Open Resources for Nursing (Open RN)
When completing a neurological assessment, it is important to understand the functions performed by different parts of the nervous system while analyzing findings. For example, damage to specific areas of the brain, such as that caused by a head injury or cerebrovascular accidents (i.e., strokes), can cause specific deficits in speech, facial movements, or use of the extremities. Damage to the spinal cord, such as that caused by a motor vehicle accident or diving accident, will cause specific motor and sensory deficits according to the level where the spinal cord was damaged.
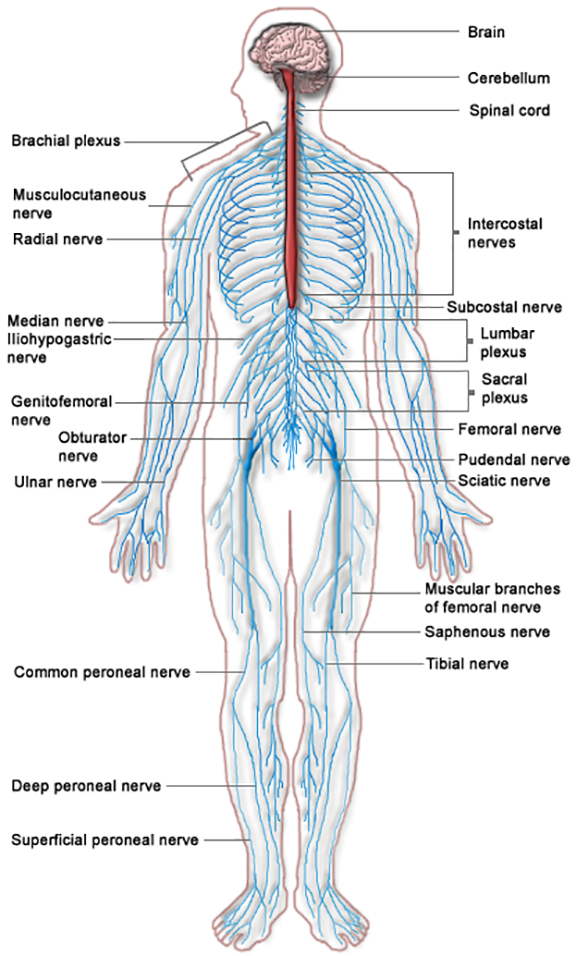
The nervous system is divided into two parts, the central nervous system and the peripheral nervous system. See Figure 6.1[1] for an image of the entire nervous system. The central nervous system (CNS) includes the brain and the spinal cord. The brain can be described as the interpretation center, and the spinal cord can be described as the transmission pathway. The peripheral nervous system (PNS) consists of the neurological system outside of the brain and spinal cord, including the cranial nerves that branch out from the brain and the spinal nerves that branch out from the spinal cord. The peripheral nervous system can be described as the communication network between the brain and the body parts. Both parts of the nervous system must work correctly for healthy body functioning.
Central Nervous System
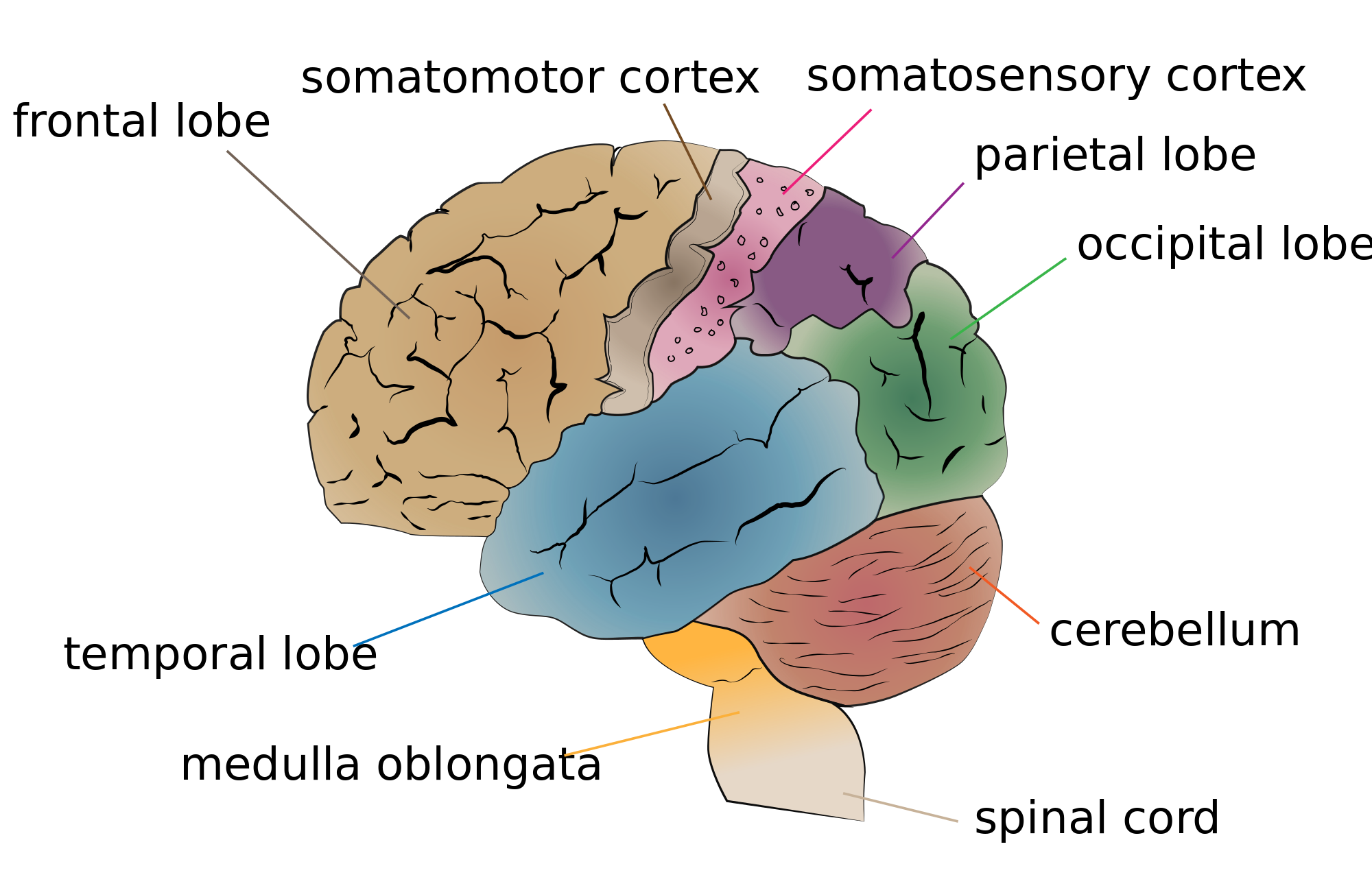
The major regions of the brain are the cerebrum and cerebral cortex, the diencephalon, the brain stem, and the cerebellum. See Figure 6.2[2] for an illustration of the cerebellum and the lobes of the cerebrum.
