categories are added, and the total score indicates a patient’s risk for developing a pressure injury. A total score of 15-19 indicates mild risk, 13-14 indicates moderate risk, 10-12 indicates high risk, and less than or equal to 9 indicates severe risk. Nurses create care plans using these scores to plan interventions that prevent or treat pressure injuries.
For more information about using the Braden Scale, go to the “Integumentary” chapter of the Open RN Nursing Fundamentals textbook.
Staging
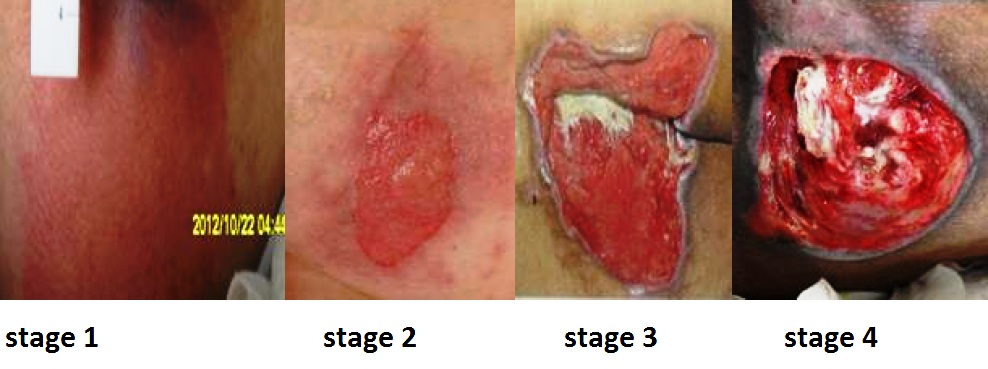
Pressure injuries commonly occur on the sacrum, heels, ischial tuberosity, and coccyx. The 2016 National Pressure Ulcer Advisory Panel (NPUAP) Pressure Injury Staging System now uses the term “pressure injury” instead of pressure ulcer because an injury can occur without an ulcer present. Pressure injuries are staged from 1 through 4 based on the extent of tissue damage. For example, Stage 1 pressure injuries have reddened but intact skin, and Stage 4 pressure injuries have deep, open ulcers affecting underlying tissue and structures such as muscles, ligaments, and tendons. See Figure 20.12[27] for an image of the four stages of pressure injuries.[28] The NPUAP’s definitions of the four stages of pressure injuries are described below:
- Stage 1 pressure injuries are intact skin with a localized area of nonblanchable erythema where prolonged pressure has occurred. Nonblanchable erythema is a medical term used to describe skin redness that does not turn white when pressed.
- Stage 2 pressure injuries are partial-thickness loss of skin with exposed dermis. The wound bed is viable and may appear like an intact or ruptured blister. Stage 2 pressure injuries heal by reepithelialization and not by granulation tissue formation.[29]
- Stage 3 pressure injuries are full-thickness tissue loss in which fat is visible, but cartilage, tendon, ligament, muscle, and bone are not exposed. The depth of tissue damage varies by anatomical location. Undermining and tunneling may occur in Stage 3 and 4 pressure injuries. Undermining occurs when the tissue under the wound edges becomes eroded, resulting in a pocket beneath the skin at the wound’s edge. Tunneling refers to passageways underneath the surface of the skin that extend from a wound and can take twists and turns. Slough and eschar may also be present in Stage 3 and 4 pressure injuries. Slough is an inflammatory exudate that is usually light yellow, soft, and moist. Eschar is dark brown/black, dry, thick, and leathery dead tissue. See Figure 20.13 [30] for an image of eschar in the center of the wound. If slough or eschar obscures the wound so that tissue loss cannot be assessed, the pressure injury is referred to as unstageable.[31] In most wounds, slough and eschar must be removed by debridement for healing to occur.
- Stage 4 pressure injuries are full-thickness tissue loss like Stage 3 pressure injuries, but also have exposed cartilage, tendon, ligament, muscle, or bone. Osteomyelitis (bone infection) may be present.[32]
View a supplementary YouTube video on Pressure Injuries[33]
Factors Affecting Wound Healing
Multiple factors affect a wound’s ability to heal and are referred to as local and systemic factors. Local factors refer to factors that directly affect the wound, whereas systemic factors refer to the overall health of the patient and their ability to heal. Local factors include localized blood flow and oxygenation of the tissue, the presence of infection or a foreign body, and venous sufficiency. Venous insufficiency is a medical condition where the veins in the legs do not adequately send blood back to the heart, resulting in a pooling of fluids in the legs.[34]
Systemic factors that affect a patient’s ability to heal include nutrition, mobility, stress, diabetes, age, obesity, medications, alcohol use, and smoking.[35] When a nurse is caring for a patient with a wound that is not healing as anticipated, it is important to further assess for the potential impact of these factors:
- Nutrition. Nutritional deficiencies can have a profound impact on healing and must be addressed for chronic wounds to heal. Protein is one of the most important nutritional factors affecting wound healing. For example, in patients with pressure injuries, 30 to 35 kcal/kg of calorie intake with 1.25 to 1.5g/kg of protein and micronutrients supplementation is recommended daily.[36] In addition, vitamin C and zinc deficiency have many roles in wound healing. It is important to collaborate with a dietician to identify and manage nutritional deficiencies when a patient is experiencing poor wound healing.[37]
- Stress. Stress causes an impaired immune response that results in delayed wound healing. Although a patient cannot necessarily control the amount of stress in their life, it is possible to control one’s reaction to stress with healthy coping mechanisms. The nurse can help educate the patient about healthy coping strategies.
- Diabetes. Diabetes causes delayed wound healing due to many factors such as neuropathy, atherosclerosis (a buildup of plaque that obstructs blood flow in the arteries resulting in decreased oxygenation of tissues), a decreased host immune resistance, and increased risk for infection.[38] Read more about neuropathy and diabetic ulcers under the “Common Types of Wounds” subsection. Nurses provide vital patient education to patients with diabetes to effectively manage the disease process for improved wound healing.
- Age. Older adults have an altered inflammatory response that can impair wound healing. Nurses can educate patients about the importance of exercise for improved wound healing in older adults.[39]
- Obesity. Obese individuals frequently have wound complications, including infection, dehiscence, hematoma formation, pressure injuries, and venous injuries. Nurses can educate patients about healthy lifestyle choices to reduce obesity in patients with chronic wounds.[40]
- Medications. Medications such as corticosteroids impair wound healing due to reduced formation of granulation tissue.[41] When assessing a chronic wound that is not healing as expected, it is important to consider the side effects of the patient’s medications.
- Alcohol consumption. Research shows that exposure to alcohol impairs wound healing and increases the incidence of infection.[42] Patients with impaired healing of chronic wounds should be educated to avoid alcohol consumption.
- Smoking. Smoking impacts the inflammatory phase of the wound healing process, resulting in poor wound healing and an increased risk of infection.[43] Patients who smoke should be encouraged to stop smoking.
Lab Values Affecting Wound Healing
When a chronic wound is not healing as expected, laboratory test results may provide additional clues regarding the causes of the delayed healing. See Table 20.2 for lab results that offer clues to systemic issues causing delayed wound healing.[44]
Table 20.2 Lab Values Associated with Delayed Wound Healing[45]
| Abnormal Lab Value | Rationale |
|---|---|
| Low hemoglobin | Low hemoglobin indicates less oxygen is transported to the wound site. |
| Elevated white blood cells (WBC) | Increased WBC indicates infection is occurring. |
| Low platelets | Platelets are important during the proliferative phase in the creation of granulation tissue and angiogenesis.[46] |
| Low albumin | Low albumin indicates decreased protein levels. Protein is required for effective wound healing. |
| Elevated blood glucose or hemoglobin A1C | Elevated blood glucose and hemoglobin A1C levels indicate poor management of diabetes mellitus, a disease that impacts wound healing. |
| Elevated serum BUN and creatinine | BUN and creatinine levels are indicators of kidney function, with elevated levels indicating worsening kidney function. Elevated BUN (blood urea nitrogen) levels impact wound healing. |
| Positive wound culture | Positive wound cultures indicate an infection is present and provide additional information, including the type and number of bacteria present, as well as identifying antibiotics to which the bacteria is susceptible. The nurse reviews this information when administering antibiotics to ensure the prescribed therapy is effective for the type of bacteria present. |
Wound Complications
In addition to delayed wound healing, several other complications can occur. Three common complications are the development of a hematoma, infection, or dehiscence. These complications should be immediately reported to the health care provider.
Hematoma
A hematoma is an area of blood that collects outside of the larger blood vessels. A hematoma is more severe than ecchymosis (bruising) that occurs when small veins and capillaries under the skin break. The development of a hematoma at a surgical site can lead to infection and incisional dehiscence.[47] See Figure 20.14[48] for an image of a hematoma.

Infection
A break in the skin allows bacteria to enter and begin to multiply. Microbial contamination of wounds can progress from localized infection to systemic infection, sepsis, and subsequent life- and limb-threatening infection. Signs of a localized wound infection include redness, warmth, and tenderness around the wound. Purulent or malodorous drainage may also be present. Signs that a systemic infection is developing and requires urgent medical management include the following[49]:
- Fever over 101 F (38 C)
- Overall malaise (lack of energy and not feeling well)
- Change in level of consciousness/increased confusion
- Increasing or continual pain in the wound
- Expanding redness or swelling around the wound
- Loss of movement or function of the wounded area
Dehiscence
Dehiscence refers to the separation of the edges of a surgical wound. A dehisced wound can appear fully open where the tissue underneath is visible, or it can be partial where just a portion of the wound has torn open. Wound dehiscence is always a risk in a surgical wound, but the risk increases if the patient is obese, smokes, or has other health conditions, such as diabetes, that impact wound healing. Additionally, the location of the wound and the amount of physical activity in that area also increase the chances of wound dehiscence.[50] See Figure 20.15[51] for an image of dehiscence in an abdominal surgical wound in a 50-year-old obese female with a history of smoking and malnutrition.
