Open Resources for Nursing (Open RN)
Before every patient interaction, the nurse must perform hand hygiene and consider the use of additional personal protective equipment, introduce themselves, and identify the patient using two different identifiers. It is also important to provide a culturally safe space for interaction and to consider the developmental stage of the patient.
Hand Hygiene and Infection Prevention
Before initiating care with a patient, hand hygiene is required, and a risk assessment should be performed to determine the need for personal protective equipment (PPE). This is important for protection of both patient and nurse.
Hand Hygiene
Hand hygiene is a simple but effective way to prevent infection when performed correctly and at the appropriate times when providing patient care. See Figure 1.3.[1] for an image about hand hygiene from the Centers for Disease Control (CDC).[2] Use the information below to learn more and watch a video about effective handwashing.
Key points from the CDC about hand hygiene include the following[3]:
- In general, hand sanitizers are as effective as washing with soap and water and are less drying to the skin. When using hand sanitizer, use enough gel to cover both hands and rub for approximately 20 seconds, coating all surfaces of both hands until your hands feel dry. Go directly to the patient without putting your hands into pockets or touching anything else.[4]
- Be sure to wash with soap and water if your hands are visibly soiled or the patient has diarrhea from suspected or confirmed C. Difficile (C-diff).
- Clean all areas of the hands, including the front and back, the fingertips, the thumbs, and between fingers.
- Gloves are not a substitute for cleaning your hands. Wash your hands after removing gloves.
- Hand hygiene should be performed at these times:
- Immediately before touching a patient
- Before performing an aseptic task (e.g., placing an indwelling device) or handling invasive medical devices
- Before moving from working on a soiled body site to a clean body site on the same patient
- After contact with blood, body fluids, or contaminated surfaces
- Before donning gloves and immediately after glove removal
- When leaving the area after touching a patient or their immediate environment
Checklists for performing handwashing and using hand sanitizer are located in Appendix A.
Visit the Center for Disease Control and Prevention’s website to read more about Hand Hygiene in Healthcare Settings.
Download a PDF factsheet from the Centers for Disease Control and Prevention called Clean Hands Count.
View supplementary videos on hand hygiene:
Clean Hands Count on YouTube[5]