Cerebrum and Cerebral Cortex
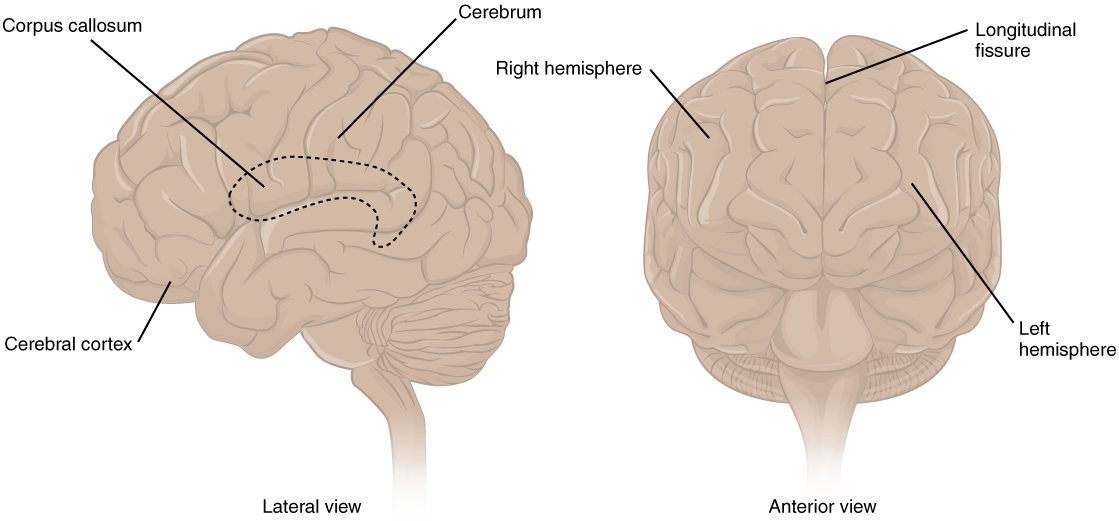
The largest portion of our brain is the cerebrum. The cerebrum is covered by a wrinkled outer layer of gray matter called the cerebral cortex. See Figure 6.3[3] for an image of the cerebral cortex. The cerebral cortex is responsible for the higher functions of the nervous system such as memory, emotion, and consciousness. The corpus callosum is the major pathway of communication between the right and left hemispheres of the cerebral cortex. The cerebral cortex is further divided into four lobes named the frontal, parietal, occipital, and temporal lobes.[4] Each lobe has specific functions.
Frontal Lobe
The frontal lobe is associated with movement because it contains neurons that instruct cells in the spinal cord to move skeletal muscles. The anterior portion of the frontal lobe is called the prefrontal lobe, and it provides cognitive functions such as planning and problem-solving that are the basis of our personality, short-term memory, and consciousness. Broca’s area is also located in the frontal lobe and is responsible for the production of language and controlling movements responsible for speech.[5]
Parietal Lobe
The parietal lobe processes general sensations from the body. All of the tactile senses are processed in this area, including touch, pressure, tickle, pain, itch, and vibration, as well as general senses of the body, such as proprioception (the sense of body position) and kinesthesia (the sense of movement).[6]
Temporal Lobe
The temporal lobe processes auditory information and is involved with language comprehension and production. Wernicke’s area and Broca’s area are located in the temporal lobe. Wernicke’s area is involved in the comprehension of written and spoken language, and Broca’s area is involved in the production of language. Because regions of the temporal lobe are part of the limbic system, memory is also an important function associated with the temporal lobe.[7] The limbic system is involved with our behavioral and emotional responses needed for survival, such as feeding, reproduction, and the fight – or – flight responses.
Occipital Lobe
The occipital lobe primarily processes visual information.[8]
Diencephalon
Information from the rest of the central and peripheral nervous system is sent to the cerebrum through the diencephalon, with the exception of the olfactory nerve that connects directly to the cerebrum.[9] See Figure 6.4[10] for an illustration of the diencephalon deep within the cerebrum. The diencephalon contains the hypothalamus and the thalamus.
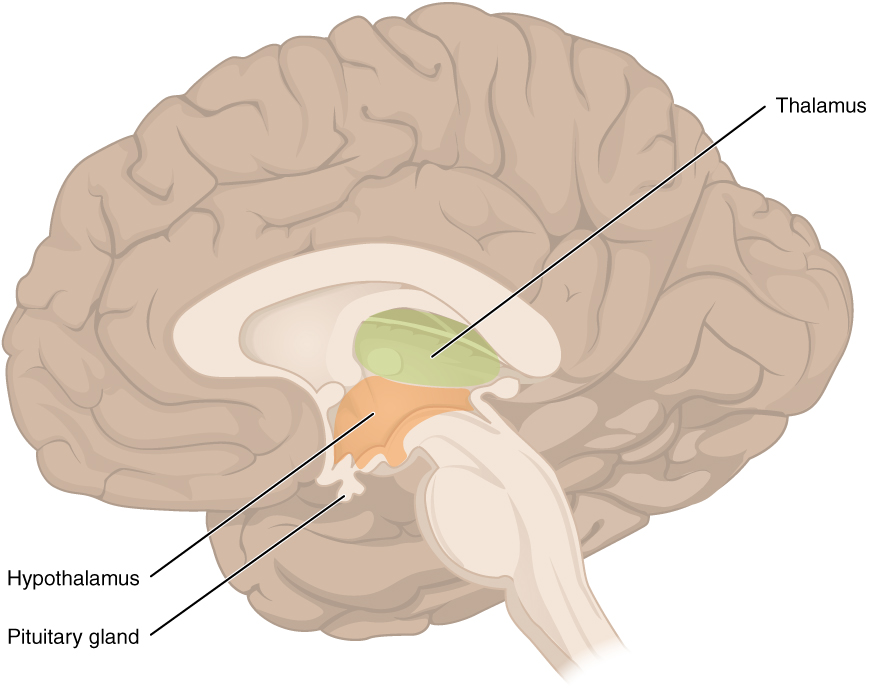
The hypothalamus helps regulate homeostasis such as body temperature, thirst, hunger, and sleep. The hypothalamus is also the executive region in charge of the autonomic nervous system and the endocrine system through its regulation of the anterior pituitary gland. Other parts of the hypothalamus are involved in memory and emotion as part of the limbic system.[11]
The thalamus relays sensory information and motor information in collaboration with the cerebellum. The thalamus does not just pass the information on, but it also processes and prioritizes that information. For example, the portion of the thalamus that receives visual information will influence what visual stimuli are considered important enough to receive further attention from the brain.[12]
Brain Stem
The brain stem is composed of the pons and the medulla. The pons and the medulla regulate several crucial autonomic functions in the body, including involuntary functions in the cardiovascular and respiratory systems, vasodilation, and reflexes like vomiting, coughing, sneezing, and swallowing. Cranial nerves also connect to the brain through the brain stem and provide sensory input and motor output.[13]
For more information about the functions of the autonomic nervous system, visit the “Autonomic Nervous System” chapter in the Open RN Nursing Pharmacology textbook.
Cerebellum
The cerebellum is located in the posterior part of the brain behind the brain stem and is responsible for fine motor movements and coordination. For example, when the motor neurons in the frontal lobe of the cerebral cortex send a command down the spinal cord to initiate walking, a copy of that instruction is also sent to the cerebellum. Sensory feedback from the muscles and joints, proprioceptive information about the movements of walking, and sensations of balance are sent back to the cerebellum. If the person becomes unbalanced while walking because the ground is uneven, the cerebellum sends out a corrective command to compensate for the difference between the original cerebral cortex command and the sensory feedback.[14]
Spinal Cord
The spinal cord is a continuation of the brain stem that transmits sensory and motor impulses. The length of the spinal cord is divided into regions that correspond to the level at which spinal nerves pass through the vertebrae. Immediately adjacent to the brain stem is the cervical region, followed by the thoracic, the lumbar, and finally the sacral region.[15] The spinal nerves in each of these regions innervate specific parts of the body. See more information under the “Spinal Nerves” subsection.
Review the anatomy of the brain using following supplementary video.
Review for Anatomy of the Brain on YouTube[16]
Peripheral Nervous System
The peripheral nervous system (PNS) consists of cranial nerves and spinal nerves that exist outside of the brain, spinal cord, and autonomic nervous system. The main function of the PNS is to connect the limbs and organs to the central nervous system (CNS). Sensory information from the body enters the CNS through cranial and spinal nerves. Cranial nerves are connected directly to the brain, whereas spinal nerves are connected to the brain via the spinal cord.
Peripheral nerves are classified as sensory nerves, motor nerves, or a combination of both. Sensory nerves carry impulses from the body to the brain for processing. Motor nerves transmit motor signals from the brain to the muscles to cause movement.
