Open Resources for Nursing (Open RN)
Tracheostomy suctioning may be performed with open or closed technique. Open suctioning requires disconnection of the patient from the oxygen source, whereas closed suctioning uses an inline suctioning catheter that does not require disconnection. This checklist will explain the open suctioning technique.
Indications for tracheostomy suctioning include the following:
- Need to maintain the patency and integrity of the artificial airway
- Deterioration of oxygen saturation and/or arterial blood gas values
- Visible secretions in the airway
- Patient’s inability to generate an effective spontaneous cough
- Acute respiratory distress
- Suspected aspiration of gastric or upper-airway secretions
- Need to obtain a sputum specimen[1]
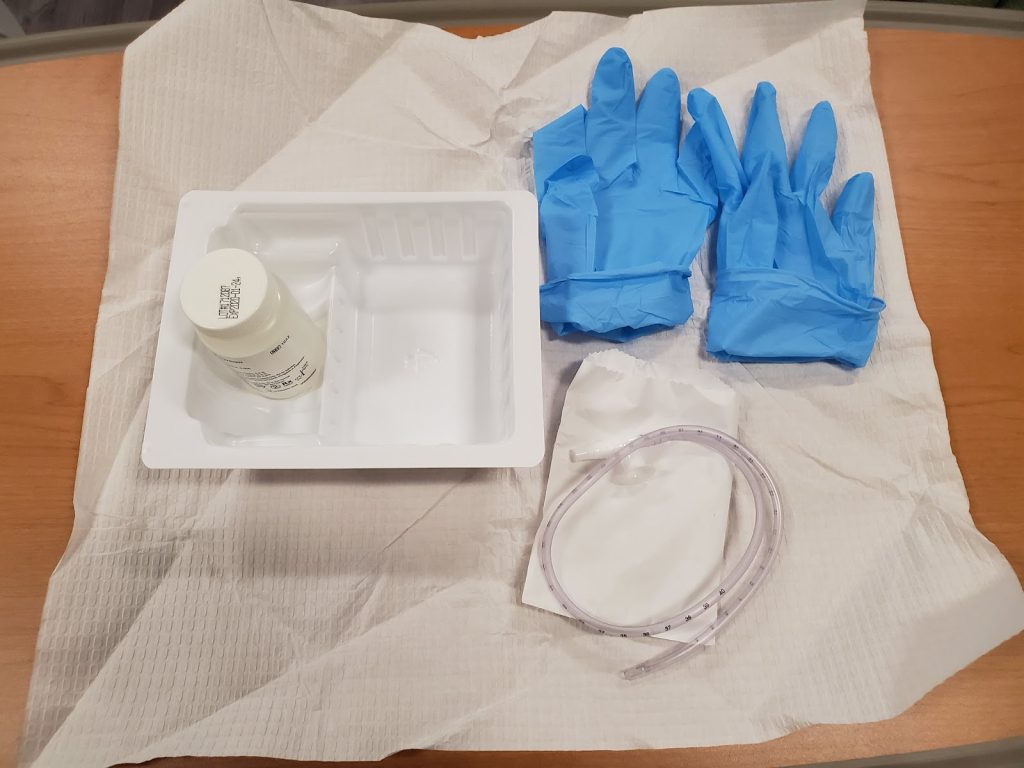
Similar assessments and monitoring apply when performing tracheostomy suctioning compared with other types of suctioning with the addition of assessing the stoma. The stoma should be free from redness and drainage. Hyperoxygenation using a bag mask valve attached to an oxygen source may be required before and during the open suctioning procedure based on the patient’s oxygenation status. See Figure 22.8[2] for an image of an example of sterile tracheostomy suctioning kit.
![]()
- To ensure patient safety, a replacement tracheostomy tube, an obturator, a bag valve mask (Ambu bag), and suction catheter kit must always be available in the room.
- Communication should be facilitated with the patient using written processes when possible.
- Follow agency policy regarding hyperoxygenation and hyperventilation prior to and during suctioning.
- Do not suction for more than 15 seconds per pass.[3]
- During the procedure, it is important to continually monitor the patient’s pulse oximetry to determine if the oxygen saturation is maintaining at an adequate level.
- Perform oral care after suctioning according to agency policy.
Checklist for Tracheostomy Suctioning[4]
Use the checklist below to review the steps for “Tracheostomy Suctioning.”
View an instructor demonstration of Tracheostomy Suctioning[5]:
Steps
Disclaimer: Always review and follow agency policy regarding this specific skill.
- Gather supplies: sterile gloves, tracheostomy suction kit, mask with face shield, gown, goggles, pulse oximetry, and bag valve device. It is helpful to request assistance from a second nurse if preoxygenating the patient before suction passes.
- Perform safety steps.
- Perform hand hygiene.
- Check the room for transmission-based precautions.
- Introduce yourself, your role, the purpose of your visit, and an estimate of the time it will take.
- Confirm patient ID using two patient identifiers (e.g., name and date of birth).
- Explain the process to the patient and ask if they have any questions.
- Be organized and systematic.
- Use appropriate listening and questioning skills.
- Listen and attend to patient cues.
- Ensure the patient’s privacy and dignity.
- Assess ABCs.
- Verify that there are a backup tracheostomy tube, obturator, and bag valve device available at the bedside.
- Assess lung sounds, respiratory rate, heart rate and rhythm, and pulse oximetry.
- Raise the head of the bed to a comfortable working height. Place the patient in a semi-Fowler’s position and apply the pulse oximeter for monitoring during the procedure.