Hand Washing Technique on YouTube[6]
Hand Sanitizing Technique on YouTube[7]
Personal Protective Equipment (PPE)
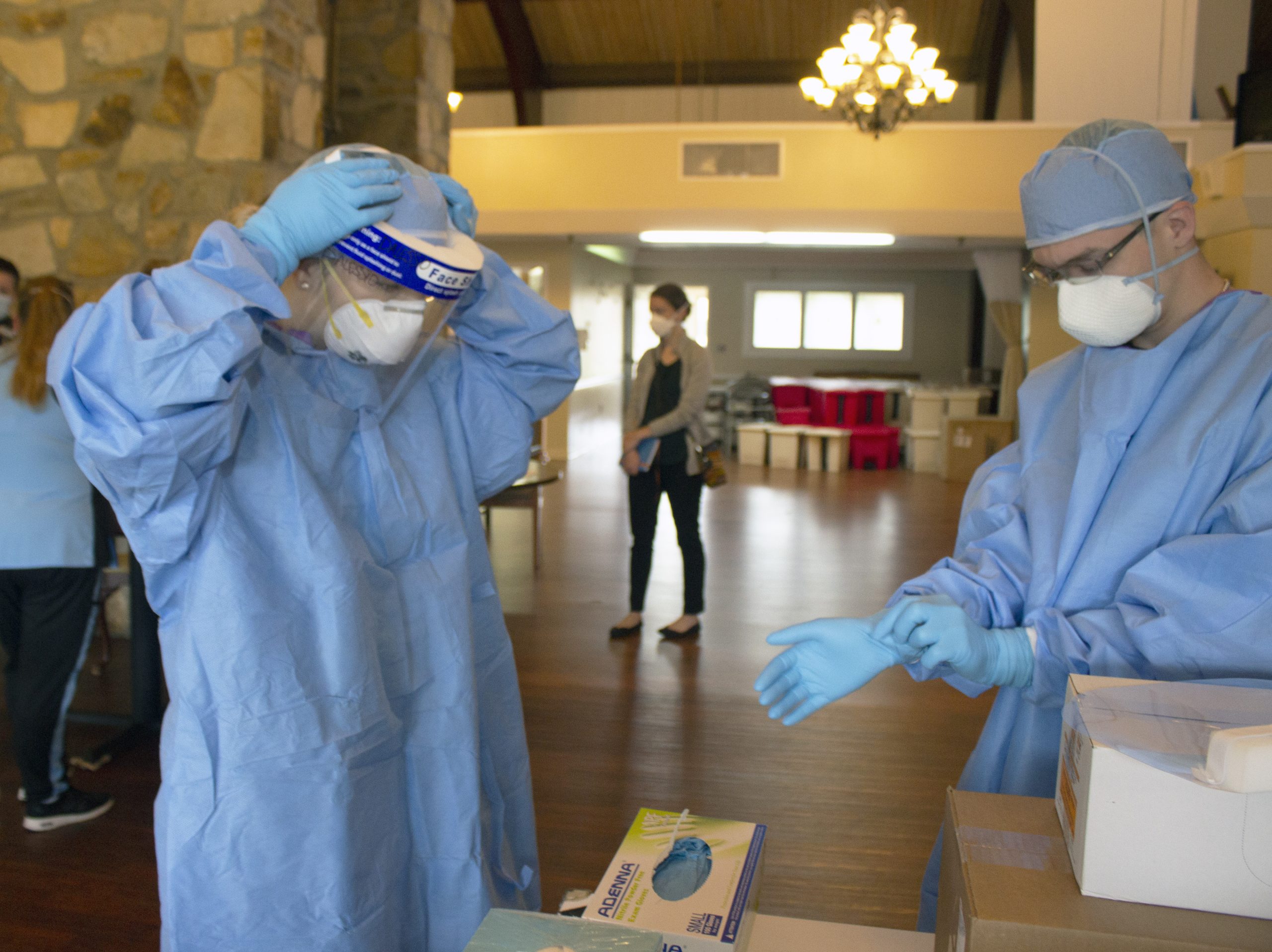
Medical asepsis is a term used to describe measures to prevent the spread of infection in health care agencies. Performing hand hygiene at appropriate times during patient care and applying gloves when there is potential risk for exposure to body fluids are examples of using medical asepsis. Additional precautions are implemented by health care team members when a patient has, or is suspected of having, an infectious disease. These additional precautions are called personal protective equipment (PPE) and are based on how an infection is transmitted, such as by contact, droplet, or airborne routes. Personal protective equipment (PPE) includes gowns, eyewear or goggles, face shields, gloves, and masks. PPE is used along with environmental controls, such as surface cleaning and disinfecting to prevent the transmission of infection.[8] See Figure 1.4[9] for an image of health care team members applying PPE. These precautions are further discussed in the “Aseptic Technique” chapter. For the purpose of this chapter, be sure to perform a general risk assessment before entering a patient’s room and apply the appropriate PPE as needed. This risk assessment includes the following:
- Is there signage posted on the patient’s door that contact, droplet, enhanced barrier, or airborne precautions are in place? If so, follow the instructions provided.
- Does this patient have a confirmed or suspected infection or communicable disease?
- Will your face, hands, skin, mucous membranes, or clothing be potentially exposed to blood or body fluids by spray, coughing, or sneezing?
Introducing Oneself
When initiating care with patients, it is essential to first provide privacy, and then introduce yourself and explain what will be occurring. Providing privacy means taking actions such as talking with the patient privately in a room with the door shut or privacy curtain drawn around the bed. A common framework used to communicate with patients is AIDET, a mnemonic for Acknowledge, Introduce, Duration, Explanation, and Thank You.[10]
- Acknowledge: Greet the patient by the name documented in their medical record. Make eye contact, smile, and acknowledge any family or friends in the room. Ask the patient their preferred way of being addressed (for example, “Mr. Doe,” “Jonathon,” or “Johnny”) and their preferred pronouns (i.e., he/him, she/her, or they/them), as appropriate.
- Introduce: Introduce yourself by your name and role. For example, “I’m John Doe and I am a nursing student working with your nurse to take care of you today.”
