Open Resources for Nursing (Open RN)
A thorough assessment of the heart provides valuable information about the function of a patient’s cardiovascular system. Understanding how to properly assess the cardiovascular system and identifying both normal and abnormal assessment findings will allow the nurse to provide quality, safe care to the patient.
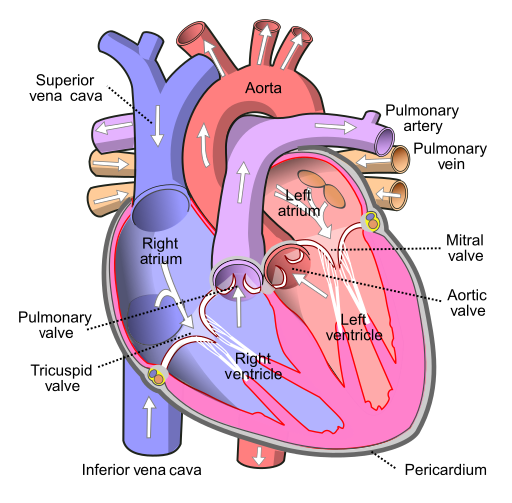
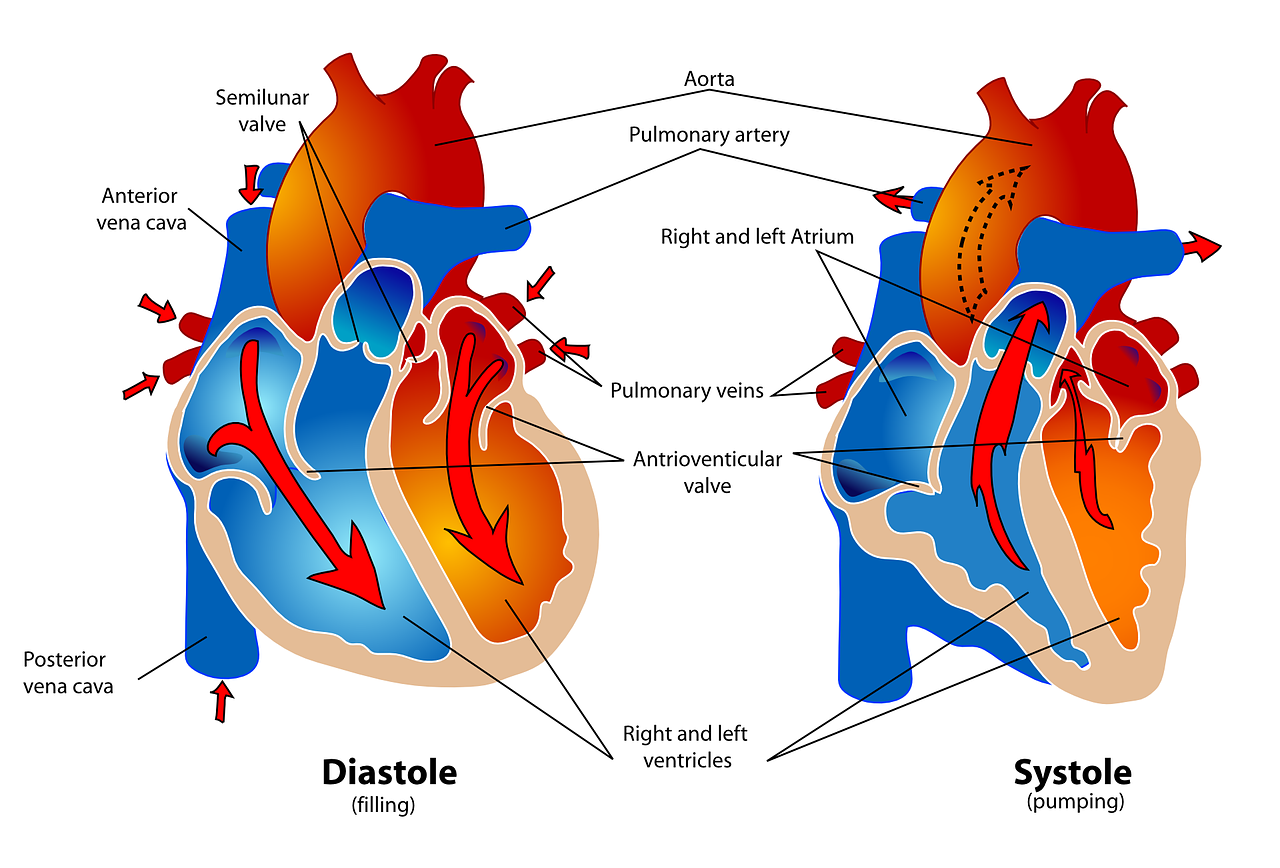
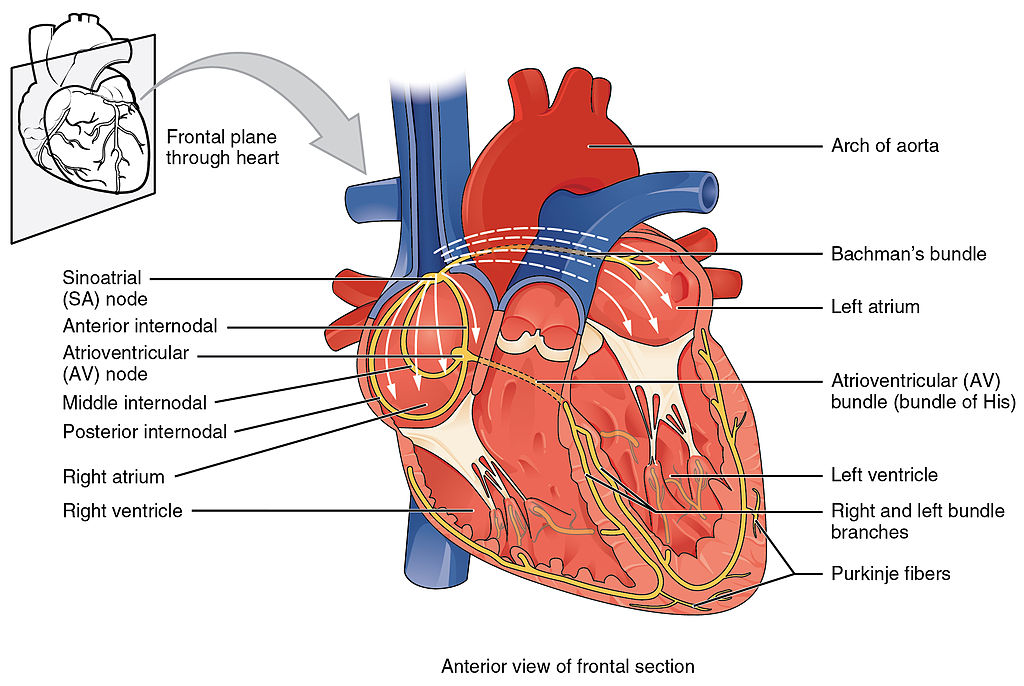
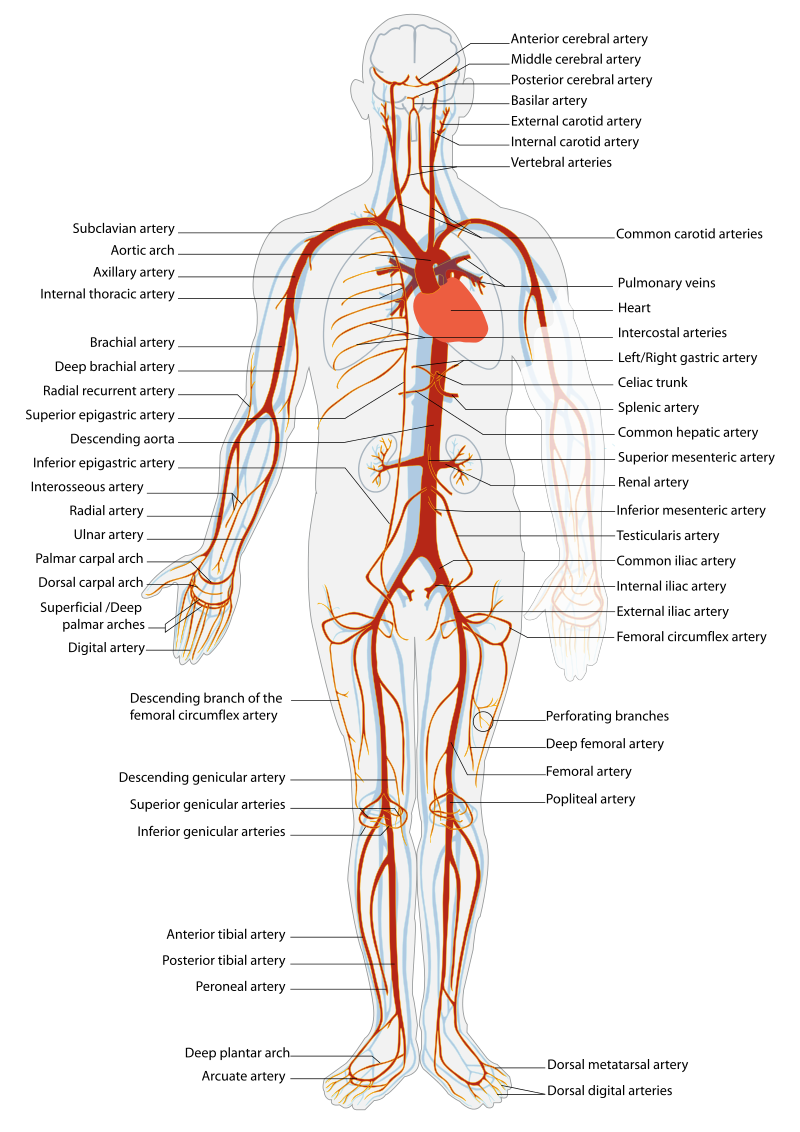
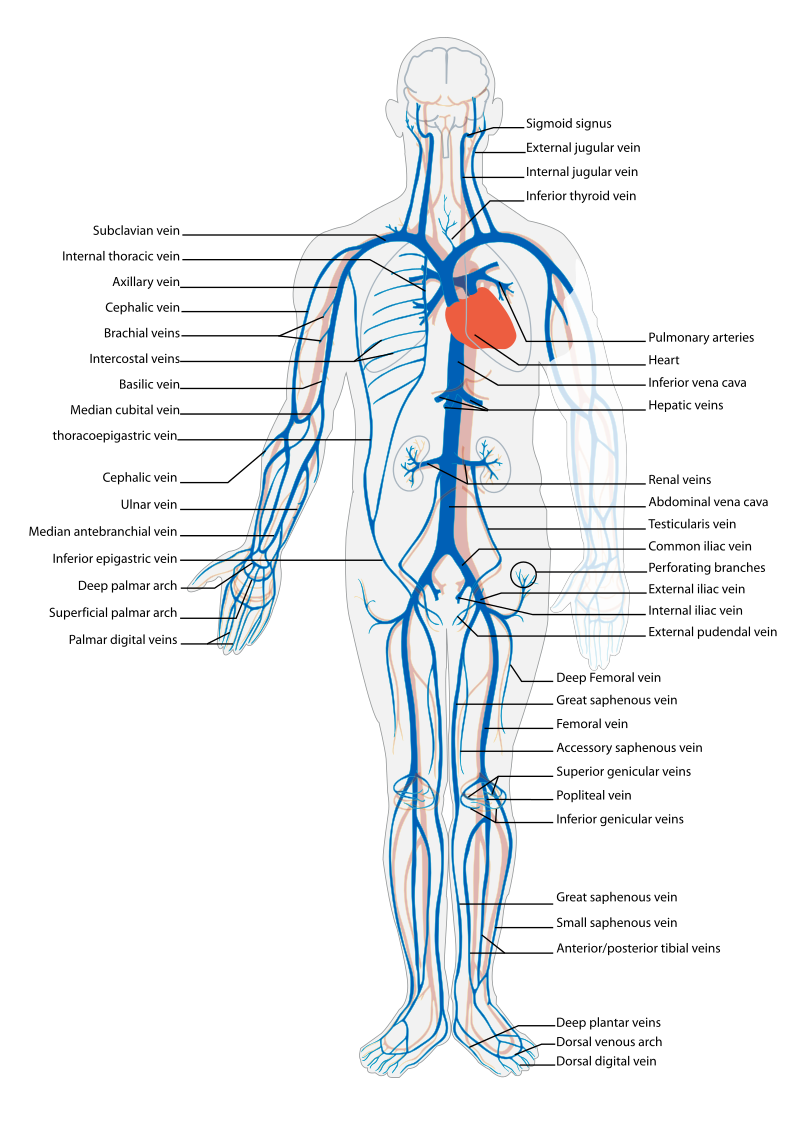
Before assessing a patient’s cardiovascular system, it is important to understand the various functions of the cardiovascular system. In addition to the information provided in the “Review of Cardiac Basics” section, the following images provide an overview of the cardiovascular system. Figure 9.1[1] provides an overview of the structure of the heart. Note the main cardiac structures are the atria, ventricles, and heart valves. Figure 9.2[2] demonstrates blood flow through the heart. Notice the flow of deoxygenated blood from the posterior and superior vena cava into the right atria and ventricle during diastole (indicated by blue coloring of these structures). The right ventricle then pumps deoxygenated blood to the lungs via the pulmonary artery during systole. At the same time, oxygenated blood from the lungs returns to the left atria and ventricle via the pulmonary veins during diastole (indicated by red coloring of these structures) and then is pumped out to the body via the aorta during systole. Figure 9.3[3] demonstrates the conduction system of the heart. This image depicts the conduction pathway through the heart as the tissue responds to electrical stimulation. Figure 9.4[4] illustrates the arteries of the circulatory system, and Figure 9.5[5] depicts the veins of the circulatory system. The purpose of these figures is to facilitate understanding of the electrical and mechanical function of the heart within the cardiovascular system.
