Open Resources for Nursing (Open RN)
Outcome Identification is the third step of the nursing process (and the third Standard of Practice by the American Nurses Association). This standard is defined as, “The registered nurse identifies expected outcomes for a plan individualized to the health care consumer or the situation.” The RN collaborates with the health care consumer, interprofessional team, and others to identify expected outcomes integrating the health care consumer’s culture, values, and ethical considerations. Expected outcomes are documented as measurable goals with a time frame for attainment.[1] Outcome identification is performed by RNs and is outside the scope of practice for LPN/VNs, but LPN/VNs must be aware of expected outcomes for clients in their nursing care plan.
An outcome is a “measurable behavior demonstrated by the client’s response to nursing interventions.”[2] Outcomes should be identified before nursing interventions are planned. After nursing interventions are implemented, the nurse will evaluate if the outcomes were met in the time frame indicated for that client.
Outcome identification includes setting short- and long-term goals and then creating specific expected outcome statements for each nursing diagnosis. See Figure 4.9a for an illustration of how the Outcome Identification phase of the nursing process correlates to the NCSBN Clinical Judgment Model.[3]

Short-Term and Long-Term Goals
Nursing care should always be individualized and client centered. No two people are the same, and neither should nursing care plans be the same for two people. Goals and outcomes should be tailored specifically to each client’s needs, values, and cultural beliefs. Clients and family members should be included in the goal-setting process when feasible. Involving clients and family members promotes awareness of identified needs, ensures realistic goals, and motivates their participation in the treatment plan to achieve the mutually agreed upon goals and live life to the fullest with their current condition.
The nursing care plan is a road map used to guide client care so that all health care providers are moving toward the same client goals. Goals are broad statements of purpose that describe the overall aim of care. Goals can be short- or long-term. The time frame for short- and long-term goals is dependent on the setting in which the care is provided. For example, in a critical care area, a short-term goal might be set to be achieved within an 8-hour nursing shift, and a long-term goal might be in 24 hours. In contrast, in an outpatient setting, a short-term goal might be set to be achieved within one month and a long-term goal might be within six months.
A nursing goal is the overall direction in which the client must progress to improve the problem/nursing diagnosis and is often the opposite of the problem.
Example of a Broad Goal
Refer to Scenario C in the “Assessment” section of this chapter. Ms. J. had a priority nursing diagnosis of Excess Fluid Volume. A broad goal would be, “Ms. J. will achieve a state of fluid balance.”
Expected Outcomes
Goals are broad, general statements, but outcomes are specific and measurable. Expected outcomes are statements of measurable action for the client within a specific time frame that are responsive to nursing interventions. Nurses may create expected outcomes independently or refer to classification systems for assistance. Just as NANDA-I creates and revises standardized nursing diagnoses, a similar classification and standardization process exists for expected nursing outcomes. The Nursing Outcomes Classification (NOC) is a list of over 330 nursing outcomes designed to coordinate with established NANDA-I diagnoses.[4]
Client-Centered
Outcome statements are always client-centered. They should be developed in collaboration with the client and individualized to meet a client’s unique needs, values, and cultural beliefs. They should start with the phrase “The client will…” Outcome statements should be directed at resolving the defining characteristics the client is exhibiting for the nursing diagnosis. Additionally, the outcome must be something the client would like to achieve.
Outcome statements should contain five components easily remembered using the “SMART” mnemonic:[5]
- Specific
- Measurable
- Attainable/Action oriented
- Relevant/Realistic
- Timeframe
See Figure 4.9[6] for an image of the SMART components of outcome statements. Each of these components is further described in the following subsections.

Specific
Outcome statements should state precisely what is to be accomplished. See examples of a not specific and a specific outcome in the following box.
Example
- Not specific outcome: “The client will increase the amount of exercise.”
- Revised as a specific outcome: “The client will participate in a bicycling exercise session daily for 30 minutes.”
Additionally, only one action should be included in each expected outcome. See examples in the following box.