Wound dehiscence can occur suddenly, especially in abdominal wounds when the patient is coughing or straining. Evisceration is a rare but severe surgical complication when dehiscence occurs, and the abdominal organs protrude out of the incision. Signs of impending dehiscence include redness around the wound margins and increasing drainage from the incision. The wound will also likely become increasingly painful. Suture breakage can be a sign that the wound has minor dehiscence or is about to dehisce.[52]
To prevent wound dehiscence, surgical patients must follow all post-op instructions carefully. The patient must move carefully and protect the skin from being pulled around the wound site. They should also avoid tensing the muscles surrounding the wound and avoid heavy lifting as advised.[53]

- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology and is licensed under CC BY 4.0 ↵
- “417 Tissue Repair.jpg” by OpenStax College is licensed under CC BY 3.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology and is licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Grubbs and Mannah and is licensed under CC BY 4.0 ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology and is licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Grubbs and Mannah and is licensed under CC BY 4.0 ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology and is licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Grubbs and Mannah and is licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Alhajj, Bansal, and Goyal and is licensed under CC BY 4.0 ↵
- This work is a derivative of StatPearls by Grubbs and Mannah and is licensed under CC BY 4.0 ↵
- “Ventriculoperitoneal shunt - surgical wound healing - belly - day 12.jpg” by Hansmuller is licensed under CC BY-SA 4.0 ↵
- “Atrophied skin.png” by sansea2 is licensed under CC BY-SA 3.0 ↵
- “Wound closed with surgical sutures.jpg” by Wikip2011 is licensed under CC BY-SA 3.0 ↵
- “Surgical staples1.jpg” by Llywrch is licensed under CC BY-SA 2.5 ↵
- “Incision wound on child's arm, closed with Dermabond.jpg” by ragesoss is licensed under CC BY-SA 3.0 ↵
- “Not quite scissors - TROML - 1366” by Clint Budd is licensed under CC BY 2.0 ↵
- Cox, J. (2019). Wound care 101. Nursing, 49(10). https://doi.org/10.1097/01.nurse.0000580632.58318.08 ↵
- Cox, J. (2019). Wound care 101. Nursing, 49(10). https://doi.org/10.1097/01.nurse.0000580632.58318.08 ↵
- Cox, J. (2019). Wound care 101. Nursing, 49(10). https://doi.org/10.1097/01.nurse.0000580632.58318.08 ↵
- “Úlceras_antes_da_cirurgia.JPG” by Nini00 is licensed under CC BY-SA 3.0 ↵
- Cox, J. (2019). Wound care 101. Nursing, 49(10). https://doi.org/10.1097/01.nurse.0000580632.58318.08 ↵
- “Arterial ulcer peripheral vascular disease.jpg” by Jonathan Moore is licensed under CC BY 3.0 ↵
- “Diabetic Planta ulcer.jpg” by Dr. Lorimer is licensed under CC BY-SA 4.0 ↵
- Cox, J. (2019). Wound care 101. Nursing, 49(10). https://doi.org/10.1097/01.nurse.0000580632.58318.08 ↵
- Edsberg, L. E., Black, J. M., Goldberg, M., McNichol, L., Moore, L., & Sieggreen, M. (2016). Revised National Pressure Ulcer Advisory Panel Pressure Injury Staging System: Revised pressure injury staging system. Journal of Wound, Ostomy, and Continence Nursing: Official Publication of The Wound, Ostomy and Continence Nurses Society, 43(6), 585–597. https://journals.lww.com/jwocnonline/Fulltext/2016/11000/Revised_National_Pressure_Ulcer_Advisory_Panel.3.aspx ↵
- The Braden Scale, from Prevention Plus, is included on the basis of Fair Use. ↵
- “Wound stage.jpg” by Babagolzadeh is licensed under CC BY-SA 3.0 ↵
- Edsberg, L. E., Black, J. M., Goldberg, M., McNichol, L., Moore, L., & Sieggreen, M. (2016). Revised National Pressure Ulcer Advisory Panel Pressure Injury Staging System: Revised pressure injury staging system. Journal of Wound, Ostomy, and Continence Nursing: Official Publication of The Wound, Ostomy and Continence Nurses Society, 43(6), 585–597. https://doi.org/10.1097/WON.0000000000000281 ↵
- Edsberg, L. E., Black, J. M., Goldberg, M., McNichol, L., Moore, L., & Sieggreen, M. (2016). Revised National Pressure Ulcer Advisory Panel Pressure Injury Staging System: Revised pressure injury staging system. Journal of Wound, Ostomy, and Continence Nursing: Official Publication of The Wound, Ostomy and Continence Nurses Society, 43(6), 585–597. https://doi.org/10.1097/WON.0000000000000281 ↵
- "Inoculation_eschar_Rickettsia_sibirica_mongolitimonae_infection.jpg" by José M. Ramos, Isabel Jado, Sergio Padilla, Mar Masiá, Pedro Anda, and Félix Gutiérrez is licensed under CC0 ↵
- Edsberg, L. E., Black, J. M., Goldberg, M., McNichol, L., Moore, L., & Sieggreen, M. (2016). Revised National Pressure Ulcer Advisory Panel Pressure Injury Staging System: Revised pressure injury staging system. Journal of Wound, Ostomy, and Continence Nursing: Official Publication of The Wound, Ostomy and Continence Nurses Society, 43(6), 585–597. https://doi.org/10.1097/WON.0000000000000281 ↵
- Edsberg, L. E., Black, J. M., Goldberg, M., McNichol, L., Moore, L., & Sieggreen, M. (2016). Revised National Pressure Ulcer Advisory Panel Pressure Injury Staging System: Revised pressure injury staging system. Journal of Wound, Ostomy, and Continence Nursing: Official Publication of The Wound, Ostomy and Continence Nurses Society, 43(6), 585–597. https://doi.org/10.1097/WON.0000000000000281 ↵
- RegisteredNurseRN. (2018, March 7). Pressure ulcers (injuries) stages, prevention, assessment | Stage 1, 2, 3, 4 unstageable NCLEX [Video]. YouTube. All rights reserved. Video used with permission. https://youtu.be/MDtPik1UE6k ↵
- Guo, S., & Dipietro, L. A. (2010). Factors affecting wound healing. Journal of Dental Research, 89(3), 219–229. https://doi.org/10.1177/0022034509359125 ↵
- Guo, S., & Dipietro, L. A. (2010). Factors affecting wound healing. Journal of Dental Research, 89(3), 219–229. https://doi.org/10.1177/0022034509359125 ↵
- Cox, J. (2019). Wound care 101. Nursing, 49(10). https://doi.org/10.1097/01.nurse.0000580632.58318.08 ↵
- Guo, S., & Dipietro, L. A. (2010). Factors affecting wound healing. Journal of Dental Research, 89(3), 219–229. https://doi.org/10.1177/0022034509359125 ↵
- Guo, S., & Dipietro, L. A. (2010). Factors affecting wound healing. Journal of Dental Research, 89(3), 219–229. https://doi.org/10.1177/0022034509359125 ↵
- Guo, S., & Dipietro, L. A. (2010). Factors affecting wound healing. Journal of Dental Research, 89(3), 219–229. https://doi.org/10.1177/0022034509359125 ↵
- Guo, S., & Dipietro, L. A. (2010). Factors affecting wound healing. Journal of Dental Research, 89(3), 219–229. https://doi.org/10.1177/0022034509359125 ↵
- Guo, S., & Dipietro, L. A. (2010). Factors affecting wound healing. Journal of Dental Research, 89(3), 219–229. https://doi.org/10.1177/0022034509359125 ↵
- Guo, S., & Dipietro, L. A. (2010). Factors affecting wound healing. Journal of Dental Research, 89(3), 219–229. https://doi.org/10.1177/0022034509359125 ↵
- Guo, S., & Dipietro, L. A. (2010). Factors affecting wound healing. Journal of Dental Research, 89(3), 219–229. https://doi.org/10.1177/0022034509359125 ↵
- Grey, J. E., Enoch, S., & Harding, K. G. (2006). Wound assessment. BMJ (Clinical research ed.), 332(7536), 285–288. https://doi.org/10.1136/bmj.332.7536.285 ↵
- Grey, J. E., Enoch, S., & Harding, K. G. (2006). Wound assessment. BMJ (Clinical research ed.), 332(7536), 285–288. https://doi.org/10.1136/bmj.332.7536.285 ↵
- This work is a derivative of StatPearls by Grubbs and Mannah is licensed under CC BY 4.0 ↵
- Edsberg, L. E., Black, J. M., Goldberg, M., McNichol, L., Moore, L., & Sieggreen, M. (2016). Revised National Pressure Ulcer Advisory Panel Pressure Injury Staging System: Revised pressure injury staging system. Journal of Wound, Ostomy, and Continence Nursing: Official Publication of The Wound, Ostomy and Continence Nurses Society, 43(6), 585–597. https://doi.org/10.1097/won.0000000000000281 ↵
- “Ankle swell and internal bleeding” by Glen Bowman is licensed under CC BY-SA 2.0 ↵
- WoundSource. (2016, October 19). 8 signs of wound infection. https://www.woundsource.com/blog/8-signs-wound-infection ↵
- WoundSource. (2018, March 28). Complications in chronic wound healing and associated interventions. https://www.woundsource.com/blog/complications-in-chronic-wound-healing-and-associated-interventions ↵
- “Bogota bag.png” by Suarez-Grau, J. M., Guadalajara Jurado, J. F., Gómez Menchero, J., Bellido Luque, J. A. is licensed under CC BY 4.0 ↵
- WoundSource. (2018, March 28). Complications in chronic wound healing and associated interventions. https://www.woundsource.com/blog/complications-in-chronic-wound-healing-and-associated-interventions ↵
- WoundSource. (2018, March 28). Complications in chronic wound healing and associated interventions. https://www.woundsource.com/blog/complications-in-chronic-wound-healing-and-associated-interventions ↵
Vomiting of blood.
Passage of bloody stool.
The very thin, top layer of the skin that contains openings of the sweat gland ducts and the visible part of hair known as the hair shaft.
Nurses access patients' veins to collect blood (i.e., perform phlebotomy) and to administer intravenous (IV) therapy. This section will describe several methods for collecting blood, as well as review the basic concepts of IV therapy.
Blood Collection
Nurses collect blood samples from patients using several methods, including venipuncture, capillary blood sampling, and blood draws from venous access devices. Blood may also be drawn from arteries by specially trained professionals for certain laboratory testing.
Venipuncture
Venipuncture involves the process of introducing a needle into a patient’s vein to collect a blood sample or insert an IV catheter. See Figure 23.1[1] for an image of venipuncture. Blood sampling with venipuncture may be initiated by nurses, phlebotomists, or other trained personnel. Venipuncture for collection of a blood sample is an important part of data collection to assess a patient’s health status. It is commonly performed to examine hematologic and immune issues such as the body’s oxygen-carrying capacity, infection, and clotting function. It is also useful for assessing metabolic and nutrition issues such as electrolyte status and kidney functioning.