Assessing the cardiovascular system includes performing several subjective and objective assessments. At times, assessment findings are modified according to life span considerations.
Subjective Assessment
The subjective assessment of the cardiovascular and peripheral vascular system is vital for uncovering signs of potential dysfunction. To complete the subjective cardiovascular assessment, the nurse begins with a focused interview. The focused interview explores past medical and family history, medications, cardiac risk factors, and reported symptoms. Symptoms related to the cardiovascular system include chest pain, peripheral edema, unexplained sudden weight gain, shortness of breath (dyspnea), irregular pulse rate or rhythm, dizziness, or poor peripheral circulation. Any new or worsening symptoms should be documented and reported to the health care provider.
Table 9.3a outlines questions used to assess symptoms related to the cardiovascular and peripheral vascular systems. Table 9.3b outlines questions used to assess medical history, medications, and risk factors related to the cardiovascular system. Information obtained from the interview process is used to tailor future patient education by the nurse.[6],[7],[8]
Table 9.3a Interview Questions for Cardiovascular and Peripheral Vascular Systems[9]
| Symptom | Question |
Follow-Up Safety Note: If findings indicate current severe symptoms suggestive of myocardial infarction or another critical condition, suspend the remaining cardiovascular assessment and obtain immediate assistance according to agency policy or call 911. |
|---|---|---|
| Chest Pain | Have you had any pain or pressure in your chest, neck, or arm? | Review how to assess a patient’s chief complaint using the PQRSTU method in the “Health History” chapter.
|
| Shortness of Breath
(Dyspnea) |
Do you ever feel short of breath with activity?
Do you ever feel short of breath at rest? Do you feel short of breath when lying flat? |
What level of activity elicits shortness of breath?
How long does it take you to recover? Have you ever woken up from sleeping feeling suddenly short of breath How many pillows do you need to sleep, or do you sleep in a chair (orthopnea)? Has this recently changed? |
| Edema | Have you noticed swelling of your feet or ankles?
Have you noticed your rings, shoes, or clothing feel tight at the end of the day? Have you noticed any unexplained, sudden weight gain? Have you noticed any new abdominal fullness? |
Has this feeling of swelling or restriction gotten worse?
Is there anything that makes the swelling better (e.g., sitting with your feet elevated)? How much weight have you gained? Over what time period have you gained this weight? |
| Palpitations | Have you ever noticed your heart feels as if it is racing or “fluttering” in your chest?
Have you ever felt as if your heart “skips” a beat? |
Are you currently experiencing palpitations?
When did palpitations start? Have you previously been treated for palpitations? If so, what treatment did you receive? |
| Dizziness (Syncope) |
Do you ever feel light-headed?
Do you ever feel dizzy? Have you ever fainted? |
Can you describe what happened?
Did you have any warning signs? Did this occur with position change? |
| Poor Peripheral Circulation | Do your hands or feet ever feel cold or look pale or bluish?
Do you have pain in your feet or lower legs when exercising? |
What, if anything, brings on these symptoms?
How much activity is needed to cause this pain? Is there anything, such as rest, that makes the pain better? |
| Calf Pain | Do you currently have any constant pain in your lower legs? | Can you point to the area of pain with one finger? |
Table 9.3b Interview Questions Exploring Cardiovascular Medical History, Medications, and Cardiac Risk Factors
| Topic | Questions |
|---|---|
| Medical History | Have you ever been diagnosed with any heart or circulation conditions, such as high blood pressure, coronary artery disease, peripheral vascular disease, high cholesterol, heart failure, or valve problems?
Have you had any procedures done to improve your heart function, such as ablation or stent placement? Have you ever had a heart attack or stroke? |
| Medications | Do you take any heart-related medications, herbs, or supplements to treat blood pressure, chest pain, high cholesterol, cardiac rhythm, fluid retention, or the prevention of clots? |
| Cardiac Risk Factors | Have your parents or siblings been diagnosed with any heart conditions?
Do you smoke or vape?
If you do not currently smoke, have you smoked in the past?
Are you physically active during the week?
What does a typical day look like in your diet?
Do you drink alcoholic drinks?
Would you say you experience stress in your life?
How many hours of sleep do you normally get each day?
|
Objective Assessment
The physical examination of the cardiovascular system involves the interpretation of vital signs, inspection, palpation, and auscultation of heart sounds as the nurse evaluates for sufficient perfusion and cardiac output.
For more information about assessing a patient’s oxygenation status as it relates to their cardiac output, visit the “Oxygenation” chapter in Open RN Nursing Fundamentals.
Equipment needed for a cardiovascular assessment includes a stethoscope, penlight, centimeter ruler or tape measure, and sphygmomanometer.[10]
Evaluate Vital Signs and Level of Consciousness
Interpret the blood pressure and pulse readings to verify the patient is stable before proceeding with the physical exam. Assess the level of consciousness; the patient should be alert and cooperative.
Inspection
- Skin color to assess perfusion. Inspect the face, lips, and fingertips for cyanosis or pallor. Cyanosis is a bluish discoloration of the skin, lips, and nail beds and indicates decreased perfusion and oxygenation. Pallor is the loss of color, or paleness of the skin or mucous membranes, as a result of reduced blood flow, oxygenation, or decreased number of red blood cells. Patients with light skin tones should be pink in color. For those with darker skin tones, assess for pallor on the palms, conjunctiva, or inner aspect of the lower lip.
- Jugular Vein Distension (JVD). Inspect the neck for JVD that occurs when the increased pressure of the superior vena cava causes the jugular vein to bulge, making it most visible on the right side of a person’s neck. JVD should not be present in the upright position or when the head of bed is at 30-45 degrees.
- Precordium for abnormalities. Inspect the chest area over the heart (also called precordium) for deformities, scars, or any abnormal pulsations the underlying cardiac chambers and great vessels may produce.
- Extremities:
- Upper Extremities: Inspect the fingers, arms, and hands bilaterally noting Color, Warmth, Movement, Sensation (CWMS). Alterations or bilateral inconsistency in CWMS may indicate underlying conditions or injury. Assess capillary refill by compressing the nail bed until it blanches and record the time taken for the color to return to the nail bed. Normal capillary refill is less than 3 seconds.[11]
- Lower Extremities: Inspect the toes, feet, and legs bilaterally, noting CWMS, capillary refill, and the presence of peripheral edema, superficial distended veins, and hair distribution. Document the location and size of any skin ulcers.
- Edema: Note any presence of edema. Peripheral edema is swelling that can be caused by infection, thrombosis, or venous insufficiency due to an accumulation of fluid in the tissues. (See Figure 9.6[12] for an image of pedal edema.)[13]
- Deep Vein Thrombosis (DVT): A deep vein thrombosis (DVT) is a blood clot that forms in a vein deep in the body. DVT requires emergency notification of the health care provider and immediate follow-up because of the risk of developing a life-threatening pulmonary embolism.[14] Inspect the lower extremities bilaterally. Assess for size, color, temperature, and for presence of pain in the calves. Unilateral warmth, redness, tenderness, swelling in the calf, or sudden onset of intense, sharp muscle pain that increases with dorsiflexion of the foot is an indication of a deep vein thrombosis (DVT).[15] See Figure 9.7[16] for an image of a DVT in the patient’s right leg, indicated by unilateral redness and edema.


Auscultation
Heart Sounds
Auscultation is routinely performed over five specific areas of the heart to listen for corresponding valvular sounds. These auscultation sites are often referred to by the mnemonic “APE To Man,” referring to Aortic, Pulmonic, Erb’s point, Tricuspid, and Mitral areas (see Figure 9.8[17] for an illustration of cardiac auscultation areas). The aortic area is the second intercostal space to the right of the sternum. The pulmonic area is the second intercostal space to the left of the sternum. Erb’s point is directly below the pulmonic area and located at the third intercostal space to the left of the sternum. The tricuspid (or parasternal) area is at the fourth intercostal space to the left of the sternum. The mitral (also called apical or left ventricular area) is the fifth intercostal space at the midclavicular line.