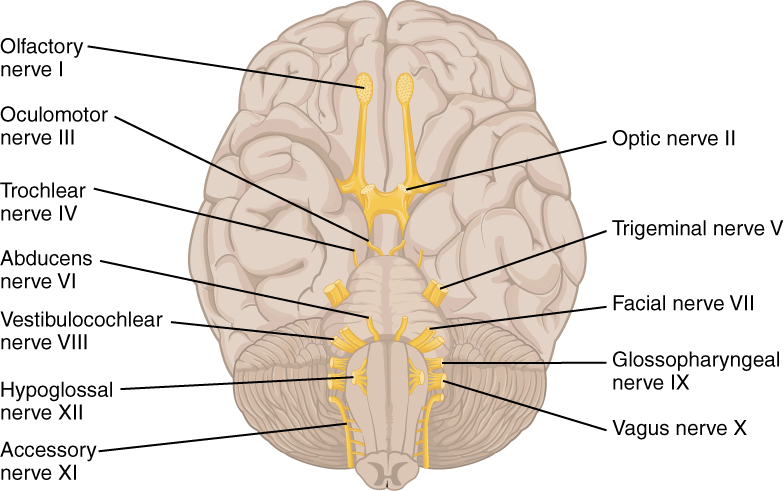
Cranial Nerves
Cranial nerves are directly connected from the periphery to the brain. They are primarily responsible for the sensory and motor functions of the head and neck. There are twelve cranial nerves that are designated by Roman numerals I through XII. See Figure 6.5[17] for an image of cranial nerves. Three cranial nerves are strictly sensory nerves; five are strictly motor nerves; and the remaining four are mixed nerves.[18] A traditional mnemonic for memorizing the names of the cranial nerves is “On Old Olympus Towering Tops A Finn And German Viewed Some Hops,” in which the initial letter of each word corresponds to the initial letter in the name of each nerve. A second popular mnemonic to assist with memorization is “Oh Once One Takes The Anatomy Final Very Good Vacations Are Heavenly”.
- The olfactory nerve is responsible for the sense of smell.
- The optic nerve is responsible for the sense of vision.
- The oculomotor nerve regulates eye movements by controlling four of the extraocular muscles, lifting the upper eyelid when the eyes point up and for constricting the pupils.
- The trochlear nerve and the abducens nerve are both responsible for eye movement but do so by controlling different extraocular muscles.
- The trigeminal nerve regulates skin sensations of the face and controls the muscles used for chewing.
- The facial nerve is responsible for the muscles involved in facial expressions, as well as part of the sense of taste and the production of saliva.
- The auditory/vestibulocochlear nerve manages hearing and balance.
- The glossopharyngeal nerve regulates the controlling muscles in the oral cavity and upper throat, as well as part of the sense of taste and the production of saliva.
- The vagus nerve is responsible for contributing to homeostatic control of the organs of the thoracic and upper abdominal cavities.
- The accessory nerve controls movements of the neck, along with cervical spinal nerves.
- The hypoglossal nerve manages the muscles of the lower throat and tongue.[19] Methods for assessing each of these nerves are described in the “Assessing Cranial Nerves” section.
Review of Cranial Nerves on YouTube[20]
Spinal Nerves
There are 31 spinal nerves that are named based on the level of the spinal cord where they emerge. See Figure 6.6[21] for an illustration of spinal nerves. There are eight pairs of cervical nerves designated C1 to C8, twelve thoracic nerves designated T1 to T12, five pairs of lumbar nerves designated L1 to L5, five pairs of sacral nerves designated S1 to S5, and one pair of coccygeal nerves. All spinal nerves are combined sensory and motor nerves. Spinal nerves extend outward from the vertebral column to innervate the periphery while also transmitting sensory information back to the CNS.[22]
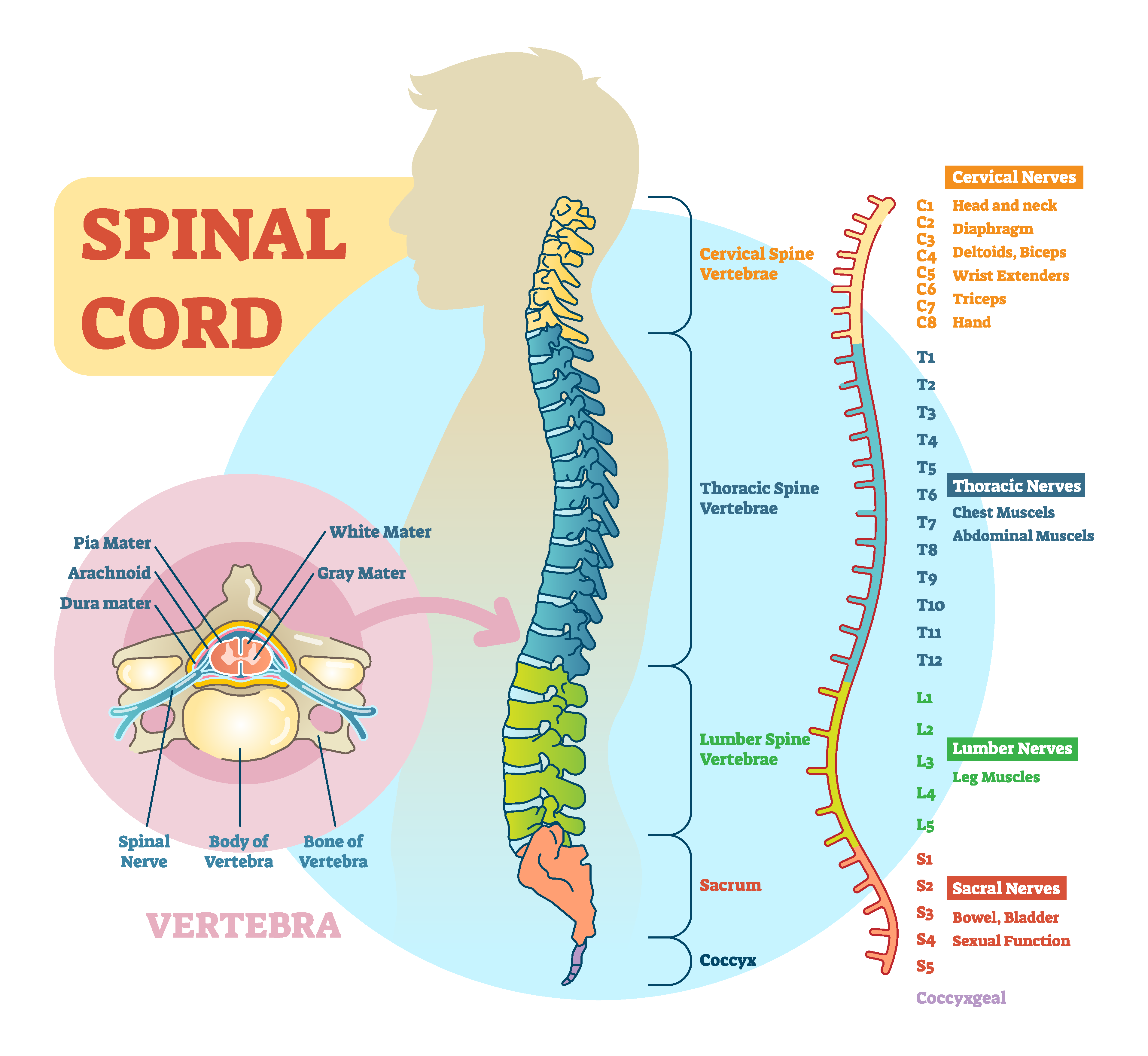
Functions of Spinal Nerves
Each spinal nerve innervates a specific region of the body:
- C1 provides motor innervation to muscles at the base of the skull.[23]
- C2 and C3 provide both sensory and motor control to the back of the head and behind the ears.[24]
- The phrenic nerve arises from nerve roots C3, C4, and C5. This is a vital nerve because it innervates the diaphragm to enable breathing. If a patient’s spinal cord is transected above C3 from an injury, then spontaneous breathing is not possible.[25]
- C5 through C8 and T1 combine to form the brachial plexus, a tangled array of nerves that serve the upper limbs and upper back.[26]
- The lumbar plexus arises from L1-L5 and innervates the pelvic region and the anterior leg.[27]
- The sacral plexus comes from the lower lumbar nerves L4 and L5 and the sacral nerves S1 to S4. The most significant systemic nerve to come from this plexus is the sciatic nerve. The sciatic nerve is associated with the painful medical condition sciatica, which is back and leg pain as a result of compression or irritation of the sciatic nerve.[28]
Functions of the Nervous System
The nervous system receives information about the environment around us (sensation) and generates responses to that information (motor responses). The process of integration combines sensory perceptions and higher cognitive functions such as memories, learning, and emotion while producing a response.