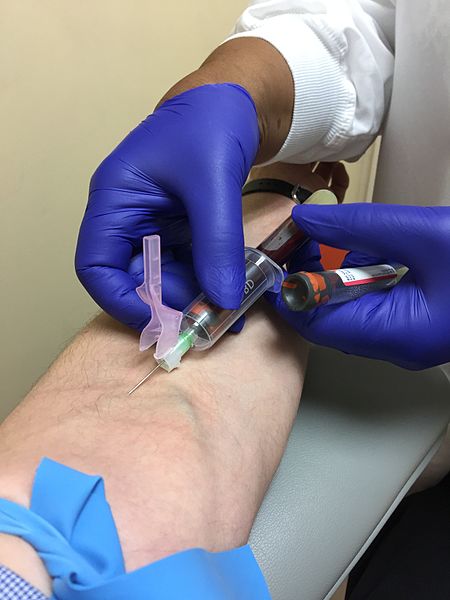
Blood collection is commonly performed via venipuncture from veins in the arms or hands. The most common sites for venipuncture are the large veins located on the antecubital fossa (i.e., the inner side of the elbow). These veins are often preferred for venipuncture because their larger size increases their ability to withstand repetitive blood sampling. However, these veins are not preferred for intravenous therapy due to the mechanical obstruction that can occur in the IV catheter when the elbow joint is contracted.
To perform the skill of venipuncture, the nurse performs many similar steps that occur with IV cannulation. The process of venipuncture for blood sample collection is outlined in the Open RN Nursing Advanced Skills "Perform Venipuncture Blood Draw" checklist.
Blood Samples From Central Venous Access Devices
Blood may also be collected by nurses from a patient's existing central venous access device (CVAD). A CVAD is a type of vascular access that involves the insertion of a catheter into a large vein in the arm, neck, chest, or groin.[2]
CVADs are discussed in more detail in the Open RN Nursing Advanced Skills "Manage Central Lines" chapter that also contains the "Obtain a Blood Sample From a CVAD" checklist.
Capillary Blood Sampling
Nurses also collect small amounts of blood for testing via capillary blood sampling. Capillary blood testing occurs when blood is collected from capillaries located near the surface of the skin. Capillaries in the fingers are used for testing in adults whereas capillaries in the heels are used for infants. An example of capillary blood testing is bedside glucose testing. See Figure 23.2[3] for an image of capillary blood glucose testing.
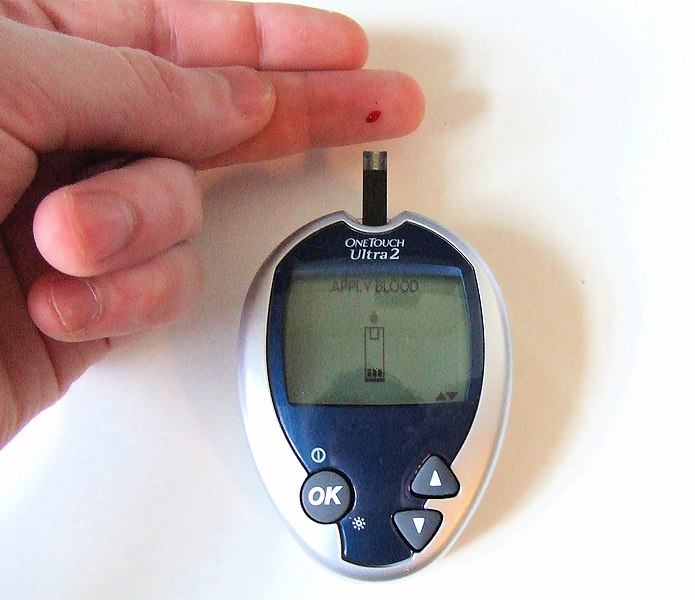
Capillary blood testing is typically used when repetitive sampling is needed. However, not all blood tests can be performed on capillary blood, and some clinical conditions make capillary blood testing inappropriate, such as when a patient is hypotensive with limited venous return.
Review how to perform capillary blood glucose testing in the "Blood Glucose Monitoring" section of the "Specimen Collection" chapter of Open RN Nursing Skills.
Arterial Blood Sampling
Arterial blood sampling occurs when blood is obtained via puncture into an artery by specially trained registered nurses and other health care personnel, such as respiratory therapists, physicians, nurse practitioners, and physician assistants. Arterial blood collection is most commonly performed to assess the body’s acid-base balance in a diagnostic test called an arterial blood gas. (For more information on arterial blood gas interpretation, please review Open RN Nursing Fundamentals Chapter 15). The most common access site for arterial blood sampling is the radial artery. See Figure 23.3[4] for an image of arterial blood sampling. Arterial blood tests are known to be more painful for the patient than venipuncture and have a higher risk of complications such as bleeding and arterial occlusion with subsequent ischemia to the area distal to the puncture.
Arterial Lines
For patients who require repetitive arterial blood sampling or are hemodynamically unstable, an arterial line may be inserted by specially trained personnel. Arterial lines are specialized tubes that are inserted and maintained in an artery to assist with continuous blood pressure monitoring. They also allow for repeated blood sampling without repetitive puncture, thus decreasing the amount of discomfort for the patient. The radial artery is the most common site used for arterial lines. Nurses must not confuse arterial lines with peripheral or central vein access devices. Arterial lines can be distinguished from venous lines by their specialized pressure tubing, which is firm and non-pliable and is connected to a pressure bag to maintain constant pressurized fluid in the tubing. Medications, fluid boluses, and maintenance IV fluids must never be infused through an arterial line. See Figure 23.3[5] for an image of arterial lines. The condition of the arterial access site, as well as perfusion of the patient's hand, is continually monitored when an arterial line is in place to prevent complications.

Intravenous Therapy
In addition to collecting blood samples, nurses also access patients' veins to administer intravenous therapy.Intravenous therapy (IV therapy) involves the administration of substances such as fluids, electrolytes, blood products, nutrition, or medications directly into a patient's vein. The intravenous route is preferred to administer fluids and medications when rapid onset of the medication or fluid is needed. The direct administration of medication into the bloodstream allows for a more rapid onset of medication actions, restoration of hydration, and correction of nutritional deficits. IV therapy is often used to restore fluids and/or resolve electrolyte imbalances more efficiently than what would be achieved via the oral route.
Fluid Balance
Fluid balance is an important part of optimal cellular functioning, and administration of fluids via the venous system provides an efficient way to quickly correct fluid imbalances. Additionally, many individuals who are physically unwell may not be able to tolerate fluids administered through their gastrointestinal tract, so IV administration is necessary. When administering IV therapy, the nurse needs to understand the nature of the solution being administered and how it will affect the patient's condition.
When patients experience deficient fluid volume, intravenous (IV) fluids are often used to restore fluid to the intravascular compartment or to facilitate the movement of fluid between compartments through the process of osmosis. There are three types of IV fluids: isotonic, hypotonic, and hypertonic.[6]
Review movement of fluid between compartments of the body in the "Basic Fluid and Electrolyte Concepts" section of the "Fluids and Electrolytes" chapter in Open RN Nursing Fundamentals.
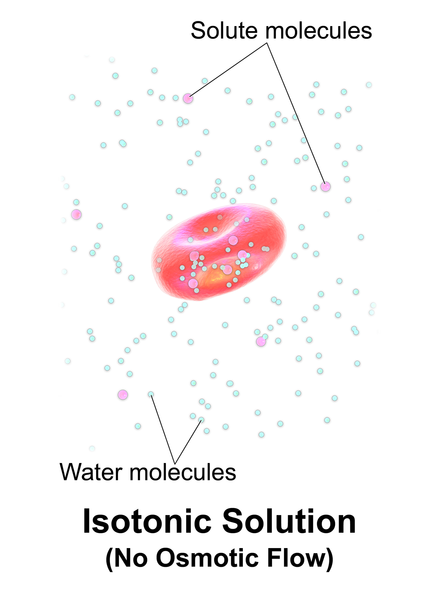
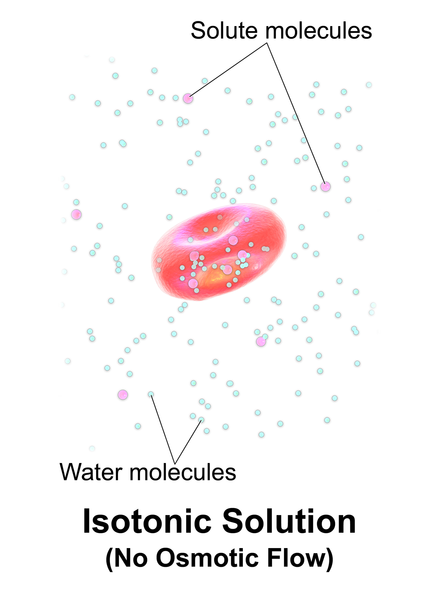
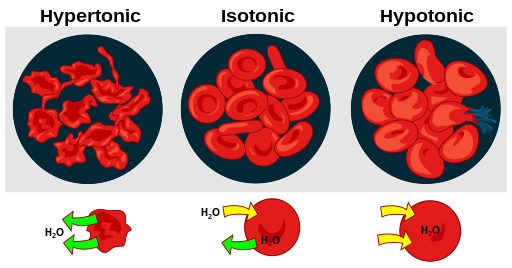
Isotonic Solutions
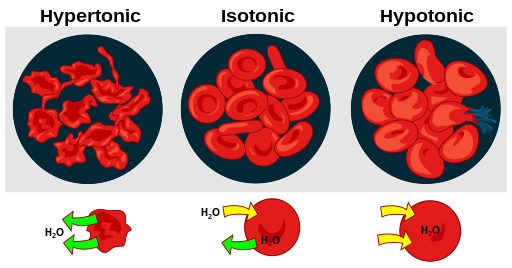
Isotonic solutions are IV fluids that have a similar concentration of dissolved particles as found in the blood. Examples of isotonic IV solutions are 0.9% normal saline (0.9% NaCl) or lactated ringers (LR). Because the concentration of isotonic IV fluid is similar to the concentration of blood, the fluid stays in the intravascular space, and osmosis does not cause fluid movement between cells. See Figure 23.4[7] for an illustration of isotonic IV solution administration that does not cause osmotic movement of fluid.