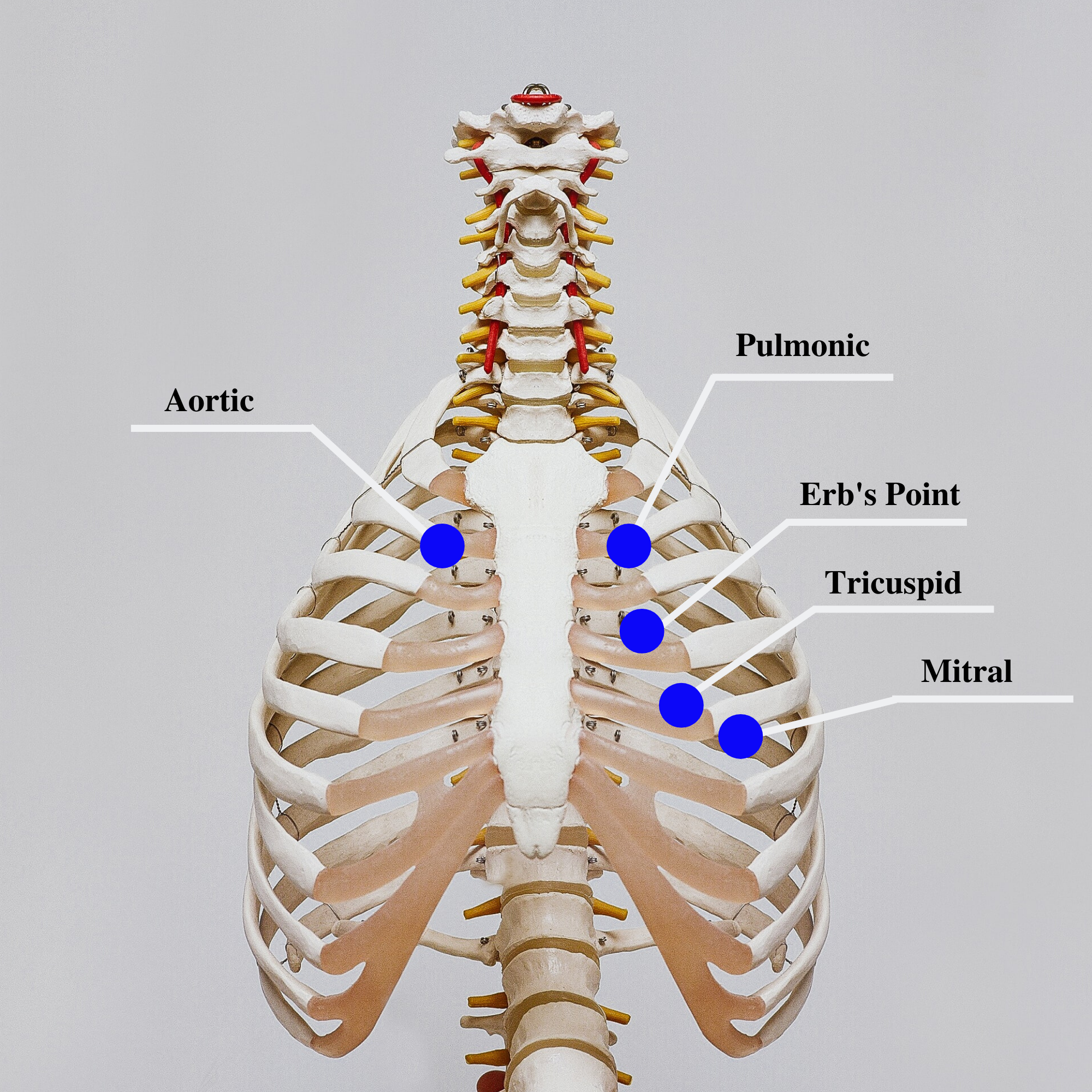
Auscultation usually begins at the aortic area (upper right sternal edge). Use the diaphragm of the stethoscope to carefully identify the S1 and S2 sounds. They will make a “lub-dub” sound. Note that when listening over the area of the aortic and pulmonic valves, the “dub” (S2) will sound louder than the “lub” (S1). Move the stethoscope sequentially to the pulmonic area (upper left sternal edge), Erb’s point (left third intercostal space at the sternal border), and tricuspid area (fourth intercostal space. When assessing the mitral area for female patients, it is often helpful to ask them to lift up their breast tissue so the stethoscope can be placed directly on the chest wall. Repeat this process with the bell of the stethoscope. The apical pulse should be counted over a 60-second period. For an adult, the heart rate should be between 60 and 100 with a regular rhythm to be considered within normal range. The apical pulse is an important assessment to obtain before the administration of many cardiac medications.
The first heart sound (S1) identifies the onset of systole, when the atrioventricular (AV) valves (mitral and tricuspid) close and the ventricles contract and eject the blood out of the heart. The second heart sound (S2) identifies the end of systole and the onset of diastole when the semilunar valves close, the AV valves open, and the ventricles fill with blood. S1 corresponds to the palpable pulse. When auscultating, it is important to identify the S1 (“lub”) and S2 (“dub”) sounds, evaluate the rate and rhythm of the heart, and listen for any extra heart sounds.
![]() Auscultating Heart Sounds
Auscultating Heart Sounds
- To effectively auscultate heart sounds, patient repositioning may be required. If it difficult to hear the heart sounds, ask the patient to lean forward if they are able, or lie on their left side. These positions move the heart closer to their chest wall and can increase the volume of the heart sounds heard on auscultation. This repositioning may be helpful in patients with increased adipose tissue in their chest wall or larger breasts.
- It is common to hear lung sounds when auscultating the heart sounds. It may be helpful to ask the patient to briefly hold their breath if lung sounds impede adequate heart auscultation. Limit the holding of breath to 10 seconds or as tolerated by the patient.
- Environmental noise can cause difficulty in auscultating heart sounds. Removing environmental noise by turning down the television volume or shutting the door may be required for an accurate assessment.
- Patients may try to talk to you as you are assessing their heart sounds. It is often helpful to explain the procedure such as, “I am going to take a few minutes to listen carefully to the sounds of blood flow going through your heart. Please try not to speak while I am listening, so I can hear the sounds better.”
Extra Heart Sounds
Extra heart sounds include clicks, murmurs, S3 and S4 sounds, and pleural friction rubs. These extra sounds can be difficult for a novice to distinguish, so if you notice any new or different sounds, consult an advanced practitioner or notify the provider. A midsystolic click, associated with mitral valve prolapse, may be heard with the diaphragm at the apex or left lower sternal border.
A click may be followed by a murmur. A murmur is a blowing or whooshing sound that signifies turbulent blood flow often caused by a valvular defect. New murmurs not previously recorded should be immediately communicated to the health care provider. In the aortic area, listen for possible murmurs of aortic stenosis and aortic regurgitation with the diaphragm of the stethoscope. In the pulmonic area, listen for potential murmurs of pulmonic stenosis and pulmonary and aortic regurgitation. In the tricuspid area, at the fourth and fifth intercostal spaces along the left sternal border, listen for the potential murmurs of tricuspid regurgitation, tricuspid stenosis, or ventricular septal defect.
S3 and S4 sounds, if present, are often heard best by asking the patient to lie on their left side and listening over the apex with the bell of the stethoscope. An S3 sound, also called a ventricular gallop, occurs after the S2 and sounds like “lub-dub-dah,” or a sound similar to a horse galloping. An S3 can occur when a patient is experiencing fluid overload, such as during an acute exacerbation of heart failure.[18] It can also be a normal finding in pregnancy due to increased blood flow through the ventricles.
The S4 sound, also called atrial gallop, occurs immediately before the S1 and sounds like “ta-lub-dub.” An S4 sound can occur with decreased ventricular compliance or coronary artery disease.[19]
A pericardial friction rub is caused by inflammation of the pericardium, with a creaky-scratchy noise generated as the parietal and visceral membranes rub together. It is best heard at the apex or left lower sternal border with the diaphragm as the patient sits up, leans forward, and holds their breath.
Carotid Sounds
The carotid artery may be auscultated for bruits. Bruits are a swishing sound due to turbulence in the blood vessel and may be heard due to atherosclerotic changes.
Palpation
Palpation is used to evaluate peripheral pulses, capillary refill, and for the presence of edema. When palpating these areas, also pay attention to the temperature and moisture of the skin.
Pulses
Compare the rate, rhythm, and quality of arterial pulses bilaterally, including the carotid, radial, brachial, posterior tibialis, and dorsalis pedis pulses. Review additional information about obtaining pulses in the “General Survey” chapter. Bilateral comparison for all pulses (except the carotid) is important for determining subtle variations in pulse strength. Carotid pulses should be palpated on one side at a time to avoid decreasing perfusion of the brain. The posterior tibial artery is located just behind the medial malleolus. It can be palpated by scooping the patient’s heel in your hand and wrapping your fingers around so that the tips come to rest on the appropriate area just below the medial malleolus. The dorsalis pedis artery is located just lateral to the extensor tendon of the big toe and can be identified by asking the patient to flex their toe while you provide resistance to this movement. Gently place the tips of your second, third, and fourth fingers adjacent to the tendon, and try to feel the pulse.
The quality of the pulse is graded on a scale of 0 to 3, with 0 being absent pulses, 1 being decreased pulses, 2 is within normal range, and 3 being increased (also referred to as “bounding”). If unable to palpate a pulse, additional assessment is needed. First, determine if this is a new or chronic finding. Second, if available, use a Doppler ultrasound to determine the presence or absence of the pulse. Many agencies use Doppler ultrasound to document if a nonpalpable pulse is present. If the pulse is not found, this could be a sign of an emergent condition requiring immediate follow-up and provider notification. See Figures 9.9[20] and 9.10[21] for images of assessing pedal pulses.


Capillary Refill
The capillary refill test is performed on the nail beds to monitor perfusion, the amount of blood flow to tissue. Pressure is applied to a fingernail or toenail until it pales, indicating that the blood has been forced from the tissue under the nail. This paleness is called blanching. Once the tissue has blanched, pressure is removed. Capillary refill time is defined as the time it takes for the color to return after pressure is removed. If there is sufficient blood flow to the area, a pink color should return within 2 seconds after the pressure is removed.[22]
Review of Capillary Refill Test on YouTube[23].