Example
- More than one action: “The client will walk 50 feet three times a day with standby assistance of one and will shower in the morning until discharge” is actually two goals written as one. The outcome of ambulation should be separate from showering for precise evaluation. For instance, the client could shower but not ambulate, which would make this outcome statement very difficult to effectively evaluate.
- Revised to create two outcome statements so each can be measured: The client will walk 50 feet three times a day with standby assistance of one until discharge. The client will shower every morning until discharge.
Measurable
Measurable outcomes have numeric parameters or other concrete methods of judging whether the outcome was met. It is important to use objective data to measure outcomes. If terms like “acceptable” or “normal” are used in an outcome statement, it is difficult to determine whether the outcome is attained. Refer to Figure 4.10[7] for examples of verbs that are measurable and not measurable in outcome statements.
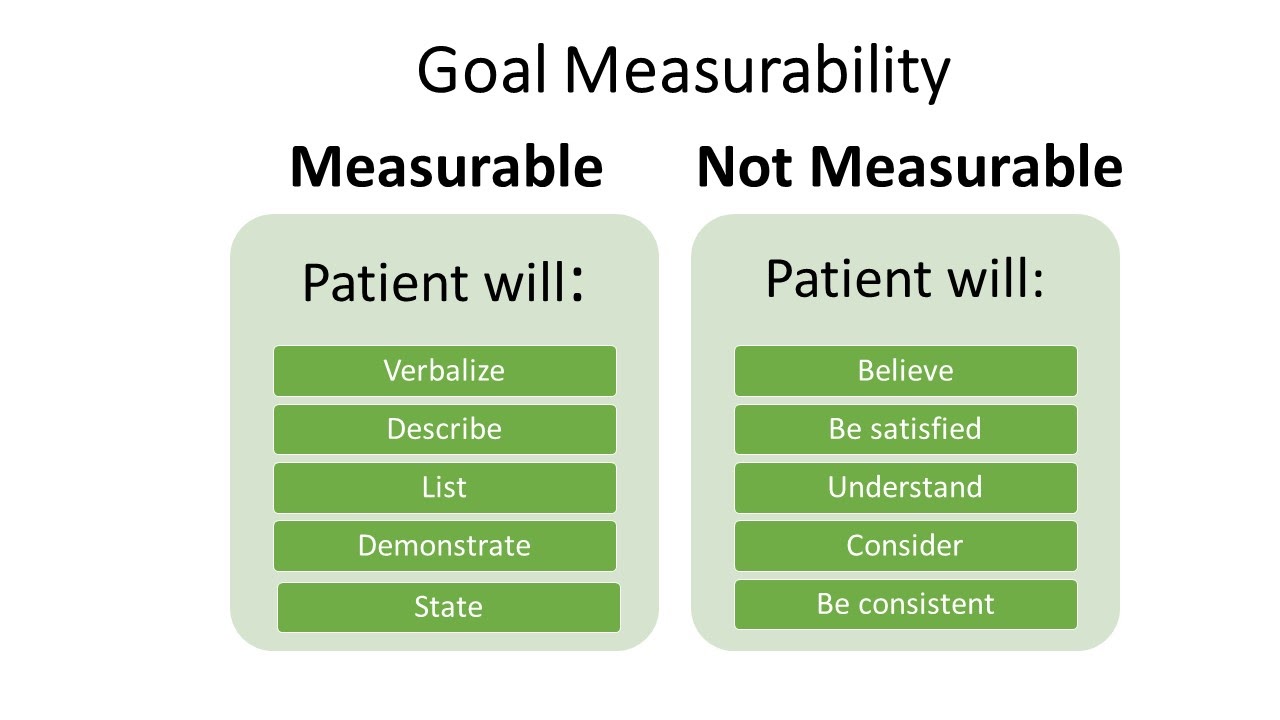
Examples of a non-measurable outcome revised to a measurable outcome is described in the following box.
Example
- Not measurable outcome: “The client will drink adequate fluid amounts every shift.”
- Revised into a measurable outcome: “The client will drink 24 ounces of fluids during every day shift (0600-1400).”
Action-Oriented and Attainable
Outcome statements should be written so that there is a clear action to be taken by the client or significant others. This means that the outcome statement should include a verb. Refer to Figure 4.11[8] for examples of action verbs.