- Duration: Estimate a timeline for how long it will take to complete the task you are doing. For example, “I am here to obtain your blood pressure, heart rate, and oxygen saturation levels. This should take about 5 minutes.”
- Explanation: Explain step by step what to expect next and answer questions. For example, “I will be putting this blood pressure cuff on your arm and inflating it. It will feel as if it is squeezing your arm for a few moments.”
- Thank You: At the end of the encounter, thank the patient and ask if anything is needed before you leave. In an acute or long-term care setting, ensure the call light is within reach and the patient knows how to use it. If family members are present, thank them for being there to support the patient as appropriate. For example, “Thank you for taking time to talk with me today. Is there anything I can get for you before I leave the room? Here is the call light (Place within reach). Press the red button if you would like to call the nurse.”
For more information about AIDET, visit AIDET Patient Communication.
Patient Identification
Use at least two patient identifiers before performing assessments, obtaining vital signs, or providing care.
Use two patient identifiers:
- Ask the patient to state their name and date of birth. If they have an armband, compare the information they are stating to the information on the armband and verify they match. See Figure 1.5[11] for an image of an armband.
- If the patient doesn’t have an armband, confirm the information they are stating to information provided in the chart.
- If the patient is unable to state their name and date of birth, scan their armband or ask another staff member or family member to identify them.
Confirm “two identifiers” with a second source:
- Scan the wristband.
- Compare the name and date of birth to the patient’s chart.
- Ask staff to verify the patient in a long-term care setting.
- Compare the picture on the medication administration record (MAR) to the patient.
- If present, ask a family member to confirm the patient’s name.

Cultural Safety
When initiating patient interaction, it is important to establish cultural safety. Cultural safety refers to the creation of safe spaces for patients to interact with health professionals without judgment or discrimination. See Figure 1.6[12] for an image representing cultural safety. Recognizing that you and all patients bring a cultural context to interactions in a health care setting is helpful when creating cultural safe spaces. If you discover you need more information about a patient’s cultural beliefs to tailor your care, use an open-ended question that allows the patient to share what they believe to be important. For example, you may ask, “I am interested in your cultural background as it relates to your health. Can you share with me what is important about your cultural background that will help me care for you?”[13]
For more information about caring for diverse patients, visit the “Diverse Patients” chapter in the Open RN Nursing Fundamentals textbook.
Adapting to Variations Across the Life Span
It is important to adapt your interactions with patients in accordance with their developmental stage. Developmentalists break the life span into nine stages[14]:
- Prenatal Development
- Infancy and Toddlerhood
- Early Childhood
- Middle Childhood
- Adolescence
- Early Adulthood
- Middle Adulthood
- Late Adulthood
- Death and Dying
A brief overview of the characteristics of each stage of human development is provided in Table 1.2. When caring for infants, toddlers, children, and adolescents, parents or guardians are an important source of information, and family dynamics should be included as part of the general survey assessment. When caring for older adults or those who are dying, other family members may be important to include in the general survey assessment. See Figure 1.7[15] for an image representing patients in various developmental stages of life.

Visit the Human Development Life Span e-book at LibreTexts to read additional information about human development across the life span.