Sensation
Sensation is defined as receiving information about the environment. The major senses are taste, smell, touch, sight, and hearing. Additional sensory stimuli are also provided from inside the body, such as the stretch of an organ wall or the concentration of certain ions in the blood.[29]
Response
The nervous system produces a response based on the stimuli perceived by sensory nerves. For example, withdrawing a hand from a hot stove is an example of a response to a painfully hot stimulus. Responses can be classified by those that are voluntary (such as contraction of a skeletal muscle) and those that are involuntary (such as contraction of smooth muscle in the intestine). Voluntary responses are governed by the somatic nervous system, and involuntary responses are governed by the autonomic nervous system.[30]
Integration
Integration occurs when stimuli received by sensory nerves are communicated to the nervous system and the information is processed, leading to the generation of a conscious response. Consider this example of sensory integration. A batter in a baseball game does not automatically swing when they see the baseball thrown to them by the pitcher. First, the trajectory of the ball and its speed will need to be considered before creating the motor response of a swing. Then, integration will occur as the batter generates a conscious decision of whether to swing or not. Perhaps the count is three balls and one strike, and the batter decides to let this pitch go by in the hope of getting a walk to first base. Perhaps the batter is afraid to strike out and doesn’t swing, or maybe the batter learned the pitcher’s nonverbal cues the previous time at bat and is confident to take a swing at an anticipated fast ball. All of these considerations are included as part of the batter’s integration response and the higher-level functioning that occurs in the cerebral cortex.[31]
- “Nervous system diagram.png” by unknown is licensed under CC BY-NC-SA 3.0. Access for free at https://med.libretexts.org/Bookshelves/Nursing/Book%3A_Clinical_Procedures_for_Safer_Patient_Care_(Doyle_and_McCutcheon)/02%3A_Patient_Assessment/2.07%3A_Focused_Assessments ↵
- “Cerebrum lobes.svg” by Jkwchui is licensed under CC BY-SA 3.0 ↵
- “1305 CerebrumN.jpg” by OpenStax is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/13-2-the-central-nervous-system ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- “1310 Diencephalon.jpg” by OpenStax is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/13-2-the-central-nervous-system ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- Forciea, B. (2015, May 12). Anatomy and physiology: Central nervous system: Brain anatomy v2.0 [Video]. YouTube. All rights reserved. Video used with permission. https://youtu.be/DBRdInd2-Vg ↵
- “1320 The Cranial Nerves.jpg” by OpenStax is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/13-4-the-peripheral-nervous-system ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- Forciea, B. (2015, May 12). Anatomy and physiology: Nervous system: Cranial nerves (v2.0) [Video]. YouTube. All rights reserved. Video used with permission. https://youtu.be/JBEZh6CHogo ↵
- “1008694237-vector.png” by VectorMine on Shutterstock. All rights reserved. Imaged used with purchased permission. ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Anatomy and Physiology by Boundless.com and is licensed under CC BY-SA 4.0 ↵
- This work is a derivative of Anatomy and Physiology by Boundless.com and is licensed under CC BY-SA 4.0 ↵
- This work is a derivative of Anatomy and Physiology by Boundless.com and is licensed under CC BY-SA 4.0 ↵
- This work is a derivative of Anatomy and Physiology by Boundless.com and is licensed under CC BY-SA 4.0 ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
- This work is a derivative of Anatomy & Physiology by OpenStax and is licensed under CC BY 4.0. Access for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction ↵
Phases of Wound Healing
When skin is injured, there are four phases of wound healing that take place: hemostasis, inflammatory, proliferative, and maturation.[1] See Figure 20.1[2] for an illustration of the phases of wound healing.
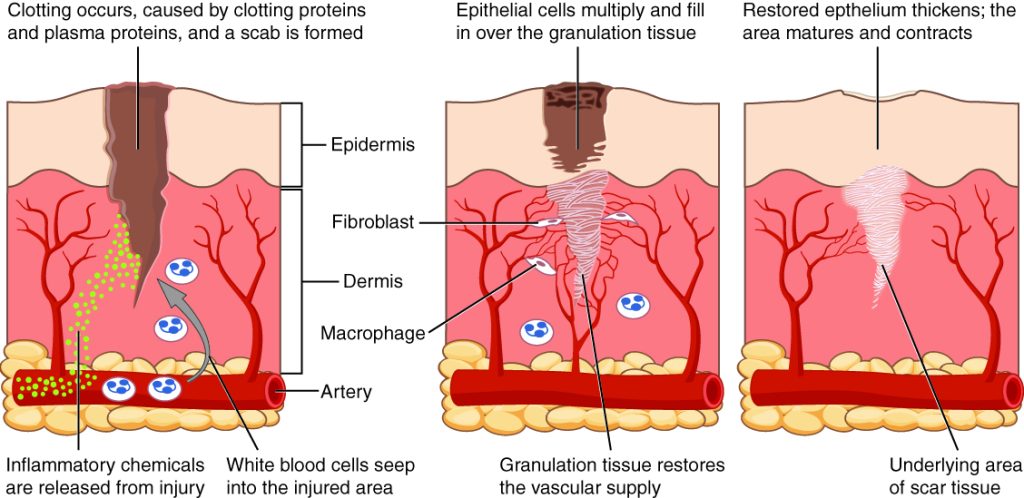
To illustrate the phases of wound healing, imagine that you accidentally cut your finger with a knife as you were slicing an apple. Immediately after the injury occurs, blood vessels constrict, and clotting factors are activated. This is referred to as the hemostasis phase. Clotting factors form clots that stop the bleeding and act as a barrier to prevent bacterial contamination. Platelets release growth factors that alert various cells to start the repair process at the wound location. The hemostasis phase lasts up to 60 minutes, depending on the severity of the injury.[3],[4]
After the hemostasis phase, the inflammatory phase begins. Vasodilation occurs so that white blood cells in the bloodstream can move into the wound to start cleaning the wound bed. The inflammatory process appears to the observer as edema (swelling), erythema (redness), and exudate. Exudate is fluid that oozes out of a wound, also commonly called pus.[5],[6]
The proliferative phase begins within a few days after the injury and includes four important processes: epithelialization, angiogenesis, collagen formation, and contraction. Epithelialization refers to the development of new epidermis and granulation tissue. Granulation tissue is new connective tissue with new, fragile, thin-walled capillaries. Collagen is formed to provide strength and integrity to the wound. At the end of the proliferation phase, the wound begins to contract in size.[7],[8]
Capillaries begin to develop within the wound 24 hours after injury during a process called angiogenesis. These capillaries bring more oxygen and nutrients to the wound for healing. When performing dressing changes, it is essential for the nurse to protect this granulation tissue and the associated new capillaries. Healthy granulation tissue appears pink due to the new capillary formation. It is also moist, painless to the touch, and may appear “bumpy.” Conversely, unhealthy granulation tissue is dark red and painful. It bleeds easily with minimal contact and may be covered by shiny white or yellow fibrous tissue referred to as biofilm that must be removed because it impedes healing. Unhealthy granulation tissue is often caused by an infection, so wound cultures should be obtained when infection is suspected. The provider can then prescribe appropriate antibiotic treatment based on the culture results.[9]
During the maturation phase, collagen continues to be created to strengthen the wound. Collagen contributes strength to the wound to prevent it from reopening. A wound typically heals within 4-5 weeks and often leaves behind a scar. The scar tissue is initially firm, red, and slightly raised from the excess collagen deposition. Over time, the scar begins to soften, flatten, and become pale in about nine months.[10]
Types of Wound Healing
There are three types of wound healing: primary intention, secondary intention, and tertiary intention. Healing by primary intention means that the wound is sutured, stapled, glued, or otherwise closed so the wound heals beneath the closure. This type of healing occurs with clean-edged lacerations or surgical incisions, and the closed edges are referred to as approximated. See Figure 20.2[11] for an image of a surgical wound healing by primary intention.

Secondary intention occurs when the edges of a wound cannot be approximated (brought together), so the wound fills in from the bottom up by the production of granulation tissue. Examples of wounds that heal by secondary intention are pressure injuries and chainsaw injuries. Wounds that heal by secondary intention are at higher risk for infection and must be protected from contamination. See Figure 20.3[12] for an image of a wound healing by secondary intention.