Edema
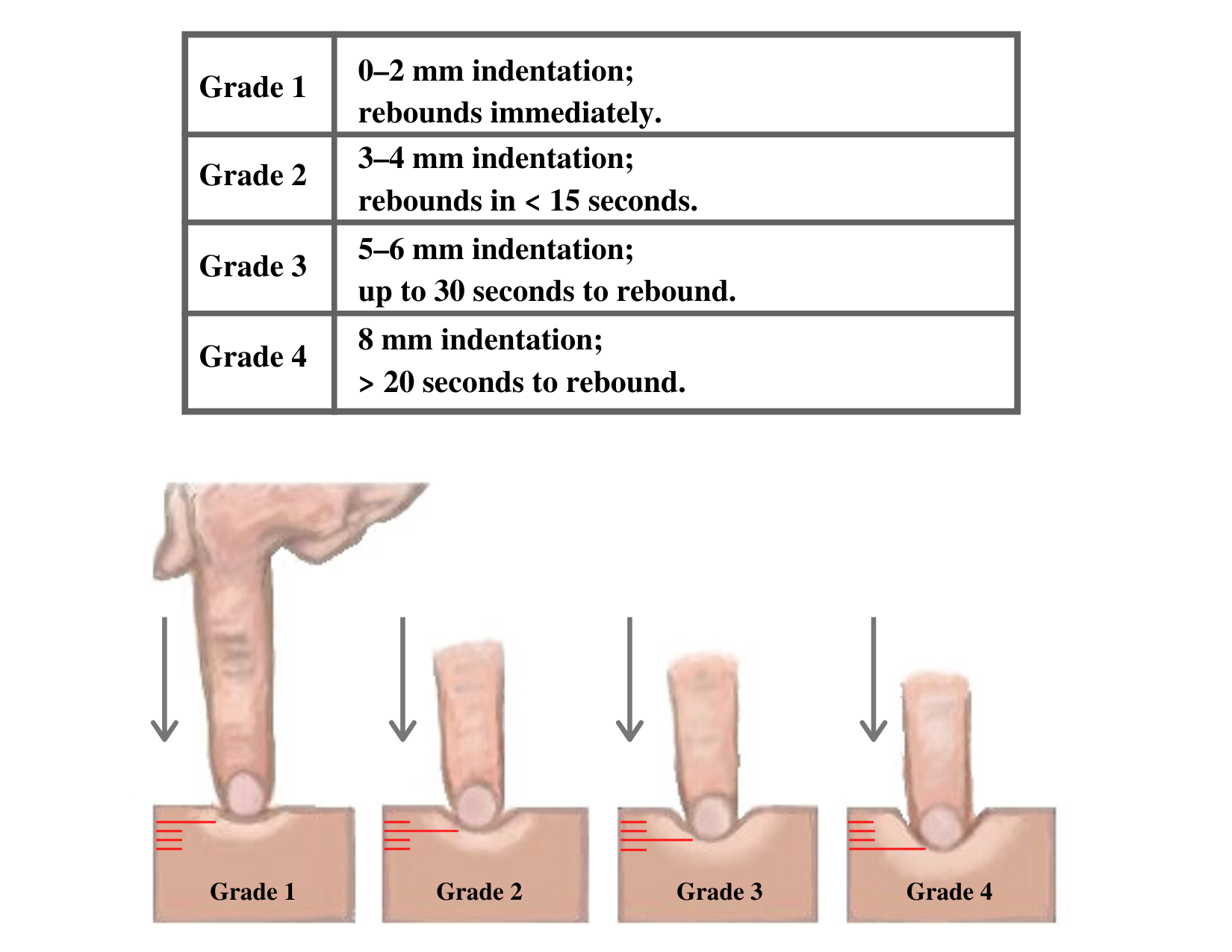
Edema occurs when one can visualize visible swelling caused by a buildup of fluid within the tissues. If edema is present on inspection, palpate the area to determine if the edema is pitting or nonpitting. Press on the skin to assess for indentation, ideally over a bony structure, such as the tibia. If no indentation occurs, it is referred to as nonpitting edema. If indentation occurs, it is referred to as pitting edema. See Figure 9.11[24] for images demonstrating pitting edema.

Note the depth of the indention and how long it takes for the skin to rebound back to its original position. The indentation and time required to rebound to the original position are graded on a scale from 1 to 4. Edema rated at 1+ indicates a barely detectable depression with immediate rebound, and 4+ indicates a deep depression with a time lapse of over 20 seconds required to rebound. See Figure 9.12[25] for an illustration of grading edema. Additionally, it is helpful to note edema may be difficult to observe in larger patients. It is also important to monitor for sudden changes in weight, which is considered a probable sign of fluid volume overload.
Heaves or Thrills
You may observe advanced practice nurses and other health care providers palpating the anterior chest wall to detect any abnormal pulsations the underlying cardiac chambers and great vessels may produce. Precordial movements should be evaluated at the apex (mitral area). It is best to examine the precordium with the patient supine because if the patient is turned on the left side, the apical region of the heart is displaced against the lateral chest wall, distorting the chest movements.[26] A heave or lift is a palpable lifting sensation under the sternum and anterior chest wall to the left of the sternum that suggests severe right ventricular hypertrophy. A thrill is a vibration felt on the skin of the precordium or over an area of turbulence, such as an arteriovenous fistula or graft.
Life Span Considerations
The cardiovascular assessment and expected findings should be modified according to common variations across the life span.
Infants and Children
A murmur may be heard in a newborn in the first few days of life until the ductus arteriosus closes.
When assessing the cardiovascular system in children, it is important to assess the apical pulse. Parameters for expected findings vary according to age group. After a child reaches adolescence, a radial pulse may be assessed. Table 9.3c outlines the expected apical pulse rate by age.
Table 9.3c Expected Apical Pulse by Age
| Age Group | Heart Rate |
|---|---|
| Preterm | 120-180 |
| Newborn (0 to 1 month) | 100-160 |
| Infant (1 to 12 months) | 80-140 |
| Toddler (1 to 3 years) | 80-130 |
| Preschool (3 to 5 years) | 80-110 |
| School Age (6 to 12 years) | 70-100 |
| Adolescents (13 to 18 years) | 60-90 |
Older Adults
In adults over age 65, irregular heart rhythms and extra sounds are more likely. An “irregularly irregular” rhythm suggests atrial fibrillation, and further investigation is required if this is a new finding. See the box below for more information about atrial fibrillation.
For more information on atrial fibrillation, visit the CDC Atrial Fibrillation webpage.
Expected Versus Unexpected Findings
After completing a cardiovascular assessment, it is important for the nurse to use critical thinking to determine if any findings require follow-up. Depending on the urgency of the findings, follow-up can range from calling the health care provider to calling the rapid response team. Table 9.3d compares examples of expected findings, meaning those considered within normal limits, to unexpected findings, which require follow-up. Critical conditions are those that should be reported immediately and may require notification of a rapid response team.
Table 9.3d Expected Versus Unexpected Findings on Cardiac Assessment
| Assessment | Expected Findings | Unexpected Findings (Document and notify the provider if this is a new finding*) |
|---|---|---|
| Inspection | Apical impulse may or may not be visible | Scars not previously documented that could indicate prior cardiac surgeries
Heave or lift observed in the precordium Chest anatomy malformations |
| Palpation | Apical pulse felt over midclavicular fifth intercostal space | Apical pulse felt to the left of the midclavicular fifth intercostal space
Additional movements over precordium such as a heave, lift, or thrill |
| Auscultation | S1 and S2 heart sounds in a regular rhythm | New irregular heart rhythm
Extra heart sounds such as a murmur, S3, or S4 |
| *CRITICAL CONDITIONS to report immediately | Symptomatic tachycardia at rest (HR>100 bpm)
Symptomatic bradycardia (HR<60 bpm) New systolic blood pressure (<100 mmHg) Orthostatic blood pressure changes (see “Blood Pressure” chapter for more information) New irregular heart rhythm New extra heart sounds such as a murmur, S3, or S4 New abnormal cardiac rhythm changes Reported chest pain, calf pain, or worsening shortness of breath |
See Table 9.3e for a comparison of expected versus unexpected findings when assessing the peripheral vascular system.
Table 9.3e Expected Versus Unexpected Peripheral Vascular Assessment Findings
| Assessment | Expected Findings | Unexpected Findings (Document or notify provider if new finding*) |
|---|---|---|
| Inspection | Skin color uniform and appropriate for race bilaterally
Equal hair distribution on upper and lower extremities Absence of jugular vein distention (JVD) Absence of edema Sensation and movement of fingers and toes intact |
Cyanosis or pallor, indicating decreased perfusion
Decreased or unequal hair distribution Presence of jugular vein distention (JVD) in an upright position or when head of bed is 30-45 degrees New or worsening edema Rapid and unexplained weight gain Impaired movement or sensation of fingers and toes |
| Palpation | Skin warm and dry
Pulses present and equal bilaterally Absence of edema Capillary refill less than 2 seconds |
Skin cool, excessively warm, or diaphoretic
Absent, weak/thready, or bounding pulses New irregular pulse New or worsening edema Capillary refill greater than 2 seconds Unilateral warmth, redness, tenderness, or edema, indicating possible deep vein thrombosis (DVT) |
| Auscultation | Carotid pulse | Carotid bruit |
| *CRITICAL CONDITIONS to report immediately | Cyanosis
Absent pulse (and not heard using Doppler device) Capillary refill time greater than 3 seconds Unilateral redness, warmth, and edema, indicating a possible deep vein thrombosis (DVT) |
“Sternum_composition.png” by Anatomography is licensed under CC BY-SA 2.1 Japan
“Sternum_composition.png” by Anatomography is licensed under CC BY-SA 2.1 Japan
- "Diagram of the human heart” by Wapcaplet is licensed under CC BY-SA 3.0 ↵
- "Diagram of the human heart” by Wapcaplet is licensed under CC BY-SA 3.0 ↵
- “2018 Conduction System of Heart.jpg” by OpenStax is licensed under CC-BY-3.0 ↵
- “Arterial System en.svg” by LadyofHats, Mariana Ruiz Villarreal is in the Public Domain. ↵
- “Venous system en.svg” by Lady of Hats Mariana Ruiz Vilarreal is in the Public Domain. ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology licensed under CC BY 4.0 ↵
- Felner, J. M. (1990). An overview of the cardiovascular system. In Walker, H. K., Hall, W. D., & Hurst, J. W. (Eds.), Clinical methods: The history, physical, and laboratory examinations (3rd ed., Chapter 7). Butterworths. https://www.ncbi.nlm.nih.gov/books/NBK393/ ↵
- Scott, C., & MacInnes, J. D. (2013, September 27). Cardiac patient assessment: putting the patient first. British Journal of Nursing, 15(9). https://doi.org/10.12968/bjon.2006.15.9.21091 ↵
- Scott, C., & MacInnes, J. D. (2013, September 27). Cardiac patient assessment: putting the patient first. British Journal of Nursing, 15(9). https://doi.org/10.12968/bjon.2006.15.9.21091 ↵
- Felner, J. M. (1990). An overview of the cardiovascular system. In Walker, H. K., Hall, W. D., & Hurst, J. W. (Eds.), Clinical methods: The history, physical, and laboratory examinations (3rd ed., Chapter 7). Butterworths. https://www.ncbi.nlm.nih.gov/books/NBK393/ ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology licensed under CC BY 4.0 ↵
- “Swollen feet at Harefield Hospital edema.jpg” by Ryaninuk is licensed under CC BY-SA 4.0 ↵
- Simon, E. C. (2014). Leg edema assessment and management. MEDSURG Nursing, 23(1), 44-53. ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology licensed under CC BY 4.0 ↵
- This work is a derivative of Clinical Procedures for Safer Patient Care by British Columbia Institute of Technology licensed under CC BY 4.0 ↵
- “Deep vein thrombosis of the right leg.jpg” by James Heilman, MD is licensed under CC BY-SA 3.0 ↵
- “Cardiac Auscultation Areas” by Meredith Pomietlo for Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- Shono, A., Mori, S., Yatomi, A., Kamio, T., Sakai, J., Soga, F., Tanaka, H., & Hirata, K. I. (2019). Ultimate third heart sound. Internal Medicine, 58(17), 2535–2538. https://doi.org/10.2169/internalmedicine.2731-19 ↵
- Felner, J. M. (1990). An overview of the cardiovascular system. In Walker, H. K., Hall, W. D., & Hurst, J. W. (Eds.), Clinical methods: The history, physical, and laboratory examinations (3rd ed., Chapter 7). Butterworths. https://www.ncbi.nlm.nih.gov/books/NBK393/ ↵
- “DSC_2277.jpg” by British Columbia Institute of Technology is licensed under CC BY 4.0. Access for free at https://opentextbc.ca/clinicalskills/chapter/2-5-focussed-respiratory-assessment/ ↵
- “DSC_2314.jpg” by British Columbia Institute of Technology is licensed under CC BY 4.0. Access for free at https://opentextbc.ca/clinicalskills/chapter/2-5-focussed-respiratory-assessment/ ↵
- A.D.A.M. Medical Encyclopedia [Internet]. Atlanta (GA): A.D.A.M., Inc.; c1997-2020. Capillary nail refill test; [updated 2020, Aug 9] https://medlineplus.gov/ency/article/003394.htm ↵
- RegisteredNurseRN. (2022, March 21). Capillary Refill Time Test: Normal vs. Abnormal - Nursing Clincial Skills. [Video]. YouTube. Used with permission. All rights reserved. https://youtu.be/EwaDSZRH1LE ↵
- “Combinpedal.jpg” by James Heilman, MD is licensed under CC BY-SA 3.0 ↵