Isotonic solutions are used to treat fluid volume deficit (also called hypovolemia) to replace extracellular fluid that has been lost due to bleeding, dehydration, shock, burns, trauma, and gastrointestinal tract fluid loss (such as diarrhea). IV therapy with isotonic fluids will increase a patient's blood pressure. However, infusion of too much isotonic fluid can cause excessive fluid volume (also referred to as hypervolemia) and must be used with caution in patients with hypertension, heart failure, and renal disease due to the potential for fluid overload.[8]
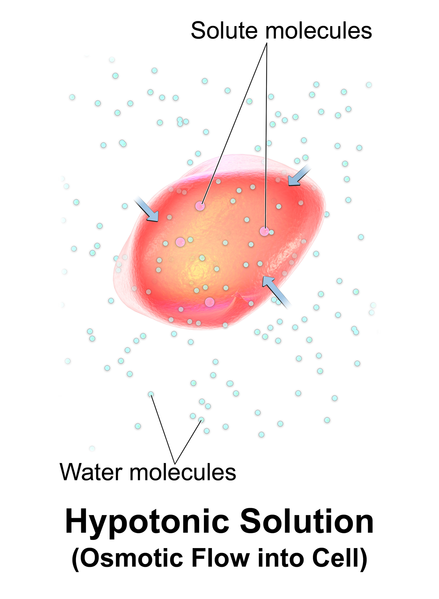
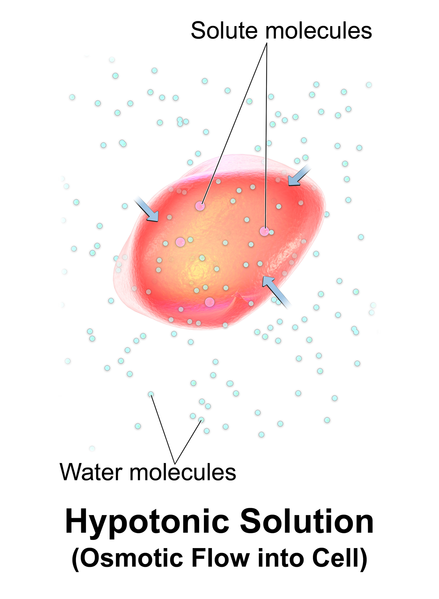
Hypotonic Solutions
Hypotonic solutions have a lower concentration of dissolved solutes than blood. An example of a hypotonic IV solution is 0.45% normal saline (0.45% NaCl). Another example of hypotonic fluid is dextrose 5% in water (D5W). D5W is isotonic in the bag but becomes hypotonic after the dextrose is rapidly metabolized by the body.
When hypotonic IV solutions are infused, it results in a decreased concentration of dissolved solutes in the blood as compared to the intracellular space. This imbalance causes osmotic movement of water from the intravascular compartment into the intracellular space. For this reason, hypotonic fluids are used to treat cellular dehydration. See Figure 23.5[9] for an illustration of the osmotic movement of fluid into a cell when a hypotonic IV solution is administered, causing lower concentration of solutes (pink molecules) in the bloodstream compared to within the cell.[10]
Hypotonic solutions are used for patients whose cells have become dehydrated, such as during diabetic ketoacidosis (DKA) or hyperosmolar hyperglycemia, and fluids must be pushed back into the cells. However, if too much fluid moves out of the intravascular compartment into the cells, cerebral edema, worsening hypovolemia, and hypotension can occur. Therefore, patient status should be monitored carefully when hypotonic solutions are infused.[11]
Hypertonic Solutions
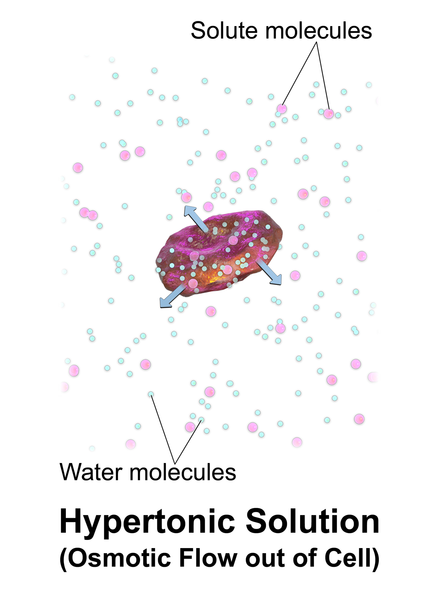
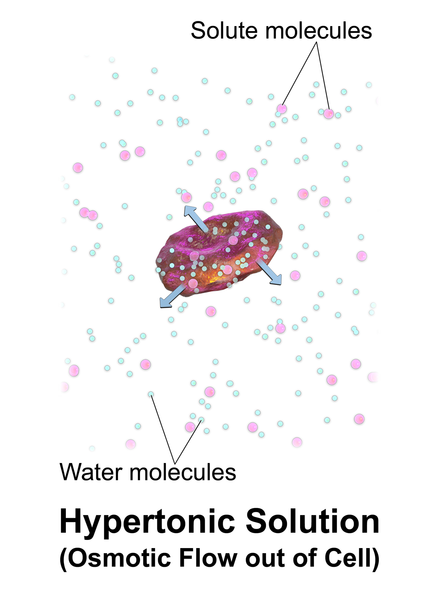
Hypertonic solutions have a higher concentration of dissolved particles than blood. An example of hypertonic IV solution is 3% normal saline (3% NaCl). When infused, hypertonic fluids cause an increased concentration of dissolved solutes in the intravascular space compared to the cells. This causes the osmotic movement of water out of the cells and into the intravascular space to dilute the solutes in the blood. See Figure 23.6[12] for an illustration of osmotic movement of fluid out of a cell when hypertonic IV fluid is administered due to a higher concentration of solutes (pink molecules) in the bloodstream compared to the cell.
Hypertonic solutions move water out of the cells of the body and into the bloodstream. They are commonly used for patients with cerebral edema, severe hyponatremia, or some types of post-op patients. Hypertonic solutions must be used very cautiously due to potentially rapid side effects of fluid overload resulting in pulmonary edema, so they are typically administered in intensive care units (ICU). Hypertonic fluids should not be administered to patients with DKA because it will worsen their cellular dehydration.
When administering hypertonic fluids, it is essential to monitor for signs of fluid overload, such as significantly elevated blood pressure and difficulties breathing. Additionally, if hypertonic solutions with sodium are given, the patient's serum sodium level should be closely monitored.[13]
See Figure 23.7[14] for an illustration comparing how different types of IV solutions affect red blood cell size.
IV fluids are considered medications. As with all medications, nurses must check the rights of medication administration according to agency policy before administering IV fluids. What began as five rights of medication administration has been extended to eight rights according to the American Nurses Association. These eight rights include the following[15]:
- Right Patient
- Right Medication
- Right Dose
- Right Time
- Right Route
- Right Documentation
- Right Reason
- Right Response
Nurses also check for patient allergies, expiration date of the fluid, and compatibility of the fluid with any other fluids, medications, or blood products being administered intravenously. With any IV infusion, it is important for the nurse to pay close attention to the provider's order and make sure that it contains the specific type of fluid, any additives or medications, amount to be infused, rate of infusion, and the length of time that the therapy should continue. The nurse should also carefully assess a patient's hydration status and oral intake to ensure that IV fluids are stopped appropriately as a patent's condition changes. For example, weight should be assessed daily for patients receiving IV fluids to monitor for fluid overload.
Review how to check the rights of medication administration in the “Administration of Enteral Medications” chapter of Open RN Nursing Skills.
Electrolyte Imbalance
In addition to rapidly improving hydration status, IV fluids may also be administered to rapidly correct electrolyte imbalances. Infusing fluids with electrolytes such as potassium, calcium, and magnesium can correct electrolyte imbalances more rapidly and effectively than by oral supplementation. However, nurses must collaborate with the interprofessional team to identify medications that should and should not be given through peripheral veins. Current standards of care consider continuous peripheral infusion therapy of electrolytes to be inappropriate because of potential vascular endothelial damage. Ideally, peripheral IV therapy should be isotonic and consistent with physiological pH; otherwise, central venous access should be used.[16]
Electrolytes administered via the IV route must always be administered cautiously at the correct infusion rate because over supplementation can be deadly. For example, potassium infusions administered too rapidly into a patient's system can cause sudden cardiac arrest.
Blood Administration
Blood and blood components are administered by registered nurses via IV infusion, typically through larger sized IV catheters. Blood and blood components are transfused through a special transfusion administration set that has a filter designed to retain potentially harmful particles. Specific procedures for verifying the correct patient and correct blood product are performed prior to transfusion to prevent transfusion reactions that can be life-threatening. Administration of blood and blood components, including the use of infusion devices and ancillary equipment, and the identification, evaluation, and reporting of adverse events related to transfusion are established in agency policies, procedures, and/or practice guidelines. Read more information about blood administration in the "Administer Blood Products" chapter in Open RN Nursing Advanced Skills.
Nutrition
Nutritional therapy can be administered through an intravenous route for patients who do not have an adequately functioning gastrointestinal tract and/or are unable to take in food or fluids appropriately. Peripheral nutrition may be ordered through a peripheral IV site for nutritional needs such as albumin replacement.
Total parenteral nutrition (TPN) may be ordered for a patient based on their specific electrolyte and/or nutritional needs. TPN is a very concentrated solution that must be administered via a central line. Central lines are placed in a larger vessel rather than a smaller, peripheral vessel. Accessing a central vessel requires additional training and expertise to prevent complications with insertion and is further discussed in the Open RN Nursing Advanced Skills "Manage Central Lines” chapter. If a nurse receives an order for TPN therapy for a patient who does not have central line access, the order should be clarified with the prescribing provider.
Medications
The IV route is preferred for the administration of many medications when immediate onset is required. For example, many types of pain medications can be given directly into the bloodstream with a much more rapid onset of action than if they were to be administered orally. Rapid relief of pain can be achieved in minutes rather than hours required for oral medications to reach their peak. Rapid onset can also be achieved with other medications such as those used to treat cardiac emergencies or severe allergic reactions to quickly restore patients to optimal body functioning. Additional information about IV administration of medications is discussed in the Open RN Nursing Advanced Skills "Administer IV Push Medications” chapter.