Tertiary intention refers to a wound that has had to remain open or has been reopened, often due to severe infection. The wound is typically closed at a later date when infection has resolved. Wounds that heal by secondary and tertiary intention have delayed healing times and increased scar tissue.
Wound Closures
Lacerations and surgical wounds are typically closed with sutures, staples, or dermabond to facilitate healing by primary intention. See Figure 20.4[13] for an image of sutures, Figure 20.5[14] for an image of staples, and Figure 20.6[15] for an image of a wound closed with dermabond, a type of sterile surgical glue. Based on agency policy, the nurse may remove sutures and staples based on a provider order. See Figure 20.7[16] for an image of a disposable staple remover. See the checklists in the subsections later in this chapter for procedures related to surgical and staple removal.




Common Types of Wounds
There are several different types of wounds. It is important to understand different types of wounds when providing wound care because each type of wound has different characteristics and treatments. Additionally, treatments that may be helpful for one type of wound can be harmful for another type. Common types of wounds include skin tears, venous ulcers, arterial ulcers, diabetic foot wounds, and pressure injuries.[17]
Skin Tears
Skin tears are wounds caused by mechanical forces such as shear, friction, or blunt force. They typically occur in the fragile, nonelastic skin of older adults or in patients undergoing long-term corticosteroid therapy. Skin tears can be caused by the simple mechanical force used to remove an adhesive bandage or from friction as the skin brushes against a surface. Skin tears occur in the epidermis and dermis but do not extend through the subcutaneous layer. The wound bases of skin tears are typically fragile and bleed easily.[18]
Venous Ulcers
Venous ulcers are caused by lack of blood return to the heart causing pooling of fluid in the veins of the lower legs. The resulting elevated hydrostatic pressure in the veins causes fluid to seep out, macerate the skin, and cause venous ulcerations. Maceration refers to the softening and wasting away of skin due to excess fluid. Venous ulcers typically occur on the medial lower leg and have irregular edges due to the maceration. There is often a dark-colored discoloration of the lower legs, due to blood pooling and leakage of iron into the skin called hemosiderin staining. For venous ulcers to heal, compression dressings must be used, along with multilayer bandage systems, to control edema and absorb large amounts of drainage.[19] See Figure 20.8[20] for an image of a venous ulcer.

Arterial Ulcers
Arterial ulcers are caused by lack of blood flow and oxygenation to tissues. They typically occur in the distal areas of the body such as the feet, heels, and toes. Arterial ulcers have well-defined borders with a “punched out” appearance where there is a localized lack of blood flow. They are typically painful due to the lack of oxygenation to the area. The wound base may become necrotic (black) due to tissue death from ischemia. Wound dressings must maintain a moist environment, and treatment must include the removal of necrotic tissue. In severe arterial ulcers, vascular surgery may be required to reestablish blood supply to the area.[21] See Figure 20.9[22] for an image of an arterial ulcer on a patient’s foot.

Diabetic Ulcers
Diabetic ulcers are also called neuropathic ulcers because peripheral neuropathy is commonly present in patients with diabetes. Peripheral neuropathy is a medical condition that causes decreased sensation of pain and pressure, especially in the lower extremities. Diabetic ulcers typically develop on the plantar aspect of the feet and toes of a patient with diabetes due to lack of sensation of pressure or injury. See Figure 20.10[23] for an image of a diabetic ulcer. Wound healing is compromised in patients with diabetes due to the disease process. In addition, there is a higher risk of developing an infection that can reach the bone requiring amputation of the area. To prevent diabetic ulcers from occurring, it is vital for nurses to teach meticulous foot care to patients with diabetes and encourage the use of well-fitting shoes.[24]

Pressure Injuries
Pressure injuries are defined as “localized damage to the skin or underlying soft tissue, usually over a bony prominence, as a result of intense and prolonged pressure in combination with shear.”[25] Shear occurs when tissue layers move over the top of each other, causing blood vessels to stretch and break as they pass through the subcutaneous tissue. For example, when a patient slides down in bed, the outer skin remains immobile because it remains attached to the sheets due to friction, but deeper tissue attached to the bone moves as the patient slides down. This opposing movement of the outer layer of skin and the underlying tissues causes the capillaries to stretch and tear, which then impacts the blood flow and oxygenation of the surrounding tissues.
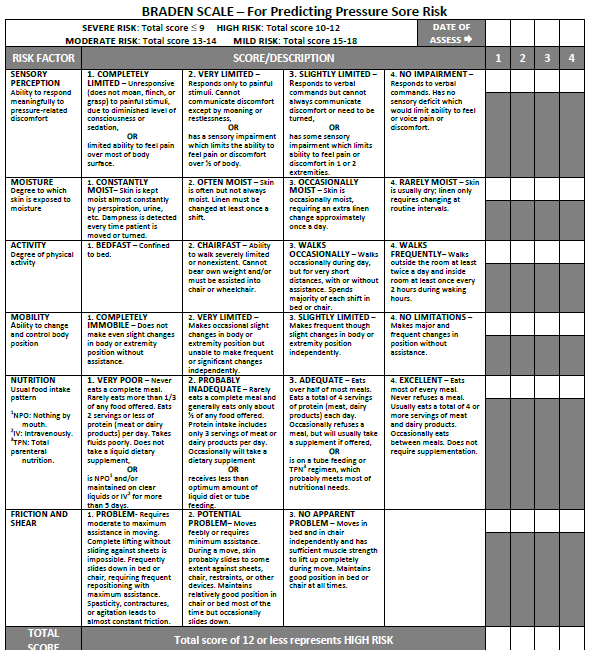
Braden Scale
Several factors place a patient at risk for developing pressure injuries, including nutrition, mobility, sensation, and moisture. The Braden Scale is a tool commonly used in health care to provide an objective assessment of a patient’s risk for developing pressure injuries. See Figure 20.11[26] for an image of a Braden Scale. The six risk factors included on the Braden Scale are sensory perception, moisture, activity, mobility, nutrition, and friction/shear, and these factors are rated on a scale from 1-4 with 1 being “completely limited” to 4 being “no impairment.” The scores from the six categories are added, and the total score indicates a patient’s risk for developing a pressure injury. A total score of 15-19 indicates mild risk, 13-14 indicates moderate risk, 10-12 indicates high risk, and less than or equal to 9 indicates severe risk. Nurses create care plans using these scores to plan interventions that prevent or treat pressure injuries.
For more information about using the Braden Scale, go to the “Integumentary” chapter of the Open RN Nursing Fundamentals textbook.
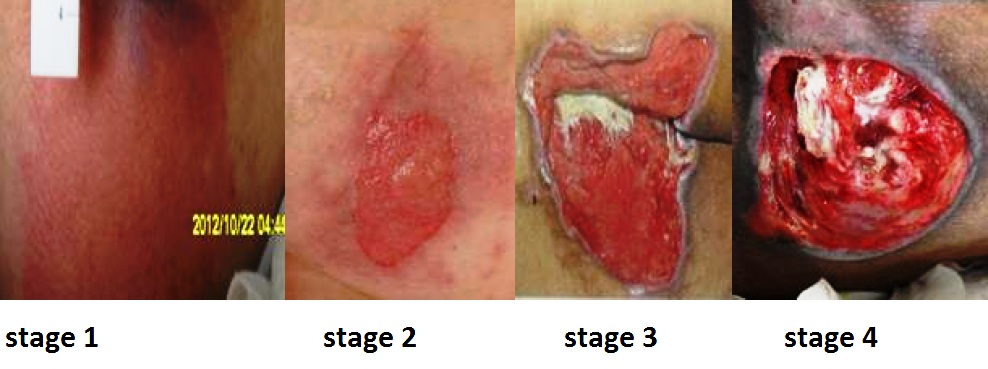
Staging
Pressure injuries commonly occur on the sacrum, heels, ischial tuberosity, and coccyx. The 2016 National Pressure Ulcer Advisory Panel (NPUAP) Pressure Injury Staging System now uses the term “pressure injury” instead of pressure ulcer because an injury can occur without an ulcer present. Pressure injuries are staged from 1 through 4 based on the extent of tissue damage. For example, Stage 1 pressure injuries have reddened but intact skin, and Stage 4 pressure injuries have deep, open ulcers affecting underlying tissue and structures such as muscles, ligaments, and tendons. See Figure 20.12[27] for an image of the four stages of pressure injuries.[28] The NPUAP’s definitions of the four stages of pressure injuries are described below:
- Stage 1 pressure injuries are intact skin with a localized area of nonblanchable erythema where prolonged pressure has occurred. Nonblanchable erythema is a medical term used to describe skin redness that does not turn white when pressed.