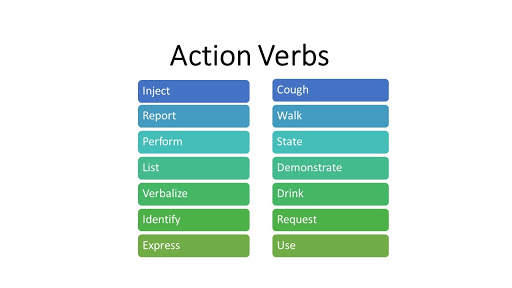
An example of a non-action-oriented outcome revised to an action-oriented outcome is provided in the following box.
Example
- Not action-oriented outcome: “The client will get increased physical activity.”
- Revised into an action-oriented outcome: “The client will list three types of aerobic activity that he would enjoy completing every week.”
Realistic and Relevant
Realistic outcomes consider the client’s physical and mental condition; their cultural and spiritual values, beliefs, and preferences; and their socioeconomic status in terms of their ability to attain these outcomes. Consideration should be also given to disease processes and the effects of conditions such as pain and decreased mobility on the client’s ability to reach expected outcomes. Other barriers to outcome attainment may be related to health literacy or lack of available resources. Outcomes should always be reevaluated and revised for attainability as needed. If an outcome is not attained, it is commonly because the original time frame was too ambitious, or the outcome was not realistic for the client.
See an example of how to revise an outcome that is not realistic into a realistic outcome in the following box.
Example
- Not realistic outcome: “The client will jog one mile every day when starting the exercise program.”
- Revised into a realistic outcome: “The client will walk ½ mile three times a week for two weeks.”
Time Limited
Outcome statements should include a time frame for evaluation. The time frame depends on the intervention and the client’s current condition. Some outcomes may need to be evaluated every shift, whereas other outcomes may be evaluated daily, weekly, or monthly. During the evaluation phase of the nursing process, the outcomes will be assessed according to the time frame specified for evaluation. If it has not been met, the nursing care plan should be revised.
See an example an outcome that is not time limited revised into a time limited outcome in the following box.
Example
- Not time limited: “The client will stop smoking cigarettes.”
- Time limited: “The client will complete the smoking cessation plan by December 12, 2025.“
Putting It Together
An example of a SMART outcome for Scenario C is provided in the following box.
Example of a SMART Expected Outcome
Refer to Scenario C in the “Assessment” section of this chapter. Ms. J.’s priority nursing diagnosis statement was Excess Fluid Volume related to excess fluid intake as manifested by bilateral basilar crackles in the lungs, bilateral 2+ pitting edema of the ankles and feet, an increase weight of ten pounds, and the client reports, “My ankles are so swollen.”
The broad goal was, “Ms. J. will achieve a state of fluid balance.”
An example of a SMART expected outcome to achieve this broad goal is, “The client will have clear bilateral lung sounds within the next 24 hours.”
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- Herdman, T. H., & Kamitsuru, S. (Eds.). (2018). Nursing diagnoses: Definitions and classification, 2018-2020. Thieme Publishers New York. ↵
- “Outcome Identification in the Nursing Process Compared to the NCJMM” by Tami Davis is licensed by CC BY 4.0 ↵
- Johnson, M., Moorhead, S., Bulechek, G., Butcher, H., Maas, M., & Swanson, E. (2012). NOC and NIC linkages to NANDA-I and clinical conditions: Supporting critical reasoning and quality care. Elsevier. ↵
- Campbell, J. (2020). SMART criteria. Salem Press Encyclopedia. ↵
- “SMART-goals.png” by Dungdm93 is licensed under CC BY-SA 4.0 ↵
- “Measurable Outcomes” by Valerie Palarski for Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- “Action Verbs” by Valerie Palarski for Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
A measurable behavior demonstrated by the client's response to nursing interventions
Broad statements of purpose that describe the aim of nursing care.
Statements of measurable action for the patient within a specific time frame and in response to nursing interventions. “SMART” outcome statements are specific, measurable, action-oriented, realistic, and include a time frame.