Table 1.2 Variations Across the Life Span
| Stage of Development | Common Characteristics |
|---|---|
| Prenatal Development | Conception occurs, and development begins. All major structures of the body are forming, and the health of the mother is of primary concern. Understanding nutrition, teratogens (environmental factors that can lead to birth defects), and labor and delivery are primary concerns for the mother. |
| Infancy and Toddlerhood | The first year and a half to two years of life are ones of dramatic growth and change. A newborn with a keen sense of hearing but very poor vision is transformed into a walking, talking toddler within a relatively short period of time. Caregivers are also transformed from someone who manages feeding and sleep schedules to a constantly moving guide and safety inspector for a mobile, energetic child. |
| Early Childhood | Early childhood is also referred to as the preschool years, consisting of the years that follow toddlerhood and precede formal schooling. As a three- to five-year-old, the child is busy learning language, gaining a sense of self and greater independence, and beginning to learn the workings of the physical world. This knowledge does not come quickly however, and preschoolers may have initially interesting conceptions of size, time, space, and distance, such as fearing that they may go down the drain if they sit at the front of the bathtub. A toddler’s fierce determination to do something may give way to a four-year-old’s sense of guilt for doing something that brings the disapproval of others. |
| Middle Childhood | The ages of six through eleven comprise middle childhood, and much of what children experience at this age is connected to their involvement in the early grades of school. Their world becomes filled with learning and testing new academic skills, assessing one’s abilities and accomplishments, and making comparisons between self and others. Schools compare students and make these comparisons public through team sports, test scores, and other forms of recognition. Growth rates slow down, and children are able to refine their motor skills at this point in life. Children begin to learn about social relationships beyond the family through interaction with friends and fellow students. |
| Adolescence | The World Health Organization defines adolescence as a person between the age of 10 and 19. Adolescence is a period of dramatic physical change marked by an overall physical growth spurt and sexual maturation, known as puberty. It is also a time of cognitive change as the adolescent begins to think of new possibilities and to consider abstract concepts such as love, fear, and freedom. Adolescents have a sense of invincibility that puts them at greater risk of injury from high-risk behaviors such as car accidents, drug and alcohol abuse, or contracting sexually transmitted infections that can have lifelong consequences or result in death. |
| Early Adulthood | The twenties and thirties are often thought of as early adulthood. It is a time of physiological peak but also highest risk for involvement in violent crimes and substance abuse. It is a time of focusing on the future and putting a lot of energy into making choices that will help one earn the status of a full adult in the eyes of others. Love and work are primary concerns at this stage of life. |
| Middle Adulthood | The late thirties through the mid-sixties is referred to as middle adulthood. This is a period in which aging processes that began earlier become more noticeable but also a time when many people are at their peak of productivity in love and work. It can also be a time of becoming more realistic about possibilities in life previously considered and of recognizing the difference between what is possible and what is likely to be achieved in their lifetime. |
| Late Adulthood | This period of the life span has increased over the last 100 years. For nurses, patients in this period are referred to as “older adults.” The term “young old” is used to describe people between 65 and 79, and the term “old old” is used for those who are 80 and older. One of the primary differences between these groups is that the young old are very similar to midlife adults because they are still working, still relatively healthy, and still interested in being productive and active. The “old old” may remain productive, active, and independent, but risks of heart disease, lung disease, cancer, and cerebral vascular disease (i.e., strokes) increase substantially for this age group. Issues of housing, health care, and extending active life expectancy are only a few of the topics of concern for this age group. A better way to appreciate the diversity of people in late adulthood is to go beyond chronological age and examine whether a person is experiencing optimal aging (when they are in very good health for their age and continue to have an active, stimulating life), normal aging (when the changes in health are similar to most of those of the same age), or impaired aging (when more physical challenges and diseases occur compared to others of the same age). |
| Death and Dying | Death is the final stage of life. Dying with dignity allows an individual to make choices about treatment, say goodbyes, and take care of final arrangements. When caring for patients who are actively dying, nurses can advocate for care that allows that person to die with dignity according to their wishes. |
- “Animated-Logo-Clean-Hands-Count” by Centers for Disease Control and Prevention is licensed under CC0. Access for free at https://www.cdc.gov/handhygiene/campaign/index.html ↵