IV Administration Equipment
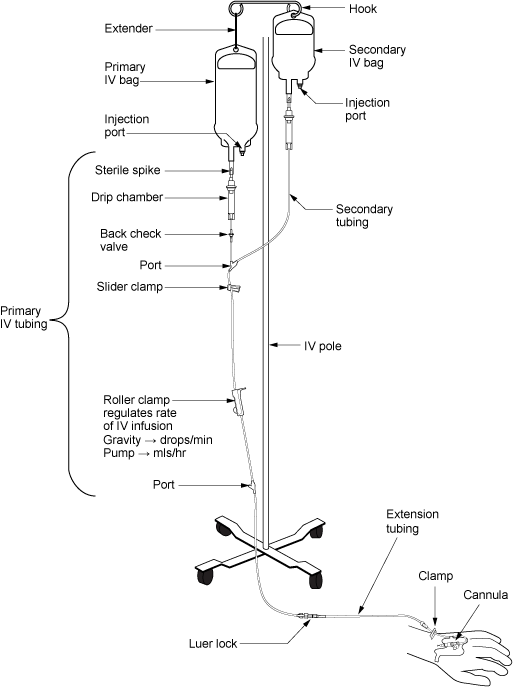
Intravenous (IV) substances are administered through flexible plastic tubing called an IV administration set. The IV administration set connects the bag of solution to the patient’s IV access site. There are two major types of IV administration sets: primary administration sets and secondary administration sets. Administration sets require routine replacement to prevent infection. Follow agency policy regarding tubing changes before initiating a new bag of fluid or medications. See a summary of general guidelines for IV therapy and administration equipment in the box at the end of this section.
Primary Administration Sets
Primary administration sets can be used to infuse continuous or intermittent fluids, electrolytes, or medications. These substances may be administered by infusion pump or by gravity, and each method requires its own type of administration set.
Primary fluids are typically administered using an IV pump. An IV pump is the safest method of administration to ensure specific amounts of fluid are administered. The rate of infusion through an IV pump is typically calculated in mL/hour.
For infusion by gravity, a primary IV administration set can be a macro-drip or a micro-drip solution set. Macro-drip sets are used for routine primary infusions for adults. Micro-drip IV tubing is used in pediatric or neonatal care where small amounts of fluids are administered over a long period of time. A macro-drip infusion set delivers fluid at 10, 15, or 20 drops per milliliter, whereas a micro-drip infusion set delivers 60 drops per milliliter. The drop factor is located on the packaging of the IV tubing and is important to verify when calculating medication administration rates.
Primary IV administration sets consist of the following parts:
- Sterile spike: Used to spike the IV fluid bag and must be kept sterile.
- Roller clamp: Used to regulate the speed or stop an infusion by gravity.
- Drip chamber: Allows air to rise out from a fluid so that it is not passed onto the patient. The drip chamber should be kept ¼ to ½ full of solution. When setting a rate by gravity to "drops per minute," the dripping from this chamber is counted.
- Backcheck valve: Prevents fluid or medication from travelling up into the primary IV bag.
- Access ports: Used to infuse secondary medications and to administer IV push medications. These may also be referred to as “Y ports.”
Secondary Administration Sets
Secondary IV administration sets are used to intermittently administer a secondary medication, such as an antibiotic, while the primary IV is also running. Secondary IV tubing is shorter in length than primary tubing and is connected to a primary line via an access port above the infusion pump. The infusion pump is then set at the prescribed secondary infusion rate while the secondary medication is administered. By hanging the secondary medication bag higher than the primary bag, gravity pulls fluid from the secondary bag until it is empty rather than the primary bag.
Secondary medications may be “piggybacked” into primary infusion lines so the solution from the primary fluid line can be used to prime the secondary tubing. To prime the secondary tubing, after the secondary tubing is connected to the primary tubing, the bag connected to the secondary tubing is held lower than the primary bag, causing fluid from the primary tubing to backflow up the secondary tubing. This eliminates air from the secondary tubing.
See Figure 23.8[17] for an illustration of the setup of primary and secondary administration sets for primary administration of fluids and secondary administration of medication by gravity. See Figure 23.9[18] for an image of an IV infusion pump.

Priming IV Tubing
Primary administration sets, secondary administration sets, and extension tubing must be primed with IV solution to prevent air from entering the patient's circulatory system and causing an air embolism. Priming refers to the process of filling the IV tubing with IV solution prior to attaching it to the patient. Review steps for setting up and priming primary and secondary administration sets using the information in the following box.
Review checklists of steps for "Primary IV Solution Administration" and "Secondary IV Solution Administration" in the "IV Therapy Management" chapter of Open RN Nursing Skills.
Infection Control
Aseptic technique must be maintained throughout all IV therapy procedures, including initiation of IV access, preparing and maintaining IV equipment, administering IV fluids and medications, and discontinuing an IV system. Hand hygiene and strict aseptic technique must be performed when handling all IV equipment. These standards can be reviewed in the “Aseptic Technique” chapter. Additionally, if an IV catheter or IV administration set should become contaminated by contact with a nonsterile surface, it should be replaced with a new one to prevent introducing bacteria or other contaminants into the system.
Types of Venous Access
There are several types of venous access devices used to administer IV therapy that are categorized as peripheral devices or central devices. Venous access device selection is tailored to each patient's needs and to the type, duration, and frequency of infusion.
Peripheral Devices
Peripheral venous access devices are commonly used for short-term IV therapy in the hospital setting. A peripheral IV is an intravenous catheter inserted by percutaneous venipuncture into a peripheral vein and held in place with a sterile transparent dressing. The transparent dressing helps to keep the site sterile, prevents accidental dislodgement, and allows the nurse to visualize the insertion site through the dressing. A securement device may be added to prevent accidental dislodgement.
The patient’s upper extremities (hands and arms) are the preferred sites for insertion. However, a potential limitation of using the hand veins is they are smaller than the cephalic, basilic, or brachial veins in the arm. If the patient requires rapid infusions where a larger gauge IV is warranted, the larger veins in the upper arm should be considered.
Peripheral IVs are used for short-term infusions of fluids, medications, or blood. Peripheral IVs are easy to monitor and can be inserted at the bedside by nurses and other trained professionals. After IV access has been obtained, the hub of an intravenous catheter is attached to a short extension set or a primary IV administration set. Luer lock connectors on the extension tubing and/or administration sets permit syringes to be attached to administer medications or fluid flushes.
Saline lock refers to the use of a short extension set that allows IV access without requiring ongoing IV infusions. When not in use, the lock is flushed with saline according to agency policy and clamped to ensure the site remains sterile and blood does not flow out of the extension tubing. See Figure 23.10[19] for an image of a saline lock.

If the patient requires continuous infusion of IV fluids, the extension tubing from the IV catheter is connected to a primary IV administration set. The IV tubing can be run through an infusion pump to administer fluids or medications at a programmed rate of infusion (typically calculated in mL/hour) or via gravity by setting a drip rate with the roller clamp (typically calculated at drops/minute). Manufacturers list the drop rate on the IV packaging. Because of the risk of error that can occur with infusion by gravity, many agencies require the use of an infusion pump to ensure correct flow rate.
Contraindications to Peripheral IV Access Sites
Before inserting a peripheral IV, the patient should be assessed for contraindications related to insertion sites in the upper extremities. For example, patients who have a history of lumpectomy or mastectomy, an arteriovenous fistula, or current lymphedema often have restrictions that prohibit venipuncture into the affected extremity.[20] Additionally, deep vein thrombosis (DVT), fractures, contractures, or extensive scarring may also prohibit the placement of a peripheral IV. Hospitalized patients may have signage or a bracelet stating "limb alert" to alert heath care professionals to these conditions.
Midline Peripheral Catheters
Midline peripheral catheters have a larger catheter (i.e., 16-18 gauge) that allows for rapid infusions. Insertion is ultrasound-guided and can be inserted by RNs with additional training or other trained professionals. Midline catheters are typically inserted into the basilic, cephalic, or brachial veins of the upper arm with the tip placed near the level of the axilla. They are much longer and inserted deeper than a peripheral IV, but do not extend into a central vessel, so they are not considered a central line. Therefore, they have a lower risk of infection than central venous access. Any medication that can be administered through a peripheral line can be administered via a midline peripheral catheter. They can also be used for longer duration than traditional peripheral venous access, which is ideal for patients needing extended hospital stays or IV access. Based on agency policy, midline catheters may also be used for blood sample collection, thus limiting the number of venipunctures a patient receives. Site care for a midline peripheral catheter is similar to a peripheral IV dressing change.[21],[22]
Central Venous Access Devices
A central venous access device (CVAD) is a type of vascular access established by specially trained registered nurses and other health care personnel. It involves the insertion of a tube into a vein in the neck, chest, or groin and threaded into a central vein (most commonly the internal jugular, subclavian, or femoral) and advanced until the tip of the catheter resides within the inferior vena cava, superior vena cava, or right atrium.[23] Only specially trained health professionals may insert central venous access devices, but nurses provide routine care of CVADs, including dressing changes. See Figure 23.11[24] for an image of a central line requiring a dressing change.
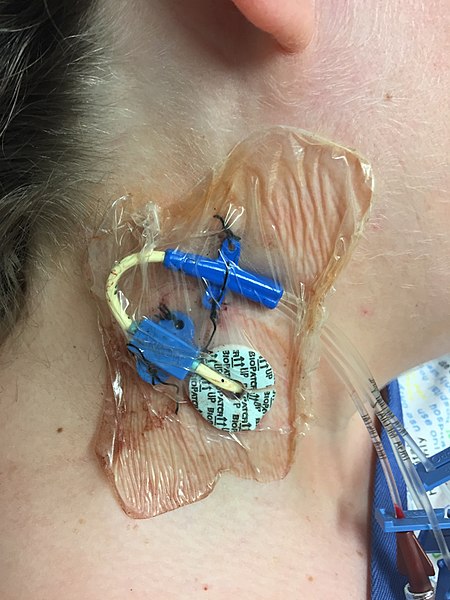
A central venous access device can be left in for longer periods of time and is useful for administering concentrated medications and fluids, such as TPN or hyperosmotic fluids, that would be otherwise irritating to smaller peripheral veins. However, central venous access devices have an increased risk for the development of bloodstream infections, so strict sterile technique is required during insertion, and aseptic technique is used for maintenance. Central venous access devices are further discussed in the "Manage Central Lines" chapter of Open RN Nursing Advanced Skills.
Peripheral Inserted Central Catheters
A peripheral inserted central catheter (PICC) is a thin, flexible tube inserted into a vein in the upper arm and guided into the superior vena cava. It is used to give intravenous fluids, blood transfusions, chemotherapy, and other medications requiring a central line. It can also be used for blood sampling. A PICC may stay in place for weeks or months and helps avoid the need for repeated needlesticks. PICC lines are further discussed in the "Manage Central Lines" chapter of Open RN Nursing Advanced Skills.