- Turn on the suction. Set the suction gauge to the appropriate setting based on age of the patient.
- Perform hand hygiene. Don appropriate PPE.
- Open the suction catheter package faced away from you to maintain sterility.
- Don the sterile gloves from the kit.
- Remove the sterile fluid and check the expiration date.
- Open the sterile container used for flushing the catheter and place it back into the kit. Pour the sterile fluid into the sterile container using sterile technique.
- Remove the suction catheter from the packaging. Ensure the catheter size is not greater than half of the inner diameter of the tracheostomy tube.
- Keep the catheter sterile by holding it with your dominant hand and attaching it to the suction tubing with your nondominant hand. Note that your nondominant hand is no longer sterile.
- Test the suction and lubricate the sterile catheter by using your sterile hand to dip the end into the sterile saline while occluding the thumb control.
- Ask an assistant to preoxygenate the patient with 100% oxygen for 30 to 60 seconds using a handheld bag valve mask (Ambu bag) per agency protocol. Alternatively, ask the patient to take two or three deep breaths if able.
- Insert the catheter into the patient’s tracheostomy tube using your sterile hand without applying suctioning:
- For shallow suctioning, insert the catheter the length of the tracheostomy tube before beginning any suctioning.
- For deep suctioning, insert the catheter until resistance is met (at the carina) and withdraw 1 centimeter before beginning suctioning.
- Do not force the catheter.
- Keep the dominant (sterile) hand at least one inch from the end of the trach tube.
- To apply suction, place your nondominant thumb over the control valve.
- Withdraw the catheter while continually rotating it between your fingers to suction all sides of the tracheostomy tube. Do not suction longer than 15 seconds to prevent hypoxia. Follow agency policy regarding the use of intermittent or continuous suctioning. Do not contaminate the catheter as you remove it from the trach tube.
- Suction sterile saline each time the suction catheter is removed to flush the catheter and suction tubing of secretions.
- Assess the patient response to suctioning; hyperoxygenation may be required. If dysrhythmia or bradycardia occur, stop the procedure.
- Allow the patient to rest. After the patient’s pulse oximetry returns to baseline, a second suctioning pass can be initiated if clinically indicated. Encourage the patient to cough and deep breathe to remove secretions between suctioning passes.
- Do not insert the suction catheter more than two times. If the patient’s respiratory status does not improve or it worsens, call for emergency assistance.
- Reattach the preexisting oxygen delivery device to the patient with your noncontaminated hand.
- Evaluate the effectiveness of the procedure and the patient’s respiratory status. Assess patency of the airway and pulse oximetry.
- Remove the catheter from the tubing and then remove gloves while holding the catheter inside the glove. Perform hand hygiene.
- Turn off the suction.
- Perform proper hand hygiene and don clean gloves.
- Reassess lung sounds, heart rate and rhythm, and pulse oximetry for improvement.
- Perform patient oral care.
- Remove gloves and perform proper hand hygiene.
- Assist the patient to a comfortable position, ask if they have any questions, and thank them for their time.
- Ensure safety measures when leaving the room:
- CALL LIGHT: Within reach
- BED: Low and locked (in lowest position and brakes on)
- SIDERAILS: Secured
- TABLE: Within reach
- ROOM: Risk-free for falls (scan room and clear any obstacles)
- Perform hand hygiene.
- Document the procedure and related assessment findings. Report any concerns according to agency policy.
Sample Documentation
Sample Documentation of Expected Findings
Mucus present at entrance to tracheostomy tube. Hyperoxygenation provided for 30 seconds before and after suctioning using a bag valve mask with FiO2 100%. Patient’s pulse oximetry remained 92-96% during suctioning. Moderate amount of thick, white mucus without odor was suctioned. Post-procedure: HR 78, RR 18, O2 sat 96%, and lung sounds clear throughout all lobes. Patient tolerated the procedure without discomfort.
Sample Documentation of Unexpected Findings
Mucus present at entrance to tracheostomy tube. Hyperoxygenation provided for 30 seconds before and after suctioning using a bag valve mask with FiO2 100%. During the first suctioning pass, the ECG demonstrated bradycardia with HR dropping into the 50s. Suctioning stopped. Trach tube was reattached to the mechanical ventilator and emergency assistance requested from the respiratory therapist. Moderate amount of thick, white mucus without odor suctioned. Post-procedure, HR 78, RR 18, O2 sat 96% and lung sounds clear throughout all lobes.
- American Association for Respiratory Care. (2010). AARC clinical practice guideline: Endotracheal suctioning of mechanically ventilated patients with artificial airways 2010. Respiratory Care, 55(6), 758-764. http://www.rcjournal.com/cpgs/pdf/06.10.0758.pdf ↵
- “Example of a Sterile Tracheostomy Kit” by Julie Teeter at Gateway Technical College is licensed under CC BY 4.0 ↵
- American Association for Respiratory Care. (2010). AARC clinical practice guideline: Endotracheal suctioning of mechanically ventilated patients with artificial airways 2010. Respiratory Care, 55(6), 758-764. http://www.rcjournal.com/cpgs/pdf/06.10.0758.pdf ↵
- Tracheostomy suctioning. (2020). Lippincott procedures. http://procedures.lww.com ↵
- Open RN Project. (2021, November 11). Tracheostomy suctioning [Video]. YouTube. Video licensed under CC-BY-4.0. https://youtu.be/VJ6kSydvaog ↵