- Stage 2 pressure injuries are partial-thickness loss of skin with exposed dermis. The wound bed is viable and may appear like an intact or ruptured blister. Stage 2 pressure injuries heal by reepithelialization and not by granulation tissue formation.[29]
- Stage 3 pressure injuries are full-thickness tissue loss in which fat is visible, but cartilage, tendon, ligament, muscle, and bone are not exposed. The depth of tissue damage varies by anatomical location. Undermining and tunneling may occur in Stage 3 and 4 pressure injuries. Undermining occurs when the tissue under the wound edges becomes eroded, resulting in a pocket beneath the skin at the wound's edge. Tunneling refers to passageways underneath the surface of the skin that extend from a wound and can take twists and turns. Slough and eschar may also be present in Stage 3 and 4 pressure injuries. Slough is an inflammatory exudate that is usually light yellow, soft, and moist. Eschar is dark brown/black, dry, thick, and leathery dead tissue. See Figure 20.13 [30] for an image of eschar in the center of the wound. If slough or eschar obscures the wound so that tissue loss cannot be assessed, the pressure injury is referred to as unstageable.[31] In most wounds, slough and eschar must be removed by debridement for healing to occur.
- Stage 4 pressure injuries are full-thickness tissue loss like Stage 3 pressure injuries, but also have exposed cartilage, tendon, ligament, muscle, or bone. Osteomyelitis (bone infection) may be present.[32]

View a supplementary YouTube video on Pressure Injuries[33]
Factors Affecting Wound Healing
Multiple factors affect a wound’s ability to heal and are referred to as local and systemic factors. Local factors refer to factors that directly affect the wound, whereas systemic factors refer to the overall health of the patient and their ability to heal. Local factors include localized blood flow and oxygenation of the tissue, the presence of infection or a foreign body, and venous sufficiency. Venous insufficiency is a medical condition where the veins in the legs do not adequately send blood back to the heart, resulting in a pooling of fluids in the legs.[34]
Systemic factors that affect a patient’s ability to heal include nutrition, mobility, stress, diabetes, age, obesity, medications, alcohol use, and smoking.[35] When a nurse is caring for a patient with a wound that is not healing as anticipated, it is important to further assess for the potential impact of these factors:
- Nutrition. Nutritional deficiencies can have a profound impact on healing and must be addressed for chronic wounds to heal. Protein is one of the most important nutritional factors affecting wound healing. For example, in patients with pressure injuries, 30 to 35 kcal/kg of calorie intake with 1.25 to 1.5g/kg of protein and micronutrients supplementation is recommended daily.[36] In addition, vitamin C and zinc deficiency have many roles in wound healing. It is important to collaborate with a dietician to identify and manage nutritional deficiencies when a patient is experiencing poor wound healing.[37]
- Stress. Stress causes an impaired immune response that results in delayed wound healing. Although a patient cannot necessarily control the amount of stress in their life, it is possible to control one’s reaction to stress with healthy coping mechanisms. The nurse can help educate the patient about healthy coping strategies.
- Diabetes. Diabetes causes delayed wound healing due to many factors such as neuropathy, atherosclerosis (a buildup of plaque that obstructs blood flow in the arteries resulting in decreased oxygenation of tissues), a decreased host immune resistance, and increased risk for infection.[38] Read more about neuropathy and diabetic ulcers under the “Common Types of Wounds” subsection. Nurses provide vital patient education to patients with diabetes to effectively manage the disease process for improved wound healing.
- Age. Older adults have an altered inflammatory response that can impair wound healing. Nurses can educate patients about the importance of exercise for improved wound healing in older adults.[39]
- Obesity. Obese individuals frequently have wound complications, including infection, dehiscence, hematoma formation, pressure injuries, and venous injuries. Nurses can educate patients about healthy lifestyle choices to reduce obesity in patients with chronic wounds.[40]
- Medications. Medications such as corticosteroids impair wound healing due to reduced formation of granulation tissue.[41] When assessing a chronic wound that is not healing as expected, it is important to consider the side effects of the patient’s medications.
- Alcohol consumption. Research shows that exposure to alcohol impairs wound healing and increases the incidence of infection.[42] Patients with impaired healing of chronic wounds should be educated to avoid alcohol consumption.
- Smoking. Smoking impacts the inflammatory phase of the wound healing process, resulting in poor wound healing and an increased risk of infection.[43] Patients who smoke should be encouraged to stop smoking.
Lab Values Affecting Wound Healing
When a chronic wound is not healing as expected, laboratory test results may provide additional clues regarding the causes of the delayed healing. See Table 20.2 for lab results that offer clues to systemic issues causing delayed wound healing.[44]
Table 20.2 Lab Values Associated with Delayed Wound Healing[45]
| Abnormal Lab Value | Rationale |
|---|---|
| Low hemoglobin | Low hemoglobin indicates less oxygen is transported to the wound site. |
| Elevated white blood cells (WBC) | Increased WBC indicates infection is occurring. |
| Low platelets | Platelets are important during the proliferative phase in the creation of granulation tissue and angiogenesis.[46] |
| Low albumin | Low albumin indicates decreased protein levels. Protein is required for effective wound healing. |
| Elevated blood glucose or hemoglobin A1C | Elevated blood glucose and hemoglobin A1C levels indicate poor management of diabetes mellitus, a disease that impacts wound healing. |
| Elevated serum BUN and creatinine | BUN and creatinine levels are indicators of kidney function, with elevated levels indicating worsening kidney function. Elevated BUN (blood urea nitrogen) levels impact wound healing. |
| Positive wound culture | Positive wound cultures indicate an infection is present and provide additional information, including the type and number of bacteria present, as well as identifying antibiotics to which the bacteria is susceptible. The nurse reviews this information when administering antibiotics to ensure the prescribed therapy is effective for the type of bacteria present. |
Wound Complications
In addition to delayed wound healing, several other complications can occur. Three common complications are the development of a hematoma, infection, or dehiscence. These complications should be immediately reported to the health care provider.
Hematoma
A hematoma is an area of blood that collects outside of the larger blood vessels. A hematoma is more severe than ecchymosis (bruising) that occurs when small veins and capillaries under the skin break. The development of a hematoma at a surgical site can lead to infection and incisional dehiscence.[47] See Figure 20.14[48] for an image of a hematoma.

Infection
A break in the skin allows bacteria to enter and begin to multiply. Microbial contamination of wounds can progress from localized infection to systemic infection, sepsis, and subsequent life- and limb-threatening infection. Signs of a localized wound infection include redness, warmth, and tenderness around the wound. Purulent or malodorous drainage may also be present. Signs that a systemic infection is developing and requires urgent medical management include the following[49]:
- Fever over 101 F (38 C)
- Overall malaise (lack of energy and not feeling well)
- Change in level of consciousness/increased confusion
- Increasing or continual pain in the wound
- Expanding redness or swelling around the wound
- Loss of movement or function of the wounded area
Dehiscence
Dehiscence refers to the separation of the edges of a surgical wound. A dehisced wound can appear fully open where the tissue underneath is visible, or it can be partial where just a portion of the wound has torn open. Wound dehiscence is always a risk in a surgical wound, but the risk increases if the patient is obese, smokes, or has other health conditions, such as diabetes, that impact wound healing. Additionally, the location of the wound and the amount of physical activity in that area also increase the chances of wound dehiscence.[50] See Figure 20.15[51] for an image of dehiscence in an abdominal surgical wound in a 50-year-old obese female with a history of smoking and malnutrition.