General Guidelines for IV Therapy
The following are general guidelines for peripheral IV therapy[25]:
- IV fluid therapy is ordered by a provider. The order must include the type of solution or medication, total amount of fluid, rate of infusion, duration, date, and time.
- IV therapy is an invasive procedure. Significant complications can occur if the wrong amount of IV fluids or incorrect medication is given or if aseptic technique is not strictly followed.
- Nurses must understand the indications and duration for IV therapy for each patient. Practice guidelines recommend that patients receiving IV therapy for more than six days should be assessed for an intermediate or long-term device such as a central venous access device (CVAD).
- Hospitalized patients may have an order for a small hourly infusion rate, such as 10-20 mL/hour, historically referred to in practice as a "to keep open" (TKO) or "keep vein open" (KVO) rate.
- IV administration sets require routine replacement to promote patient safety and reduce the risk of infection. Primary and secondary continuous administration sets used to administer solutions other than lipids, blood, or blood products are typically changed every 96 hours, or up to every 7 days, as directed by agency policy and/or the manufacturer’s instructions. Administration sets should also be changed if contamination or compromise in the integrity of the product or system is suspected. Secondary administration sets that are detached from a primary administration set are typically changed every 24 hours or as directed by agency policy. Administration sets should be labelled according to agency policy with the date of initiation or the date of change indicated.[26]
Increased peristaltic activity; may be related to diarrhea, obstruction, or digestion of a meal.
Decreased peristaltic activity; may be related to constipation, following abdominal surgery, or with an ileus.
Hyperperistalsis, often referred to as “stomach growling”.
An expansion of the abdomen caused by the accumulation of air or fluid. Patients often report “feeling bloated”.
Sunken appearance.
Convex or bulging appearance.
Involuntary leakage of urine.
The phase of the heartbeat when the left ventricle contracts and pumps blood into the arteries.
The maximum pressure of blood on the arteries during the contraction of the left ventricle of the heart referred to as systole.
White or silver markings from stretching of the skin.
Pain when hand is withdrawn during palpation.
Involuntary contraction of the abdominal musculature in response to peritoneal inflammation.
Voluntary contraction of abdominal wall musculature; may be related to fear, anxiety or presence of cold hands.
A decrease in blood pressure by at least 20mmHg systolic or 10mmHg diastolic within three minutes of standing from a seated or lying position.
Decreased blood pressure less than 90/60 mmHg in an adult.
The audible sounds of blood pressure named after Dr. Korotkoff who discovered them.
The phase between each contraction of the heart when the ventricles are filling with blood.
Bicarbonate level reflected in arterial blood gas results. Normal range is 22-26 meq/L.
A sample of arterial blood that measures the oxygen, carbon dioxide, and bicarbonate levels.
An estimated oxygenation level based on the saturation level of hemoglobin measured by a pulse oximeter.
Also referred to as “rales”; sound like popping or crackling noises during inspiration. Associated with inflammation and fluid accumulation in the alveoli.
Fraction of inspired oxygen (i.e. the concentration of oxygen inhaled). Room air contains 21% oxygen levels, and oxygenation devices can increase the inhaled concentration of oxygen up to 100%. However, FiO2 levels should be decreased as soon as feasible to do so to prevent lung injury.
OSA is characterized by repeated occurrences of complete or partial obstructions of the upper airway during sleep, resulting in apneic episodes.
A surgically created opening that goes from the front of the neck into the trachea.
Type of tracheostomy tube that contains holes so the patient can speak if the cuff is deflated and the inner cannula is removed.
The end of the tracheostomy tube that is placed securely against the patient’s neck.
OSA is characterized by repeated occurrences of complete or partial obstructions of the upper airway during sleep, resulting in apneic episodes.
Nurses access patients' veins to collect blood (i.e., perform phlebotomy) and to administer intravenous (IV) therapy. This section will describe several methods for collecting blood, as well as review the basic concepts of IV therapy.
Blood Collection
Nurses collect blood samples from patients using several methods, including venipuncture, capillary blood sampling, and blood draws from venous access devices. Blood may also be drawn from arteries by specially trained professionals for certain laboratory testing.
Venipuncture
Venipuncture involves the process of introducing a needle into a patient’s vein to collect a blood sample or insert an IV catheter. See Figure 23.1[27] for an image of venipuncture. Blood sampling with venipuncture may be initiated by nurses, phlebotomists, or other trained personnel. Venipuncture for collection of a blood sample is an important part of data collection to assess a patient’s health status. It is commonly performed to examine hematologic and immune issues such as the body’s oxygen-carrying capacity, infection, and clotting function. It is also useful for assessing metabolic and nutrition issues such as electrolyte status and kidney functioning.
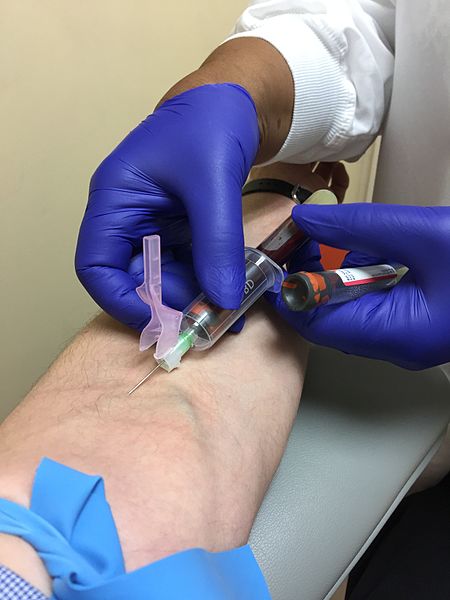
Blood collection is commonly performed via venipuncture from veins in the arms or hands. The most common sites for venipuncture are the large veins located on the antecubital fossa (i.e., the inner side of the elbow). These veins are often preferred for venipuncture because their larger size increases their ability to withstand repetitive blood sampling. However, these veins are not preferred for intravenous therapy due to the mechanical obstruction that can occur in the IV catheter when the elbow joint is contracted.
To perform the skill of venipuncture, the nurse performs many similar steps that occur with IV cannulation. The process of venipuncture for blood sample collection is outlined in the Open RN Nursing Advanced Skills "Perform Venipuncture Blood Draw" checklist.
Blood Samples From Central Venous Access Devices
Blood may also be collected by nurses from a patient's existing central venous access device (CVAD). A CVAD is a type of vascular access that involves the insertion of a catheter into a large vein in the arm, neck, chest, or groin.[28]
CVADs are discussed in more detail in the Open RN Nursing Advanced Skills "Manage Central Lines" chapter that also contains the "Obtain a Blood Sample From a CVAD" checklist.
Capillary Blood Sampling
Nurses also collect small amounts of blood for testing via capillary blood sampling. Capillary blood testing occurs when blood is collected from capillaries located near the surface of the skin. Capillaries in the fingers are used for testing in adults whereas capillaries in the heels are used for infants. An example of capillary blood testing is bedside glucose testing. See Figure 23.2[29] for an image of capillary blood glucose testing.
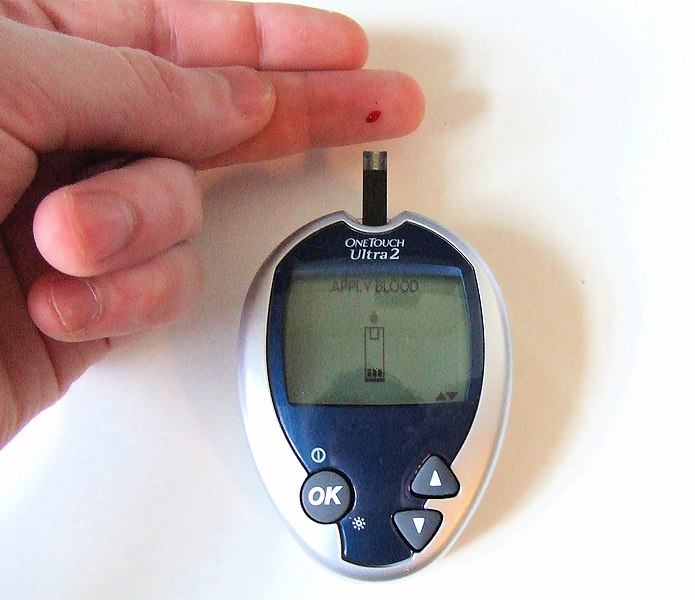
Capillary blood testing is typically used when repetitive sampling is needed. However, not all blood tests can be performed on capillary blood, and some clinical conditions make capillary blood testing inappropriate, such as when a patient is hypotensive with limited venous return.
Review how to perform capillary blood glucose testing in the "Blood Glucose Monitoring" section of the "Specimen Collection" chapter of Open RN Nursing Skills.
Arterial Blood Sampling
Arterial blood sampling occurs when blood is obtained via puncture into an artery by specially trained registered nurses and other health care personnel, such as respiratory therapists, physicians, nurse practitioners, and physician assistants. Arterial blood collection is most commonly performed to assess the body’s acid-base balance in a diagnostic test called an arterial blood gas. (For more information on arterial blood gas interpretation, please review Open RN Nursing Fundamentals Chapter 15). The most common access site for arterial blood sampling is the radial artery. See Figure 23.3[30] for an image of arterial blood sampling. Arterial blood tests are known to be more painful for the patient than venipuncture and have a higher risk of complications such as bleeding and arterial occlusion with subsequent ischemia to the area distal to the puncture.
Arterial Lines
For patients who require repetitive arterial blood sampling or are hemodynamically unstable, an arterial line may be inserted by specially trained personnel. Arterial lines are specialized tubes that are inserted and maintained in an artery to assist with continuous blood pressure monitoring. They also allow for repeated blood sampling without repetitive puncture, thus decreasing the amount of discomfort for the patient. The radial artery is the most common site used for arterial lines. Nurses must not confuse arterial lines with peripheral or central vein access devices. Arterial lines can be distinguished from venous lines by their specialized pressure tubing, which is firm and non-pliable and is connected to a pressure bag to maintain constant pressurized fluid in the tubing. Medications, fluid boluses, and maintenance IV fluids must never be infused through an arterial line. See Figure 23.3[31] for an image of arterial lines. The condition of the arterial access site, as well as perfusion of the patient's hand, is continually monitored when an arterial line is in place to prevent complications.