- “Grading of Edema” by Meredith Pomietlo for Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- Felner, J. M. (1990). An overview of the cardiovascular system. In Walker, H. K., Hall, W. D., & Hurst, J. W. (Eds.), Clinical methods: The history, physical, and laboratory examinations (3rd ed., Chapter 7). Butterworths. https://www.ncbi.nlm.nih.gov/books/NBK393/ ↵
Assessment is the first step of the nursing process (and the first Standard of Practice by the American Nurses Association). This standard is defined as, "The registered nurse collects pertinent data and information relative to the health care consumer's health or the situation." This includes collecting “pertinent data related to the health and quality of life in a systematic, ongoing manner, with compassion and respect for the wholeness, inherent dignity, worth, and unique attributes of every person, including, but not limited to, demographics, environmental and occupational exposures, social determinants of health, health disparities, physical, functional, psychosocial, emotional, cognitive, spiritual/transpersonal, sexual, sociocultural, age-related, environmental, and lifestyle/economic assessments.”[1] See Figure 4.5a for an illustration of how the Assessment phase of the nursing process corresponds to the NCSBN Clinical Judgment Measurement Model (NCJMM).[2]
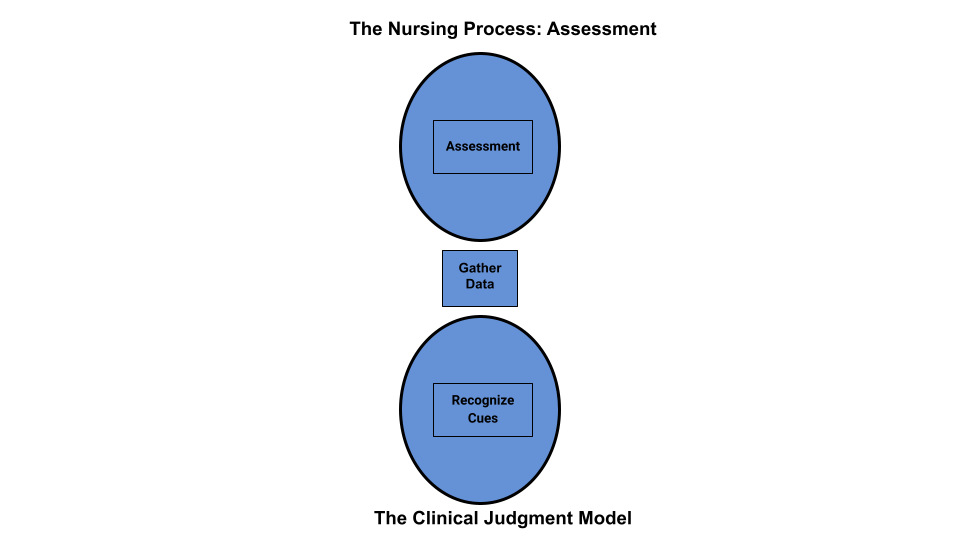
Figure 4.5a Comparison of the Assessment Phase of the Nursing Process to the NCJMM
Nurses assess clients to gather information, then use critical thinking to analyze the data and recognized cues. Data is considered subjective or objective and can be collected from multiple sources.
Subjective Assessment Data
Subjective data is information obtained from the client and/or family members and offers important cues from their perspectives. When documenting subjective data stated by a client, it should be in quotation marks and start with verbiage such as, "The client reports..." It is vital for the nurse to establish rapport with a client to obtain accurate, valuable subjective data regarding the mental, emotional, and spiritual aspects of their condition.
There are two types of subjective information, primary and secondary. Primary data is information provided directly by the client. Clients are the best source of information about their bodies and feelings, and the nurse who actively listens to a client will often learn valuable information while also promoting a sense of well-being. Information collected from a family member, chart, or other sources is known as secondary data. Family members can provide important information, especially for individuals with memory impairments, infants, children, or when clients are unable to speak for themselves.
See Figure 4.5b[3] for an illustration of a nurse obtaining subjective data and establishing rapport after obtaining permission from the client to sit on the bed.
Example of Subjective Data
An example of how to document subjective data obtained during a client assessment is, "The client reports, 'My pain is a level 2 on a 1-10 scale.'”

Objective Assessment Data
Objective data is anything that you can observe through your sense of hearing, sight, smell, and touch while assessing the client. Objective data is reproducible, meaning another person can easily obtain the same data. Examples of objective data are vital signs, physical examination findings, and laboratory results. See Figure 4.6[4] for an image of a nurse performing a physical examination.
Example of Objective Data
An example of documented objective data obtained during a client assessment is, "The client’s radial pulse is 58 and regular, and their skin feels warm and dry."

Sources of Assessment Data
There are three sources of assessment data: interview, physical examination, and review of laboratory or diagnostic test results.
Interviewing
Interviewing includes asking the client and their family members questions, listening, and observing verbal and nonverbal communication. Reviewing the chart prior to interviewing the client may eliminate redundancy in the interview process and allows the nurse to hone in on the most significant areas of concern or need for clarification. However, if information in the chart does not make sense or is incomplete, the nurse should use the interview process to verify data with the client.
After performing client identification, the best way to initiate a caring relationship is to introduce yourself to the client and explain your role. Share the purpose of your interview and the approximate time it will take. When beginning an interview, it may be helpful to start with questions related to the client’s medical diagnoses. Medical diagnoses are diseases, disorders, or injuries diagnosed by a physician or advanced health care provider, such as a nurse practitioner or physician's assistant. Reviewing the medical diagnoses allows the nurse to gather information about how they have affected the client's functioning, relationships, and lifestyle. Listen carefully and ask for clarification when something isn’t clear to you. Clients may not volunteer important information because they don’t realize it is important for their care. By using critical thinking and active listening, you may discover valuable cues that are important to provide safe, quality nursing care. Sometimes nursing students can feel uncomfortable having difficult conversations or asking personal questions due to generational or other cultural differences. Don’t shy away from asking about information that is important to know for safe client care. Most clients will be grateful that you cared enough to ask and listen.
Be alert and attentive to how the client answers questions, as well as when they do not answer a question. Nonverbal communication and body language can be cues to important information that requires further investigation. A keen sense of observation is important. To avoid making inappropriate inferences, the nurse should validate cues for accuracy. For example, a nurse may make an inference that a client appears depressed when the client avoids making eye contact during an interview. However, upon further questioning, the nurse may discover that the client’s cultural background believes direct eye contact to be disrespectful and this is why they are avoiding eye contact. To read more information about communicating with clients, review the “Communication” chapter of this book.
Physical Examination
A physical examination is a systematic data collection method of the body that uses the techniques of inspection, auscultation, palpation, and percussion. Inspection is the observation of a client’s anatomical structures. Auscultation is listening to sounds, such as heart, lung, and bowel sounds, created by organs using a stethoscope. Palpation is the use of touch to evaluate organs for size, location, or tenderness. Percussion is an advanced physical examination technique typically performed by providers where body parts are tapped with fingers to determine their size and if fluid or air are present. Detailed physical examination procedures of various body systems can be found in the Open RN Nursing Skills, 2e textbook with a head-to-toe checklist in Appendix C. Physical examination also includes the collection and analysis of vital signs.
Registered nurses (RNs) complete the initial physical examination and analyze the findings as part of the nursing process. Collection of follow-up physical examination data can be delegated to licensed practical nurses/licensed vocational nurses (LPNs/LVNs), or measurements such as vital signs and weight may be delegated to trained unlicensed assistive personnel (UAP) when appropriate to do so. However, the RN remains responsible for supervising these tasks, analyzing the findings, and ensuring they are documented.
A physical examination can be performed as a comprehensive head-to-toe assessment or as a focused assessment related to a particular condition or problem. Assessment data is documented in the client’s medical record, either in their electronic medical record (EMR) or their paper chart, depending upon agency policies and procedures.
Reviewing Laboratory and Diagnostic Test Results
Reviewing laboratory and diagnostic test results provides relevant and useful information related to the needs of the client. Understanding how normal and abnormal results affect client care is important when implementing the nursing care plan and administering provider prescriptions. If results cause concern, it is the nurse’s responsibility to notify the provider and verify the appropriateness of prescriptions based on the client’s current status before implementing them.
Types of Assessments
Several types of nursing assessment are used in clinical practice:
- Primary Survey: Used during every client encounter to briefly evaluate level of consciousness, airway, breathing, and circulation and implement emergency care if needed.
- Admission Assessment: A comprehensive assessment completed when a client is admitted to a facility that involves assessing a large amount of information using an organized approach.
- Ongoing Assessment: In acute care agencies such as hospitals, a head-to-toe assessment is completed and documented at least once every shift. Any changes in client condition are reported to the health care provider.
- Focused Assessment: Focused assessments are used to reevaluate the status of a previously diagnosed problem.
- Time-lapsed Reassessment: Time-lapsed reassessments are used in long-term care facilities when three or more months have elapsed since the previous assessment to evaluate progress on previously identified outcomes.[5]
Putting It Together
Review Scenario C in the following box to apply concepts of assessment to a client scenario.
Scenario C[6]

Ms. J. is a 74-year-old woman who is admitted directly to the medical unit after visiting her physician because of shortness of breath, increased swelling in her ankles and calves, and fatigue. Her medical history includes hypertension (30 years), coronary artery disease (18 years), heart failure (2 years), and type 2 diabetes (14 years). She takes 81 mg of aspirin every day, metoprolol 50 mg twice a day, furosemide 40 mg every day, and metformin 2,000 mg every day.