Wound dehiscence can occur suddenly, especially in abdominal wounds when the patient is coughing or straining. Evisceration is a rare but severe surgical complication when dehiscence occurs, and the abdominal organs protrude out of the incision. Signs of impending dehiscence include redness around the wound margins and increasing drainage from the incision. The wound will also likely become increasingly painful. Suture breakage can be a sign that the wound has minor dehiscence or is about to dehisce.[52]
To prevent wound dehiscence, surgical patients must follow all post-op instructions carefully. The patient must move carefully and protect the skin from being pulled around the wound site. They should also avoid tensing the muscles surrounding the wound and avoid heavy lifting as advised.[53]

Wounds should be assessed and documented at every dressing change. Wound assessment should include the following components:
- Anatomic location
- Type of wound (if known)
- Degree of tissue damage
- Wound bed
- Wound size
- Wound edges and periwound skin
- Signs of infection
- Pain[54]
These components are further discussed in the following sections.
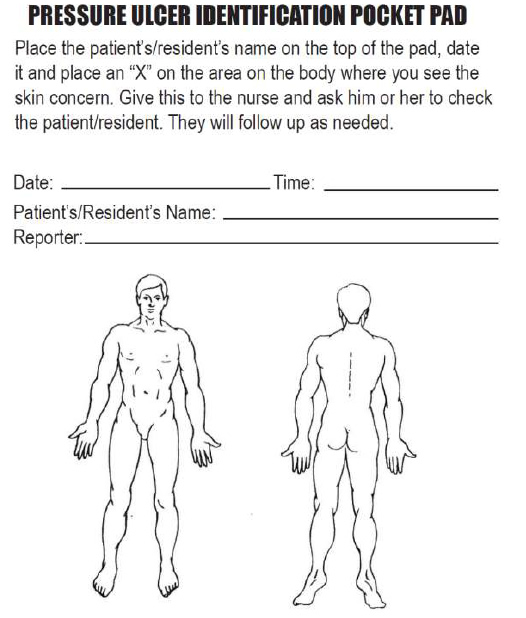
Anatomic Location and Type of Wound
The location of the wound should be documented clearly using correct anatomical terms and numbering. This will ensure that if more than one wound is present, the correct one is being assessed and treated. Many agencies use images to facilitate communication regarding the location of wounds among the health care team. See Figure 20.16[55] for an example of facility documentation that includes images to indicate wound location.
The location of a wound also provides information about the cause and type of a wound. For example, a wound over the sacral area of an immobile patient is likely a pressure injury, and a wound near the ankle of a patient with venous insufficiency is likely a venous ulcer. For successful healing, different types of wounds require different treatments based on the cause of the wound.
Degree of Tissue Damage
It is important to continually assess the degree of tissue damage in pressure injuries because the level of damage can worsen if they are not treated appropriately. Refer to the “Staging” subsection of “Pressure Injuries” in the “Basic Concepts Related to Wounds” section for more information about tissue damage.
Wound Base
Assess the color of the wound base. Recall that healthy granulation tissue appears pink due to the new capillary formation. It is moist, painless to the touch, and may appear “bumpy.” Conversely, unhealthy granulation tissue is dark red and painful. It bleeds easily with minimal contact and may be covered with biofilm. The appearance of slough (yellow) or eschar (black) in the wound base should be documented and communicated to the health care provider because it likely will need to be removed for healing. Tunneling and undermining should also be assessed, documented, and communicated.
Type and Amount of Exudate
The color, consistency, and amount of exudate (drainage) should be assessed and documented at every dressing change. The amount of drainage from wounds is categorized as scant, small/minimal, moderate, or large/copious. Use the following descriptions to select the appropriate terms[56]:
- No exudate: The wound base is dry.
- Scant amount of exudate: The wound is moist, but no measurable amount of exudate appears on the dressing.
- Minimal amount of exudate: Exudate covers less than 25% of the size of the bandage.
- Moderate amount of drainage: Wound tissue is wet, and drainage covers 25% to 75% of the size of the bandage.
- Large or copious amount of drainage: Wound tissue is filled with fluid, and exudate covers more than 75% of the bandage.[57]
The type of wound drainage should be described using medical terms such as serosanguinous, sanguineous, serous, or purulent.
- Sanguineous: Sanguineous exudate is fresh bleeding.[58]
- Serous: Serous drainage is clear, thin, watery plasma. It’s normal during the inflammatory stage of wound healing, and small amounts are considered normal wound drainage.[59]
- Serosanguinous: Serosanguineous exudate contains serous drainage with small amounts of blood present.[60]
- Purulent: Purulent exudate is thick and opaque. It can be tan, yellow, green, or brown. It is never considered normal in a wound bed, and new purulent drainage should always be reported to the health care provider.[61] See Figure 20.17[62] for an image of purulent drainage.

Wound Size
Wounds should be measured on admission and during every dressing change to evaluate for signs of healing. Accurate wound measurements are vital for monitoring wound healing. Measurements should be taken in the same manner by all clinicians to maintain consistent and accurate documentation of wound progress. This can be difficult to accomplish with oddly shaped wounds because there can be confusion about how consistently to measure them. Wounds should be described by length by width, with the length of the wound based on the head-to-toe axis. The width of a wound should be measured from side to side laterally. If a wound is deep, the deepest point of the wound should be measured to the wound surface using a sterile, cotton-tipped applicator. Many facilities use disposable, clear plastic measurement tools to measure the area of a wound healing by secondary intention. Measurements are typically documented in centimeters. See Figure 20.18[63] for an image of a wound measurement tool.
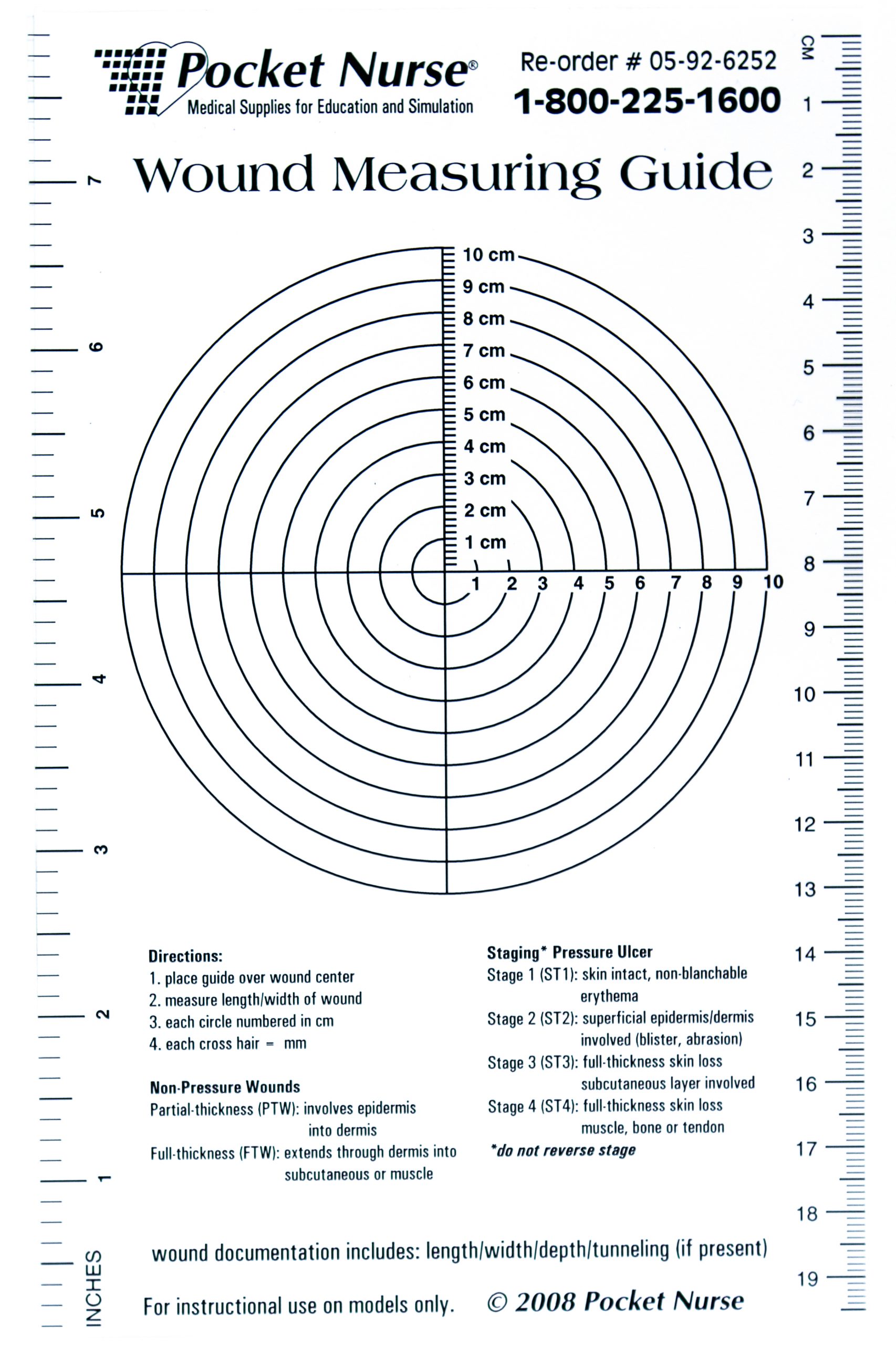
Tunneling can occur in a full-thickness wound that can lead to abscess formation. The depth of a tunneling can be measured by gently probing the tunneled area with a sterile, cotton-tipped applicator from the wound base to the end of the tract. When probing a tunnel, it is imperative to not force the swab but only insert until resistance is felt to prevent further damage to the area. The location of the tunnel in the wound should be documented using the analogy of a clock face, with 12:00 pointing toward the patient’s head.[64]
Undermining occurs when the tissue under the wound edges becomes eroded, resulting in a pocket beneath the skin at the wound's edge. Undermining is measured by inserting a probe under the wound edge directed almost parallel to the wound surface until resistance is felt. The amount of undermining is the distance from the probe tip to the point at which the probe is level with the wound edge. Clock terms are also used to identify the area of undermining.[65]
Wound Edges and Periwound Skin
If the wound is healing by primary intention, it should be documented if the wound edges are well-approximated (closed together) or if there are any signs of dehiscence. The skin outside the outer edges of the wound, called the periwound skin, provides information related to wound development or healing. For example, a venous ulcer often has excess wound drainage that macerates the periwound skin, giving it a wet, waterlogged appearance that is soft and grayish white in color.[66] See Figure 20.19[67] for an image of erythematous periwound with partial dehiscence.