Intravenous Therapy
In addition to collecting blood samples, nurses also access patients' veins to administer intravenous therapy.Intravenous therapy (IV therapy) involves the administration of substances such as fluids, electrolytes, blood products, nutrition, or medications directly into a patient's vein. The intravenous route is preferred to administer fluids and medications when rapid onset of the medication or fluid is needed. The direct administration of medication into the bloodstream allows for a more rapid onset of medication actions, restoration of hydration, and correction of nutritional deficits. IV therapy is often used to restore fluids and/or resolve electrolyte imbalances more efficiently than what would be achieved via the oral route.
Fluid Balance
Fluid balance is an important part of optimal cellular functioning, and administration of fluids via the venous system provides an efficient way to quickly correct fluid imbalances. Additionally, many individuals who are physically unwell may not be able to tolerate fluids administered through their gastrointestinal tract, so IV administration is necessary. When administering IV therapy, the nurse needs to understand the nature of the solution being administered and how it will affect the patient's condition.
When patients experience deficient fluid volume, intravenous (IV) fluids are often used to restore fluid to the intravascular compartment or to facilitate the movement of fluid between compartments through the process of osmosis. There are three types of IV fluids: isotonic, hypotonic, and hypertonic.[32]
Review movement of fluid between compartments of the body in the "Basic Fluid and Electrolyte Concepts" section of the "Fluids and Electrolytes" chapter in Open RN Nursing Fundamentals.
Isotonic Solutions
Isotonic solutions are IV fluids that have a similar concentration of dissolved particles as found in the blood. Examples of isotonic IV solutions are 0.9% normal saline (0.9% NaCl) or lactated ringers (LR). Because the concentration of isotonic IV fluid is similar to the concentration of blood, the fluid stays in the intravascular space, and osmosis does not cause fluid movement between cells. See Figure 23.4[33] for an illustration of isotonic IV solution administration that does not cause osmotic movement of fluid.
Isotonic solutions are used to treat fluid volume deficit (also called hypovolemia) to replace extracellular fluid that has been lost due to bleeding, dehydration, shock, burns, trauma, and gastrointestinal tract fluid loss (such as diarrhea). IV therapy with isotonic fluids will increase a patient's blood pressure. However, infusion of too much isotonic fluid can cause excessive fluid volume (also referred to as hypervolemia) and must be used with caution in patients with hypertension, heart failure, and renal disease due to the potential for fluid overload.[34]
Hypotonic Solutions
Hypotonic solutions have a lower concentration of dissolved solutes than blood. An example of a hypotonic IV solution is 0.45% normal saline (0.45% NaCl). Another example of hypotonic fluid is dextrose 5% in water (D5W). D5W is isotonic in the bag but becomes hypotonic after the dextrose is rapidly metabolized by the body.
When hypotonic IV solutions are infused, it results in a decreased concentration of dissolved solutes in the blood as compared to the intracellular space. This imbalance causes osmotic movement of water from the intravascular compartment into the intracellular space. For this reason, hypotonic fluids are used to treat cellular dehydration. See Figure 23.5[35] for an illustration of the osmotic movement of fluid into a cell when a hypotonic IV solution is administered, causing lower concentration of solutes (pink molecules) in the bloodstream compared to within the cell.[36]
Hypotonic solutions are used for patients whose cells have become dehydrated, such as during diabetic ketoacidosis (DKA) or hyperosmolar hyperglycemia, and fluids must be pushed back into the cells. However, if too much fluid moves out of the intravascular compartment into the cells, cerebral edema, worsening hypovolemia, and hypotension can occur. Therefore, patient status should be monitored carefully when hypotonic solutions are infused.[37]
Hypertonic Solutions
Hypertonic solutions have a higher concentration of dissolved particles than blood. An example of hypertonic IV solution is 3% normal saline (3% NaCl). When infused, hypertonic fluids cause an increased concentration of dissolved solutes in the intravascular space compared to the cells. This causes the osmotic movement of water out of the cells and into the intravascular space to dilute the solutes in the blood. See Figure 23.6[38] for an illustration of osmotic movement of fluid out of a cell when hypertonic IV fluid is administered due to a higher concentration of solutes (pink molecules) in the bloodstream compared to the cell.
Hypertonic solutions move water out of the cells of the body and into the bloodstream. They are commonly used for patients with cerebral edema, severe hyponatremia, or some types of post-op patients. Hypertonic solutions must be used very cautiously due to potentially rapid side effects of fluid overload resulting in pulmonary edema, so they are typically administered in intensive care units (ICU). Hypertonic fluids should not be administered to patients with DKA because it will worsen their cellular dehydration.
When administering hypertonic fluids, it is essential to monitor for signs of fluid overload, such as significantly elevated blood pressure and difficulties breathing. Additionally, if hypertonic solutions with sodium are given, the patient's serum sodium level should be closely monitored.[39]
See Figure 23.7[40] for an illustration comparing how different types of IV solutions affect red blood cell size.
IV fluids are considered medications. As with all medications, nurses must check the rights of medication administration according to agency policy before administering IV fluids. What began as five rights of medication administration has been extended to eight rights according to the American Nurses Association. These eight rights include the following[41]:
- Right Patient
- Right Medication
- Right Dose
- Right Time
- Right Route
- Right Documentation
- Right Reason
- Right Response
Nurses also check for patient allergies, expiration date of the fluid, and compatibility of the fluid with any other fluids, medications, or blood products being administered intravenously. With any IV infusion, it is important for the nurse to pay close attention to the provider's order and make sure that it contains the specific type of fluid, any additives or medications, amount to be infused, rate of infusion, and the length of time that the therapy should continue. The nurse should also carefully assess a patient's hydration status and oral intake to ensure that IV fluids are stopped appropriately as a patent's condition changes. For example, weight should be assessed daily for patients receiving IV fluids to monitor for fluid overload.
Review how to check the rights of medication administration in the “Administration of Enteral Medications” chapter of Open RN Nursing Skills.
Electrolyte Imbalance
In addition to rapidly improving hydration status, IV fluids may also be administered to rapidly correct electrolyte imbalances. Infusing fluids with electrolytes such as potassium, calcium, and magnesium can correct electrolyte imbalances more rapidly and effectively than by oral supplementation. However, nurses must collaborate with the interprofessional team to identify medications that should and should not be given through peripheral veins. Current standards of care consider continuous peripheral infusion therapy of electrolytes to be inappropriate because of potential vascular endothelial damage. Ideally, peripheral IV therapy should be isotonic and consistent with physiological pH; otherwise, central venous access should be used.[42]
Electrolytes administered via the IV route must always be administered cautiously at the correct infusion rate because over supplementation can be deadly. For example, potassium infusions administered too rapidly into a patient's system can cause sudden cardiac arrest.
Blood Administration
Blood and blood components are administered by registered nurses via IV infusion, typically through larger sized IV catheters. Blood and blood components are transfused through a special transfusion administration set that has a filter designed to retain potentially harmful particles. Specific procedures for verifying the correct patient and correct blood product are performed prior to transfusion to prevent transfusion reactions that can be life-threatening. Administration of blood and blood components, including the use of infusion devices and ancillary equipment, and the identification, evaluation, and reporting of adverse events related to transfusion are established in agency policies, procedures, and/or practice guidelines. Read more information about blood administration in the "Administer Blood Products" chapter in Open RN Nursing Advanced Skills.
Nutrition
Nutritional therapy can be administered through an intravenous route for patients who do not have an adequately functioning gastrointestinal tract and/or are unable to take in food or fluids appropriately. Peripheral nutrition may be ordered through a peripheral IV site for nutritional needs such as albumin replacement.
Total parenteral nutrition (TPN) may be ordered for a patient based on their specific electrolyte and/or nutritional needs. TPN is a very concentrated solution that must be administered via a central line. Central lines are placed in a larger vessel rather than a smaller, peripheral vessel. Accessing a central vessel requires additional training and expertise to prevent complications with insertion and is further discussed in the Open RN Nursing Advanced Skills "Manage Central Lines” chapter. If a nurse receives an order for TPN therapy for a patient who does not have central line access, the order should be clarified with the prescribing provider.
Medications
The IV route is preferred for the administration of many medications when immediate onset is required. For example, many types of pain medications can be given directly into the bloodstream with a much more rapid onset of action than if they were to be administered orally. Rapid relief of pain can be achieved in minutes rather than hours required for oral medications to reach their peak. Rapid onset can also be achieved with other medications such as those used to treat cardiac emergencies or severe allergic reactions to quickly restore patients to optimal body functioning. Additional information about IV administration of medications is discussed in the Open RN Nursing Advanced Skills "Administer IV Push Medications” chapter.
IV Administration Equipment
Intravenous (IV) substances are administered through flexible plastic tubing called an IV administration set. The IV administration set connects the bag of solution to the patient’s IV access site. There are two major types of IV administration sets: primary administration sets and secondary administration sets. Administration sets require routine replacement to prevent infection. Follow agency policy regarding tubing changes before initiating a new bag of fluid or medications. See a summary of general guidelines for IV therapy and administration equipment in the box at the end of this section.
Primary Administration Sets
Primary administration sets can be used to infuse continuous or intermittent fluids, electrolytes, or medications. These substances may be administered by infusion pump or by gravity, and each method requires its own type of administration set.
Primary fluids are typically administered using an IV pump. An IV pump is the safest method of administration to ensure specific amounts of fluid are administered. The rate of infusion through an IV pump is typically calculated in mL/hour.
For infusion by gravity, a primary IV administration set can be a macro-drip or a micro-drip solution set. Macro-drip sets are used for routine primary infusions for adults. Micro-drip IV tubing is used in pediatric or neonatal care where small amounts of fluids are administered over a long period of time. A macro-drip infusion set delivers fluid at 10, 15, or 20 drops per milliliter, whereas a micro-drip infusion set delivers 60 drops per milliliter. The drop factor is located on the packaging of the IV tubing and is important to verify when calculating medication administration rates.
Primary IV administration sets consist of the following parts:
- Sterile spike: Used to spike the IV fluid bag and must be kept sterile.
- Roller clamp: Used to regulate the speed or stop an infusion by gravity.
- Drip chamber: Allows air to rise out from a fluid so that it is not passed onto the patient. The drip chamber should be kept ¼ to ½ full of solution. When setting a rate by gravity to "drops per minute," the dripping from this chamber is counted.
- Backcheck valve: Prevents fluid or medication from travelling up into the primary IV bag.