Ms. J.’s vital sign values on admission were as follows:
- Blood Pressure: 162/96 mm Hg
- Heart Rate: 88 beats/min
- Oxygen Saturation: 91% on room air
- Respiratory Rate: 28 breaths/minute
- Temperature: 97.8 degrees F orally
Her weight is up 10 pounds since the last office visit three weeks prior. The client states, “I am so short of breath” and “My ankles are so swollen I have to wear my house slippers.” Ms. J. also shares, “I am so tired and weak that I can’t get out of the house to shop for groceries,” and “Sometimes I’m afraid to get out of bed because I get so dizzy.” She confides, “I would like to learn more about my health so I can take better care of myself.”
The physical assessment findings of Ms. J. are bilateral basilar crackles in the lungs and bilateral 2+ pitting edema of the ankles and feet. Laboratory results indicate a decreased serum potassium level of 3.4 mEq/L.
As the nurse completes the physical assessment, the client’s daughter enters the room. She confides, “We are so worried about mom living at home by herself when she is so tired all the time!”
Critical Thinking Questions
- Identify relevant subjective data.
- Identify relevant objective data.
- Provide an example of secondary data.
Answers are located in the Answer Key at the end of the book.
This chapter introduces concepts related to nursing leadership and management, prioritization strategies, delegation and supervision, legal implications of nursing practice, ethical nursing practice, collaboration within the interprofessional team, health care economics, quality and evidence-based practice, advocacy, preparation for the RN role, and the avoidance of burnout with self-care.
This textbook discusses professional and management concepts related to the role of a registered nurse (RN) as defined by the American Nurses Association (ANA). The ANA publishes two resources that set standards and guide professional nursing practice in the United States: The Code of Ethics for Nurses With Interpretive Statements and Nursing: Scope and Standards of Practice. The Code of Ethics for Nurses With Interpretive Statements establishes an ethical framework for nursing practice across all roles, levels, and settings and is discussed in greater detail in the “Ethical Practice” chapter of this book. The Nursing: Scope and Standards of Practice resource defines the “who, what, where, when, why, and how of nursing” and sets the standards for practice that all registered nurses are expected to perform competently.[7]
The ANA defines the “who” of nursing practice as the nurses who have been educated, titled, and maintain active licensure to practice nursing. The “what” of nursing is the recently revised ANA definition of nursing: “Nursing integrates the art and science of caring and focuses on the protection, promotion, and optimization of health and human functioning; prevention of illness and injury; facilitation of healing; and alleviation of suffering through compassionate presence. Nursing is the diagnosis and treatment of human responses and advocacy in the care of individuals, families, groups, communities, and populations in recognition of the connection of all humanity.”[8] Simply put, nurses treat human responses to health problems and life processes and advocate for the care of others.
Nursing practice occurs “when'' there is a need for nursing knowledge, wisdom, caring, leadership, practice, or education, anytime, anywhere. Nursing practice occurs in any environment “where'' there is a health care consumer in need of care, information, or advocacy. The “why” of nursing practice is described as nursing’s response to the changing needs of society to achieve positive health care consumer outcomes in keeping with nursing’s social contract and obligation to society. The “how” of nursing practice is defined as the ways, means, methods, and manners that nurses use to practice professionally.[9] The “how” of nursing, also referred to as a nurse’s “scope and standards of practice,” is further defined by each state’s Nurse Practice Act; agency policies, procedures, and protocols; and federal regulations and ANA’s Standards of Practice.
State Boards of Nursing and Nurse Practice Acts
RNs must legally follow regulations set by the Nurse Practice Act by the state in which they are caring for patients with their nursing license. The Board of Nursing is the state-specific licensing and regulatory body that sets standards for safe nursing care and issues nursing licenses to qualified candidates based on the Nurse Practice Act. The Nurse Practice Act is enacted by that state’s legislature and defines the scope of nursing practice and establishes regulations for nursing practice within that state. If nurses do not follow the standards and scope of practice set forth by the Nurse Practice Act, they may be disciplined by the Board of Nursing in the form of reprimand, probation, suspension, or revocation of their nursing license. Investigations and discipline actions are reportable among states participating in the Nurse Licensure Compact (that allows nurses to practice across state lines) or when a nurse applies for licensure in a different state. The scope and standards of practice set forth in the Nurse Practice Act can also be used as evidence if a nurse is sued for malpractice.
Find your state's Nurse Practice Act on the National Council of State Board of Nursing (NCSBN) website.
Agency Policies, Procedures, and Protocols
In addition to practicing according to the Nurse Practice Act in the state they are employed, nurses must also practice according to agency policies, procedures, and protocols.
A policy is an expected course of action set by an agency. For example, hospitals set a policy requiring a thorough skin assessment to be completed when a patient is admitted and then reassessed and documented daily.
Agencies also establish their own set of procedures. A procedure is the method or defined steps for completing a task. For example, each agency has specific procedural steps for inserting a urinary catheter.
A protocol is a detailed, written plan for performing a regimen of therapy. For example, agencies typically establish a hypoglycemia protocol that nurses can independently and quickly implement when a patient’s blood sugar falls below a specific number without first calling a provider. A hypoglycemia protocol typically includes actions such as providing orange juice and rechecking the blood sugar and then reporting the incident to the provider.
Agency-specific policies, procedures, and protocols supersede the information taught in nursing school, and nurses can be held legally liable if they don’t follow them. It is vital for nurses to review and follow current agency-specific procedures, policies, and protocols while also practicing according to that state's nursing scope of practice. Malpractice cases have occurred when a nurse was asked by their employer to do something outside their legal scope of practice, impacting their nursing license. It is up to you to protect your nursing license and follow the Nurse Practice Act when providing patient care. If you have a concern about an agency’s policy, procedure, or protocol, follow the agency’s chain of command to report your concern.
Federal Regulations
Nursing practice is impacted by regulations enacted by federal agencies. Two examples of federal agencies setting standards of care are The Joint Commission and the Centers for Medicare and Medicaid Services.
The Joint Commission accredits and certifies over 20,000 health care organizations in the United States. The Joint Commission’s standards help health care organizations measure, assess, and improve performance on functions that are essential to providing safe, high-quality care. The standards are updated regularly to reflect the rapid advances in health care and address topics such as patient rights and education, infection control, medication management, and prevention of medical errors. The annual National Patient Safety Goals are also set by The Joint Commission after reviewing emerging patient safety issues.[10]
The Centers for Medicare & Medicaid Services (CMS) is an example of another federal agency that establishes regulations affecting nursing care. CMS is a part of the U.S. Department of Health and Human Services (HHS) that administers the Medicare program and works in partnership with state governments to administer Medicaid. The CMS establishes and enforces regulations to protect patient safety in hospitals that receive Medicare and Medicaid funding. For example, one CMS regulation often referred to as “checking the rights of medication administration” requires nurses to confirm specific information several times before medication is administered to a patient.[11]
Standards of Practice
The ANA defines Standards of Professional Nursing Practice as “authoritative statements of the actions and behaviors that all registered nurses, regardless of role, population, specialty, and setting, are expected to perform competently.”[12] These standards are classified into two categories: Standards of Practice and Standards of Professional Performance.
The ANA’s Standards of Practice describe a competent level of nursing practice as demonstrated by the critical thinking model known as the nursing process. The nursing process includes the components of assessment, diagnosis, outcomes identification, planning, implementation, and evaluation and forms the foundation of the nurse’s decision-making, practice, and provision of care.[13]
The ANA’s Standards of Professional Performance “describe a competent level of behavior in the professional role, including activities related to ethics, advocacy, respectful and equitable practice, communication, collaboration, leadership, education, scholarly inquiry, quality of practice, professional practice evaluation, resource stewardship, and environmental health. All registered nurses are expected to engage in professional role activities, including leadership, reflective of their education, position, and role.”[14] This book discusses content related to these professional practice standards. Each professional practice standard is defined in the following sections with information provided to related content in this book and the Open RN Nursing Fundamentals, 2e textbook.[15]
Ethics
The ANA’s Ethics standard states, “The registered nurse integrates ethics in all aspects of practice.”[16]
Advocacy
The ANA’s Advocacy standard states, “The registered nurse demonstrates advocacy in all roles and settings.”[17]
Respectful and Equitable Practice
The ANA’s Respectful and Equitable Practice standard states, “The registered nurse practices with cultural humility and inclusiveness.”
Communication
The ANA’s Communication standard states, “The registered nurse communicates effectively in all areas of professional practice.”[18]
Collaboration
The ANA’s Collaboration standard states, “The registered nurse collaborates with the health care consumer and other key stakeholders.”[19]
Leadership
The ANA’s Leadership standard states, “The registered nurse leads within the profession and practice setting.”[20]
Education
The ANA’s Education standard states, “The registered nurse seeks knowledge and competence that reflects current nursing practice and promotes futuristic thinking.”[21]
Scholarly Inquiry
The ANA’s Scholarly Inquiry standard states, “The registered nurse integrates scholarship, evidence, and research findings into practice.”[22]
Quality of Practice
The ANA’s Quality of Practice standard states, “The nurse contributes to quality nursing practice.”[23]
Professional Practice Evaluation
The ANA’s Professional Practice Evaluation standard states, “The registered nurse evaluates one’s own and others’ nursing practice.”[24]
Resource Stewardship
The ANA’s Resource Stewardship standard states, “The registered nurse utilizes appropriate resources to plan, provide, and sustain evidence-based nursing services that are safe, effective, financially responsible, and used judiciously.”[25]
Environmental Health
The ANA’s Environmental Health standard states, “The registered nurse practices in a manner that advances environmental safety and health.”[26]
Outcome Identification is the third step of the nursing process (and the third Standard of Practice by the American Nurses Association). This standard is defined as, "The registered nurse identifies expected outcomes for a plan individualized to the health care consumer or the situation." The RN collaborates with the health care consumer, interprofessional team, and others to identify expected outcomes integrating the health care consumer's culture, values, and ethical considerations. Expected outcomes are documented as measurable goals with a time frame for attainment.[27] Outcome identification is performed by RNs and is outside the scope of practice for LPN/VNs, but LPN/VNs must be aware of expected outcomes for clients in their nursing care plan.
An outcome is a “measurable behavior demonstrated by the client's response to nursing interventions.”[28] Outcomes should be identified before nursing interventions are planned. After nursing interventions are implemented, the nurse will evaluate if the outcomes were met in the time frame indicated for that client.
Outcome identification includes setting short- and long-term goals and then creating specific expected outcome statements for each nursing diagnosis. See Figure 4.9a for an illustration of how the Outcome Identification phase of the nursing process correlates to the NCSBN Clinical Judgment Model.[29]

Short-Term and Long-Term Goals
Nursing care should always be individualized and client centered. No two people are the same, and neither should nursing care plans be the same for two people. Goals and outcomes should be tailored specifically to each client’s needs, values, and cultural beliefs. Clients and family members should be included in the goal-setting process when feasible. Involving clients and family members promotes awareness of identified needs, ensures realistic goals, and motivates their participation in the treatment plan to achieve the mutually agreed upon goals and live life to the fullest with their current condition.