- Centers for Disease Control and Prevention. (2019, April 29). Hand hygiene. https://www.cdc.gov/handhygiene/index.html ↵
- Centers for Disease Control and Prevention. (2019, April 29). Hand hygiene. https://www.cdc.gov/handhygiene/index.html ↵
- Centers for Disease Control and Prevention. (2019, April 29). Hand hygiene. https://www.cdc.gov/handhygiene/index.html ↵
- Centers for Disease Control and Prevention. (2017, May 5). Clean hands count [Video]. YouTube. All rights reserved. https://youtu.be/MzkNSzqmUSY ↵
- Johns Hopkins Medicine. (2019, March 26). Hand-washing steps using the WHO technique [Video]. YouTube. All rights reserved. https://youtu.be/IisgnbMfKvI ↵
- Johns Hopkins Medicine. (2019, May 8). Hand rubbing steps using the WHO technique [Video]. YouTube. All rights reserved. https://youtu.be/B3eq5fLzAOo ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology licensed under CC BY 4.0 ↵
- “Pennsylvania_National_Guard_(49923831732).jpg” by The National Guard is in the Public Domain. ↵
- Huron. (n.d.). AIDET patient communication. https://www.studergroup.com/aidet ↵
- “barcode_clinic_fist_hand_healthcare_hospital_identification_identity-1517387.jpg” by rawpixel.com is licensed under CC0 ↵
- “MODEL OF MULTINATIONAL UNITY” by Margherita Marchetti is licensed under CC0 ↵
- This work is a derivative of The Complete Subjective Health Assessment by Lapum, St-Amant, Hughes, Petrie, Morrell, & Mistry and is licensed under CC BY 4.0 ↵
- This work is a derivative of Human Development Life Span by Laura Overstreet and is licensed under CC BY 4.0 ↵
- “pexels-photo-1556706.jpeg” by Daniel Reche is licensed under CC0; “kids-1675964_960_720.jpg” by auntmasako is licensed under CC0; “100312-F-6448T-001.JPG” by U.S. Air Force photo/Senior Airman Timothy Taylor is licensed under CC0; “smart-3479338_1280.jpg” by malcolmbeldon4 is licensed under CC0; “Business man” by Tim Engle is licensed under CC BY-NC 2.0; “Portrait of an old woman in front of her home” by Nithi Anand is licensed under CC BY 2.0 ↵
Fluids found between the cells and outside of the vascular system.
Fluids found in the vascular system consisting of the body’s arteries, veins, and capillary networks.
Movement of fluid through a semipermeable membrane from an area of lesser solute concentration to an area of greater solute concentration.
Intravascular fluid loss. Used interchangeably with “deficient fluid volume” and “dehydration.”
Adult day care centers: Care that offers people with dementia and other chronic illnesses the opportunity to be social and to participate in activities in a safe environment, while also giving their caregivers the opportunity to work, run errands, or take a much-needed break. (Chapter 6.3)
Ageism: The stereotyping and discrimination against individuals or groups on the basis of their age. Ageism can take many forms, including prejudicial attitudes, discriminatory practices, or institutional policies and practices that perpetuate stereotypical beliefs. (Chapter 6.4)
Alzheimer’s disease: An irreversible, progressive brain disorder that slowly destroys memory and thinking skills and eventually the ability to carry out the simplest tasks. (Chapter 6.3)
Cognition: A term used to describe our ability to think. (Chapter 6.1)
Cognitive impairment: Impairment in mental processes that drive how an individual understands and acts in the world, affecting the acquisition of information and knowledge. (Chapter 6.2)
Delirium: An acute state of cognitive impairment that typically occurs suddenly due to a physiological cause, such as infection, hypoxia, electrolyte imbalances, drug effects, or other acute brain injury. (Chapter 6.2)
Dementia: A chronic condition of impaired cognition, caused by brain disease or injury, marked by personality changes, memory deficits, and impaired reasoning. Dementia can be caused by a group of conditions, such as Alzheimer’s disease, vascular dementia, frontal-temporal dementia, and Lewy body disease. It is gradual, progressive, and irreversible. (Chapter 6.2)
Depression: A brain disorder that can cause a persistent low mood, memory problems, loss of interest in life, and other symptoms that can overlap with dementia. (Chapter 6.2)
Development: Biological changes, as well as social and cognitive changes, that occur continuously throughout our lives. (Chapter 6.2)
Growth: Physical changes that occur during the development of an individual beginning at the time of conception. (Chapter 6.2)
Hospice care: A type of care selected by clients who are terminally ill and whose health care provider has determined they are expected to live six months or less that focuses on providing comfort and dignity at the end of life. It involves care and support services that can be of great benefit to people in the final stages of dementia and to their families. (Chapter 6.3)
Intellectual disability: A diagnostic term that describes intellectual and adaptive functioning deficits identified during the developmental period prior to the age 18. (Chapter 6.2)
Respite care: Care provided at home (by a volunteer or paid service) or in a care setting, such as adult day centers or residential facilities, that allows the caregiver to take a much-needed break. (Chapter 6.3)
Sundowning: Increased confusion, anxiety, agitation, pacing, or disorientation in clients with dementia that typically begins at dusk and continues throughout the night. (Chapter 6.3)
The movement of solute particles from an area of higher concentration to an area of lower concentration.