- Access ports: Used to infuse secondary medications and to administer IV push medications. These may also be referred to as “Y ports.”
Secondary Administration Sets
Secondary IV administration sets are used to intermittently administer a secondary medication, such as an antibiotic, while the primary IV is also running. Secondary IV tubing is shorter in length than primary tubing and is connected to a primary line via an access port above the infusion pump. The infusion pump is then set at the prescribed secondary infusion rate while the secondary medication is administered. By hanging the secondary medication bag higher than the primary bag, gravity pulls fluid from the secondary bag until it is empty rather than the primary bag.
Secondary medications may be “piggybacked” into primary infusion lines so the solution from the primary fluid line can be used to prime the secondary tubing. To prime the secondary tubing, after the secondary tubing is connected to the primary tubing, the bag connected to the secondary tubing is held lower than the primary bag, causing fluid from the primary tubing to backflow up the secondary tubing. This eliminates air from the secondary tubing.
See Figure 23.8[43] for an illustration of the setup of primary and secondary administration sets for primary administration of fluids and secondary administration of medication by gravity. See Figure 23.9[44] for an image of an IV infusion pump.
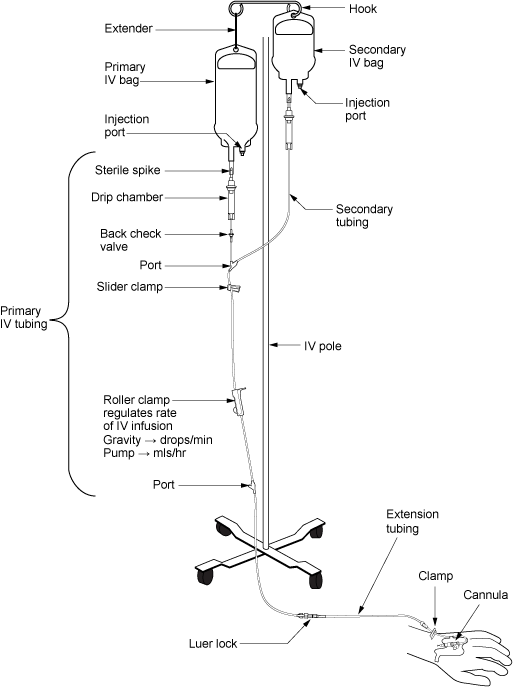

Priming IV Tubing
Primary administration sets, secondary administration sets, and extension tubing must be primed with IV solution to prevent air from entering the patient's circulatory system and causing an air embolism. Priming refers to the process of filling the IV tubing with IV solution prior to attaching it to the patient. Review steps for setting up and priming primary and secondary administration sets using the information in the following box.
Review checklists of steps for "Primary IV Solution Administration" and "Secondary IV Solution Administration" in the "IV Therapy Management" chapter of Open RN Nursing Skills.
Infection Control
Aseptic technique must be maintained throughout all IV therapy procedures, including initiation of IV access, preparing and maintaining IV equipment, administering IV fluids and medications, and discontinuing an IV system. Hand hygiene and strict aseptic technique must be performed when handling all IV equipment. These standards can be reviewed in the “Aseptic Technique” chapter. Additionally, if an IV catheter or IV administration set should become contaminated by contact with a nonsterile surface, it should be replaced with a new one to prevent introducing bacteria or other contaminants into the system.
Types of Venous Access
There are several types of venous access devices used to administer IV therapy that are categorized as peripheral devices or central devices. Venous access device selection is tailored to each patient's needs and to the type, duration, and frequency of infusion.
Peripheral Devices
Peripheral venous access devices are commonly used for short-term IV therapy in the hospital setting. A peripheral IV is an intravenous catheter inserted by percutaneous venipuncture into a peripheral vein and held in place with a sterile transparent dressing. The transparent dressing helps to keep the site sterile, prevents accidental dislodgement, and allows the nurse to visualize the insertion site through the dressing. A securement device may be added to prevent accidental dislodgement.
The patient’s upper extremities (hands and arms) are the preferred sites for insertion. However, a potential limitation of using the hand veins is they are smaller than the cephalic, basilic, or brachial veins in the arm. If the patient requires rapid infusions where a larger gauge IV is warranted, the larger veins in the upper arm should be considered.
Peripheral IVs are used for short-term infusions of fluids, medications, or blood. Peripheral IVs are easy to monitor and can be inserted at the bedside by nurses and other trained professionals. After IV access has been obtained, the hub of an intravenous catheter is attached to a short extension set or a primary IV administration set. Luer lock connectors on the extension tubing and/or administration sets permit syringes to be attached to administer medications or fluid flushes.
Saline lock refers to the use of a short extension set that allows IV access without requiring ongoing IV infusions. When not in use, the lock is flushed with saline according to agency policy and clamped to ensure the site remains sterile and blood does not flow out of the extension tubing. See Figure 23.10[45] for an image of a saline lock.

If the patient requires continuous infusion of IV fluids, the extension tubing from the IV catheter is connected to a primary IV administration set. The IV tubing can be run through an infusion pump to administer fluids or medications at a programmed rate of infusion (typically calculated in mL/hour) or via gravity by setting a drip rate with the roller clamp (typically calculated at drops/minute). Manufacturers list the drop rate on the IV packaging. Because of the risk of error that can occur with infusion by gravity, many agencies require the use of an infusion pump to ensure correct flow rate.
Contraindications to Peripheral IV Access Sites
Before inserting a peripheral IV, the patient should be assessed for contraindications related to insertion sites in the upper extremities. For example, patients who have a history of lumpectomy or mastectomy, an arteriovenous fistula, or current lymphedema often have restrictions that prohibit venipuncture into the affected extremity.[46] Additionally, deep vein thrombosis (DVT), fractures, contractures, or extensive scarring may also prohibit the placement of a peripheral IV. Hospitalized patients may have signage or a bracelet stating "limb alert" to alert heath care professionals to these conditions.
Midline Peripheral Catheters
Midline peripheral catheters have a larger catheter (i.e., 16-18 gauge) that allows for rapid infusions. Insertion is ultrasound-guided and can be inserted by RNs with additional training or other trained professionals. Midline catheters are typically inserted into the basilic, cephalic, or brachial veins of the upper arm with the tip placed near the level of the axilla. They are much longer and inserted deeper than a peripheral IV, but do not extend into a central vessel, so they are not considered a central line. Therefore, they have a lower risk of infection than central venous access. Any medication that can be administered through a peripheral line can be administered via a midline peripheral catheter. They can also be used for longer duration than traditional peripheral venous access, which is ideal for patients needing extended hospital stays or IV access. Based on agency policy, midline catheters may also be used for blood sample collection, thus limiting the number of venipunctures a patient receives. Site care for a midline peripheral catheter is similar to a peripheral IV dressing change.[47],[48]
Central Venous Access Devices
A central venous access device (CVAD) is a type of vascular access established by specially trained registered nurses and other health care personnel. It involves the insertion of a tube into a vein in the neck, chest, or groin and threaded into a central vein (most commonly the internal jugular, subclavian, or femoral) and advanced until the tip of the catheter resides within the inferior vena cava, superior vena cava, or right atrium.[49] Only specially trained health professionals may insert central venous access devices, but nurses provide routine care of CVADs, including dressing changes. See Figure 23.11[50] for an image of a central line requiring a dressing change.
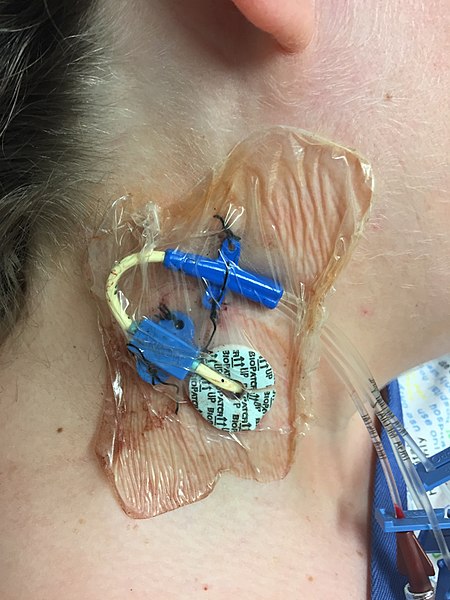
A central venous access device can be left in for longer periods of time and is useful for administering concentrated medications and fluids, such as TPN or hyperosmotic fluids, that would be otherwise irritating to smaller peripheral veins. However, central venous access devices have an increased risk for the development of bloodstream infections, so strict sterile technique is required during insertion, and aseptic technique is used for maintenance. Central venous access devices are further discussed in the "Manage Central Lines" chapter of Open RN Nursing Advanced Skills.
Peripheral Inserted Central Catheters
A peripheral inserted central catheter (PICC) is a thin, flexible tube inserted into a vein in the upper arm and guided into the superior vena cava. It is used to give intravenous fluids, blood transfusions, chemotherapy, and other medications requiring a central line. It can also be used for blood sampling. A PICC may stay in place for weeks or months and helps avoid the need for repeated needlesticks. PICC lines are further discussed in the "Manage Central Lines" chapter of Open RN Nursing Advanced Skills.
General Guidelines for IV Therapy
The following are general guidelines for peripheral IV therapy[51]:
- IV fluid therapy is ordered by a provider. The order must include the type of solution or medication, total amount of fluid, rate of infusion, duration, date, and time.
- IV therapy is an invasive procedure. Significant complications can occur if the wrong amount of IV fluids or incorrect medication is given or if aseptic technique is not strictly followed.
- Nurses must understand the indications and duration for IV therapy for each patient. Practice guidelines recommend that patients receiving IV therapy for more than six days should be assessed for an intermediate or long-term device such as a central venous access device (CVAD).
- Hospitalized patients may have an order for a small hourly infusion rate, such as 10-20 mL/hour, historically referred to in practice as a "to keep open" (TKO) or "keep vein open" (KVO) rate.
- IV administration sets require routine replacement to promote patient safety and reduce the risk of infection. Primary and secondary continuous administration sets used to administer solutions other than lipids, blood, or blood products are typically changed every 96 hours, or up to every 7 days, as directed by agency policy and/or the manufacturer’s instructions. Administration sets should also be changed if contamination or compromise in the integrity of the product or system is suspected. Secondary administration sets that are detached from a primary administration set are typically changed every 24 hours or as directed by agency policy. Administration sets should be labelled according to agency policy with the date of initiation or the date of change indicated.[52]
Calculated arterial oxygen saturation level.