The nursing care plan is a road map used to guide client care so that all health care providers are moving toward the same client goals. Goals are broad statements of purpose that describe the overall aim of care. Goals can be short- or long-term. The time frame for short- and long-term goals is dependent on the setting in which the care is provided. For example, in a critical care area, a short-term goal might be set to be achieved within an 8-hour nursing shift, and a long-term goal might be in 24 hours. In contrast, in an outpatient setting, a short-term goal might be set to be achieved within one month and a long-term goal might be within six months.
A nursing goal is the overall direction in which the client must progress to improve the problem/nursing diagnosis and is often the opposite of the problem.
Example of a Broad Goal
Refer to Scenario C in the "Assessment" section of this chapter. Ms. J. had a priority nursing diagnosis of Excess Fluid Volume. A broad goal would be, “Ms. J. will achieve a state of fluid balance.”
Expected Outcomes
Goals are broad, general statements, but outcomes are specific and measurable. Expected outcomes are statements of measurable action for the client within a specific time frame that are responsive to nursing interventions. Nurses may create expected outcomes independently or refer to classification systems for assistance. Just as NANDA-I creates and revises standardized nursing diagnoses, a similar classification and standardization process exists for expected nursing outcomes. The Nursing Outcomes Classification (NOC) is a list of over 330 nursing outcomes designed to coordinate with established NANDA-I diagnoses.[30]
Client-Centered
Outcome statements are always client-centered. They should be developed in collaboration with the client and individualized to meet a client’s unique needs, values, and cultural beliefs. They should start with the phrase “The client will…” Outcome statements should be directed at resolving the defining characteristics the client is exhibiting for the nursing diagnosis. Additionally, the outcome must be something the client would like to achieve.
Outcome statements should contain five components easily remembered using the "SMART" mnemonic:[31]
- Specific
- Measurable
- Attainable/Action oriented
- Relevant/Realistic
- Timeframe
See Figure 4.9[32] for an image of the SMART components of outcome statements. Each of these components is further described in the following subsections.

Specific
Outcome statements should state precisely what is to be accomplished. See examples of a not specific and a specific outcome in the following box.
Example
- Not specific outcome: "The client will increase the amount of exercise."
- Revised as a specific outcome: "The client will participate in a bicycling exercise session daily for 30 minutes."
Additionally, only one action should be included in each expected outcome. See examples in the following box.
Example
- More than one action: "The client will walk 50 feet three times a day with standby assistance of one and will shower in the morning until discharge" is actually two goals written as one. The outcome of ambulation should be separate from showering for precise evaluation. For instance, the client could shower but not ambulate, which would make this outcome statement very difficult to effectively evaluate.
- Revised to create two outcome statements so each can be measured: The client will walk 50 feet three times a day with standby assistance of one until discharge. The client will shower every morning until discharge.
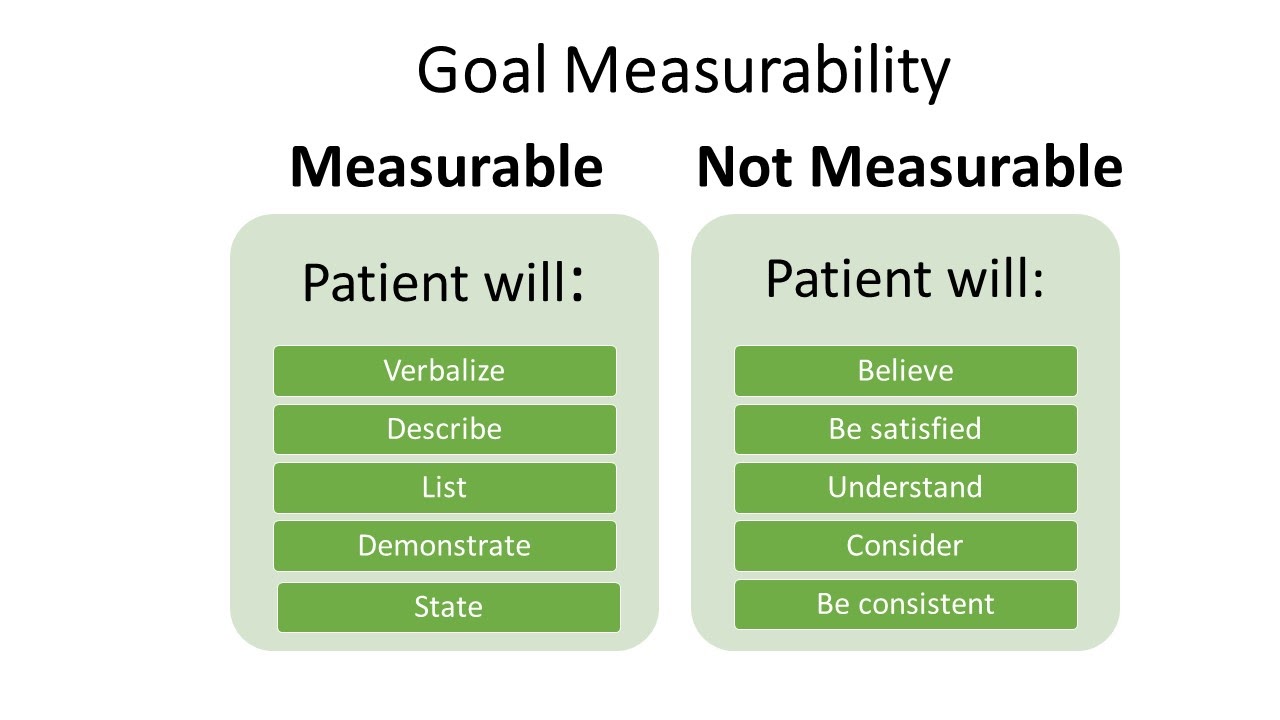
Measurable
Measurable outcomes have numeric parameters or other concrete methods of judging whether the outcome was met. It is important to use objective data to measure outcomes. If terms like “acceptable” or “normal” are used in an outcome statement, it is difficult to determine whether the outcome is attained. Refer to Figure 4.10[33] for examples of verbs that are measurable and not measurable in outcome statements.
Examples of a non-measurable outcome revised to a measurable outcome is described in the following box.
Example
- Not measurable outcome: "The client will drink adequate fluid amounts every shift."
- Revised into a measurable outcome: "The client will drink 24 ounces of fluids during every day shift (0600-1400)."
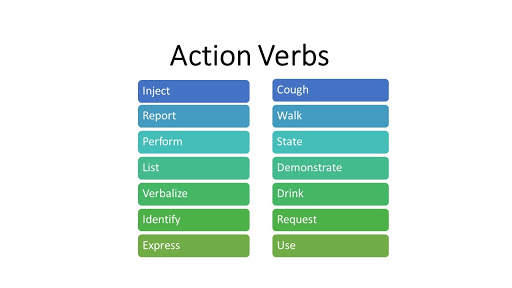
Action-Oriented and Attainable
Outcome statements should be written so that there is a clear action to be taken by the client or significant others. This means that the outcome statement should include a verb. Refer to Figure 4.11[34] for examples of action verbs.
An example of a non-action-oriented outcome revised to an action-oriented outcome is provided in the following box.
Example
- Not action-oriented outcome: "The client will get increased physical activity."
- Revised into an action-oriented outcome: "The client will list three types of aerobic activity that he would enjoy completing every week."
Realistic and Relevant
Realistic outcomes consider the client’s physical and mental condition; their cultural and spiritual values, beliefs, and preferences; and their socioeconomic status in terms of their ability to attain these outcomes. Consideration should be also given to disease processes and the effects of conditions such as pain and decreased mobility on the client's ability to reach expected outcomes. Other barriers to outcome attainment may be related to health literacy or lack of available resources. Outcomes should always be reevaluated and revised for attainability as needed. If an outcome is not attained, it is commonly because the original time frame was too ambitious, or the outcome was not realistic for the client.
See an example of how to revise an outcome that is not realistic into a realistic outcome in the following box.
Example
- Not realistic outcome: "The client will jog one mile every day when starting the exercise program."
- Revised into a realistic outcome: "The client will walk ½ mile three times a week for two weeks."
Time Limited
Outcome statements should include a time frame for evaluation. The time frame depends on the intervention and the client's current condition. Some outcomes may need to be evaluated every shift, whereas other outcomes may be evaluated daily, weekly, or monthly. During the evaluation phase of the nursing process, the outcomes will be assessed according to the time frame specified for evaluation. If it has not been met, the nursing care plan should be revised.
See an example an outcome that is not time limited revised into a time limited outcome in the following box.
Example
- Not time limited: "The client will stop smoking cigarettes."
- Time limited: "The client will complete the smoking cessation plan by December 12, 2025."
Putting It Together
An example of a SMART outcome for Scenario C is provided in the following box.
Example of a SMART Expected Outcome
Refer to Scenario C in the "Assessment" section of this chapter. Ms. J.’s priority nursing diagnosis statement was Excess Fluid Volume related to excess fluid intake as manifested by bilateral basilar crackles in the lungs, bilateral 2+ pitting edema of the ankles and feet, an increase weight of ten pounds, and the client reports, “My ankles are so swollen.”
The broad goal was, “Ms. J. will achieve a state of fluid balance.”
An example of a SMART expected outcome to achieve this broad goal is, “The client will have clear bilateral lung sounds within the next 24 hours.”
This chapter introduces concepts related to nursing leadership and management, prioritization strategies, delegation and supervision, legal implications of nursing practice, ethical nursing practice, collaboration within the interprofessional team, health care economics, quality and evidence-based practice, advocacy, preparation for the RN role, and the avoidance of burnout with self-care.