Signs of Infection
Wounds should be continually monitored for signs of infection. Signs of localized wound infection include erythema (redness), induration (area of hardened tissue), pain, edema, purulent exudate (yellow or green drainage), and wound odor.[68] New signs of infection should be reported to the health care provider with an anticipated order for a wound culture.
Pain
The intensity of pain that a patient is experiencing with a wound should be assessed and documented. If a patient experiences pain during dressing changes, it should be managed with administration of pain medication before scheduled dressing changes. Be aware that the degree of pain may not correlate to the extent of tissue damage. For example, skin tears are often painful because the nerve endings are exposed in the dermal layer, whereas patients with severe diabetic ulcers on their feet may experience little or no pain because of existing neuropathic damage.[69]
Wound therapy is often prescribed by a multidisciplinary team that can include the provider, a wound care nurse, a dietician, and the bedside nurse who performs dressing changes. Topical dressings should be selected that create an environment conducive to healing the specific type of wound and its causes. It is important to perform the following actions when providing wound care:
- Prevent and manage infection
- Cleanse the wound
- Debride the wound
- Maintain appropriate moisture in the wound
- Control odor
- Manage wound pain
- Consider the big picture[70]
Each of these objectives is further discussed in the following subsections.
Prevent and Manage Infection
One of the primary goals of wound dressings is to protect the wound base from bacteria and contaminants (i.e., urine and feces). If new signs of infection are present during a wound dressing change, wound swabs should be taken according to agency policy and the need for a wound culture and possible antibiotic therapy discussed with the primary provider.[71]
Silver sulfadiazine is an example of a common topical antibiotic prescribed for wounds. Topical antibiotics are covered with a secondary dressing.[72]
Cleanse the Wound
Routine cleansing should be performed at each dressing change with products that are physiologically compatible with wound tissue. Normal saline is the most gentle solution and is typically delivered using a syringe or commercial cleansers. See Figure 20.20[73] for an image of wound irrigation with a syringe. Commercial cleansers may be used, but hydrogen peroxide, betadine, and acetic acid should be avoided because these agents can be cytotoxic.[74]

Debride the Wound
Debridement is the removal of nonviable tissue in a wound. If necrotic (black) tissue is present in the wound bed, it must be removed in most circumstances for the wound to heal. However, one exception is stable, dry eschar on a patient’s heel that should be left in place until the patient’s vascular status is determined.[75]
Wound debridement can be accomplished using several methods, such as autolytic, enzymatic, or sharp wound debridement. Autolytic debridement occurs when moist topical dressings foster the breakdown of necrotic tissue. Enzymatic debridement occurs when prescribed topical agents are directly applied to the wound bed.[76] Collagenase ointment is an example of a topical enzymatic debridement ointment that is applied daily (or more frequently if the dressing becomes soiled) and covered with sterile gauze or a foam dressing.[77] Sharp wound debridement is performed by a trained health care provider and may be at the bedside or in the operating room. Sharp debridement is an invasive procedure using a scalpel or scissors to remove necrotic tissue so that only viable tissue remains. See Figure 20.21[78] for an image of a wound that has been surgically debrided of necrotic tissue.

Maintain Appropriate Moisture in the Wound
Wound dressings should maintain a moist wound environment to facilitate the development of granulation tissue. However, excessive exudate must be managed with dressings that absorb excess moisture to avoid maceration of the surrounding tissue.[79] For example, dressings such as alginate or hydrofiber are used in wounds with large amounts of exudate to maintain an appropriate moisture level but also prevent maceration of tissue. Frequent dressing changes may also be required in wounds with heavy drainage.
Eliminate Dead Space
Deep wounds and tunneling should be packed with dressings to keep the wound bed moist. Sterile gauze dressings moistened with normal saline or hydrogel-impregnated dressings are examples of packing agents used to keep the wound bed moist. Packing material should be easy to remove from the wound base during each dressing change to avoid injuring the fragile granulation tissue. Keep in mind that dressings made of alginate have a slight greenish tint when removed and should not be confused with purulent drainage.
Control Odor
If odor is present in a wound, the nurse should consult with the health care provider about the frequency of dressing changes, wound cleansing agents, and the possible need for topical antimicrobial therapy or debridement. Room deodorants can be obtained for use after dressing changes.[80]
Manage Wound Pain
Wounds that are becoming increasingly painful should be assessed for potential infection or dehiscence. The nurse should plan on administering medication to the patient before performing dressing changes on wounds that are painful. If pain medication is not ordered, then the nurse should contact the health care provider for a prescription before performing the dressing change.[81]
Protect Periwound Skin
Heavily draining wounds or the improper use of moist dressings can cause maceration of the periwound skin. The nurse should apply dressings carefully to maintain wound bed moisture yet also protect the periwound skin. Skin barrier creams, skin protective wipes, or skin barrier wafers can also be used to protect the periwound skin.[82]
Consider the Big Picture
Most wounds do not occur in isolation but also have other systemic or local factors that impact wound healing. Be sure to consider the following points when caring for patients with wounds with delayed wound healing:
- Minimize pressure and shear for patients with pressure injuries. For example, a patient with a pressure injury should be repositioned at least every two hours to minimize pressure.
- Educate patients with neuropathy and decreased sensation about preventing further injury. For example, a patient with diabetes should wear well-fitting shoes and never go barefoot to prevent injuries.
- Control edema in patients with venous ulcers through the use of compression dressings.
- Promote adequate perfusion to patients with arterial ulcers. For example, in most cases, the extremity of a patient with an arterial ulcer should not be elevated.
- Protect fragile skin in patients with skin tears to prevent further injury.
- Manage blood sugar levels in patients with diabetes mellitus for optimal healing.
- Promote good nutrition and hydration for all patients with wounds. Consult a registered dietician to assess the patient’s nutritional status and develop a nutrition plan if needed.[83]
- Document ongoing assessment findings and wound interventions for good communication and continuity of care across the multidisciplinary health care team.
- Concerns about the healing of a chronic wound or the dressings ordered should be communicated to the health care provider. Referral to a specialized wound care nurse is often helpful.