ADOPIE: An easy way to remember the ANA Standards and the nursing process. Each letter refers to the six components of the nursing process: Assessment, Diagnosis, Outcomes Identification, Planning, Implementation, and Evaluation. (Chapter 4.2)
Art of nursing: Unconditionally acceptance of the humanity of others, respecting their need for dignity and worth, while providing compassionate, comforting care.[35] (Chapter 4.2)
At-risk populations: Groups of people who share a characteristic that causes each member to be susceptible to a particular human response, such as demographics, health/family history, stages of growth/development, or exposure to certain events/experiences.[36] (Chapter 4.4)
Associated conditions: Medical diagnoses, injuries, procedures, medical devices, or pharmacological agents. These conditions are not independently modifiable by the nurse, but support accuracy in nursing diagnosis.[37] (Chapter 4.4)
Care relationship: A relationship described as one in which the whole person is assessed while balancing the vulnerability and dignity of the client and family.[38] (Chapter 4.2)
Client: Individual, family, or group, which includes significant others and populations.[39] (Chapter 4.2)
Clinical judgment: The observed outcome of critical thinking and decision-making. It is an iterative process that uses nursing knowledge to observe and access presenting situations, identify a prioritized client concern, and generate the best possible evidence-based solutions in order to deliver safe client care.[40] (Chapter 4.2)
Clinical reasoning: A complex cognitive process that uses formal and informal thinking strategies to gather and analyze client information, evaluate the significance of this information, and weigh alternative actions. [41] (Chapter 4.2)
Clustering data: Grouping data into similar domains or patterns. (Chapter 4.4)
Collaborative nursing interventions: Nursing interventions that require cooperation among health care professionals and unlicensed assistive personnel (UAP). (Chapter 4.6)
Coordination of care: While implementing interventions during the nursing process, includes competencies such as organizing the components of the plan with input from the health care consumer, engaging the client in self-care to achieve goals, and advocating for the delivery of dignified and person-centered care by the interprofessional team.[42] (Chapter 4.7)
Critical thinking: Reasoning about clinical issues such as teamwork, collaboration, and streamlining workflow.[43] (Chapter 4.2)
Cues: Subjective or objective data that gives the nurse a hint or indication of a potential problem, process, or disorder. (Chapter 4.2)
Deductive reasoning: “Top-down thinking” or moving from the general to the specific. Deductive reasoning relies on a general statement or hypothesis—sometimes called a premise or standard—that is held to be true. The premise is used to reach a specific, logical conclusion. (Chapter 4.2)
Defining characteristics: Observable cues/inferences that cluster as manifestations of a problem-focused, health-promotion diagnosis, or syndrome. This does not only imply those things that the nurse can see, but also things that are seen, heard (e.g., the client/family tells us), touched, or smelled.[44] (Chapter 4.4)
Delegation: The assignment of the performance of activities or tasks related to client care to unlicensed assistive personnel while retaining accountability for the outcome.[45] (Chapter 4.7)
Dependent nursing interventions: Interventions that require a prescription from a physician, advanced practice nurse, or physician’s assistant. (Chapter 4.6)
Direct care: Interventions that are carried out by having personal contact with a client. (Chapter 4.6)
Electronic Medical Record (EMR): An electronic version of the client’s medical record. (Chapter 4.3)
Evidence-Based Practice (EBP): A lifelong problem-solving approach that integrates the best evidence from well-designed research studies and evidence-based theories; clinical expertise and evidence from assessment of the health care consumer’s history and condition, as well as health care resources; and client, family, group, community, and population preferences and values.[46] (Chapter 4.2)
Expected outcomes: Statements of measurable action for the client within a specific time frame and in response to nursing interventions. “SMART” outcome statements are specific, measurable, action-oriented, realistic, and include a time frame. (Chapter 4.5)
Functional Health Patterns: An evidence-based assessment framework for identifying client problems and risks during the assessment phase of the nursing process. (Chapter 4.4)
Generalization: A judgment formed from a set of facts, cues, and observations. (Chapter 4.2)
Goals: Broad statements of purpose that describe the aim of nursing care. (Chapter 4.5)
Health promotion-wellness nursing diagnosis: A clinical judgment concerning motivation and desire to increase well-being and to actualize human health potential. (Chapter 4.4)
Health teaching and health promotion: Employing strategies to teach and promote health and wellness.[47] (Chapter 4.7)
Hypothesis: A proposed explanation for a situation. It attempts to explain the “why” behind the problem that is occurring. (Chapter 4.2)
Independent nursing interventions: Any intervention that the nurse can provide without obtaining a prescription or consulting anyone else. (Chapter 4.6)
Indirect care: Interventions performed by the nurse in a setting other than directly with the client. An example of indirect care is creating a nursing care plan. (Chapter 4.6)
Inductive reasoning: A type of reasoning that involves forming generalizations based on specific incidents. (Chapter 4.2)
Inference: Interpretations or conclusions based on cues, personal experiences, preferences, or generalizations. (Chapter 4.3)
Licensed Practical Nurses or Licensed Vocational Nurses (LPNs/LVNs): Nurses who have had specific training and passed a licensing exam. The training is generally less than that of a Registered Nurse. The scope of practice of an LPN/LVN is determined by the facility and the state’s Nurse Practice Act. (Chapter 4.3)
Maslow’s Hierarchy of Needs: A theory used to prioritize the most urgent client needs to address first. The bottom levels of the pyramid represent the most important physiological needs intertwined with safety. (Chapter 4.4)
Medical diagnosis: A disease or illness diagnosed by a physician or advanced health care provider such as a nurse practitioner or physician’s assistant. Medical diagnoses are a result of clustering signs and symptoms to determine what is medically affecting an individual. (Chapter 4.3)
Nursing: Nursing integrates the art and science of caring and focuses on the protection, promotion, and optimization of health and human functioning; prevention of illness and injury; facilitation of healing; and alleviation of suffering through compassionate presence. Nursing is the diagnosis and treatment of human responses and advocacy in the care of individuals, families, groups, communities, and populations in the recognition of the connection of all humanity.[48] (Chapter 4.2)
Nursing care plan: Specific documentation of the planning and delivery of nursing care that is required by The Joint Commission. (Chapter 4.2)
Nursing diagnosis: A clinical judgment concerning a human response to health conditions/life processes, or a vulnerability for that response, by an individual, family, group, or community. (Chapter 4.4)
Nursing interventions: Evidence-based actions that the nurse performs to achieve client outcomes. (Chapter 4.6)
Nursing process: A systematic approach to client-centered care with steps including assessment, diagnosis, outcome identification, planning, implementation, and evaluation; otherwise known by the mnemonic “ADOPIE.” (Chapter 4.1)
Objective data: Data that the nurse can see, touch, smell, or hear or is reproducible such as vital signs. Laboratory and diagnostic results are also considered objective data. (Chapter 4.3)
Order: An intervention, remedy or treatment as directed by an authorized primary health care provider.[49] (Chapter 4.6)
Outcome: A measurable behavior demonstrated by the client's response to nursing interventions.[50] (Chapter 4.5)
PES format: The format of a nursing diagnosis statement that includes:
- Problem (P) - statement of the client problem (i.e., the nursing diagnosis)
- Etiology (E) - related factors (etiology) contributing to the cause of the nursing diagnosis
- Signs and Symptoms (S) - defining characteristics manifested by the client of that nursing diagnosis (Chapter 4.4)
Physical examination: A systematic data collection method of the body that uses the techniques of inspection, auscultation, palpation, and percussion. (Chapter 4.3)
Prescription: Intervention as it relates to medication specifically as directed by an authorized primary health care provider.[51] (Chapter 4.6)
Primary data: Information collected from the client. (Chapter 4.3)
Primary health care provider: Member of the health care team (usually a medical physician, nurse practitioner, etc.) licensed and authorized to formulate prescriptions on behalf of the client.[52] (Chapter 4.6)
Prioritization: The skillful process of deciding which actions to complete first for client safety and optimal client outcomes. (Chapter 4.4)
Problem-focused nursing diagnosis: A clinical judgment concerning an undesirable human response to health condition/life processes that exist in an individual, family, group, or community. (Chapter 4.4)
Quality improvement: The “combined and unceasing efforts of everyone -- health care professionals, clients and their families, researchers, payers, planners, and educators -- to make the changes that will lead to better client outcomes (health), better system performance (care), and better professional development (learning).”[53] (Chapter 4.7)
Rapport: Developing a relationship of mutual trust and understanding. (Chapter 4.2)
Registered Nurse (RN): A nurse who has had a designated amount of education and training in nursing and is licensed by a state Board of Nursing. (Chapter 4.3)
Related factors: The underlying cause (etiology) of a nursing diagnosis. (Chapter 4.4)
Risk nursing diagnosis: A clinical judgment concerning the vulnerability of an individual, family, group, or community for developing an undesirable human response to health conditions/life processes. (Chapter 4.4)
Secondary data: Information collected from sources other than the client. (Chapter 4.3)
Subjective data: Data that the client or family reports or data that the nurse makes as an inference, conclusion, or assumption, such as “The client appears anxious.” (Chapter 4.3)
Syndrome nursing diagnosis: A clinical judgment concerning a specific cluster of nursing diagnoses that occur together and are best addressed together and through similar interventions. (Chapter 4.4)
Unlicensed Assistive Personnel (UAP): Any unlicensed personnel trained to function in a supportive role, regardless of title, to whom a nursing responsibility may be delegated.[54] (Chapter 4.3)
Planning is the fourth step of the nursing process (and the fourth Standard of Practice by the American Nurses Association). This standard is defined as, "The registered nurse develops a collaborative plan encompassing strategies to achieve expected outcomes." The RN develops an individualized, holistic, evidence-based plan in partnership with the health care consumer, family, significant others, and interprofessional team. Elements of the plan are prioritized for client safety and optimal client outcomes. The plan is modified according to the ongoing assessment of the health care consumer's response and other indicators. The plan is documented using standardized language or terminology.[55]
After expected outcomes are identified, the nurse begins planning nursing interventions to implement. Nursing interventions are evidence-based actions that the nurse performs to achieve client outcomes. Just as a provider makes medical diagnoses and writes prescriptions to improve the client's medical condition, a nurse formulates nursing diagnoses and plans nursing interventions to resolve client problems. Nursing interventions should focus on eliminating or reducing the related factors (etiology) of the nursing diagnoses when possible.[56] Nursing interventions, goals, and expected outcomes are written in the nursing care plan for continuity of care across shifts, nurses, and health professionals. Planning is outside the scope of practice for LPN/VNs, although they may assist in performing planned interventions during the Implementation phase according to their scope of practice. Refer to Figure 4.9a in the "Outcome Identification" section for a illustration of how the Planning phase of the nursing process correlates to NCSBN's Clinical Judgment Measurement Model.
Planning Nursing Interventions
You might be asking yourself, “How do I know what evidence-based nursing interventions to include in the nursing care plan?” There are several sources that nurses and nursing students can use to select nursing interventions. Many agencies have care planning tools and references included in the electronic health record that are easily documented in the client chart. Nurses can also refer to other care planning books or sources such as the Nursing Interventions Classification (NIC) system. Based on research and input from the nursing profession, NIC categorizes and describes nursing interventions that are regularly evaluated and updated. Interventions included in NIC are considered evidence-based nursing practices. The RN is responsible for using clinical judgment to make decisions about which interventions are best suited to meet an individualized client’s needs.[57]
Direct and Indirect Care
Nursing interventions are considered direct care or indirect care. Direct care refers to interventions that are carried out by having personal contact with clients. Examples of direct care interventions are wound care, repositioning, and ambulation. Indirect care interventions are performed when the nurse provides assistance in a setting other than with the client. Examples of indirect care interventions are attending care conferences, documenting, and communicating about client care with other providers.
Classification of Nursing Interventions
There are three types of nursing interventions: independent, dependent, and collaborative. (See Figure 4.12[58] for an image of a nurse collaborating with the health care team when planning interventions.)

Independent Nursing Interventions
Any intervention that the nurse can independently provide without obtaining a prescription or consulting another member of the health care team is considered an independent nursing intervention. An example of an independent nursing intervention is when the nurse monitors the client’s 24-hour intake/output record for trends because of a risk for imbalanced fluid volume. Another example of independent nursing interventions is the therapeutic communication that a nurse uses to assist clients to cope with a new medical diagnosis.
Example of an Independent Nursing Intervention
Refer to Scenario C in the "Assessment" section of this chapter. Ms. J. was diagnosed with Excess Fluid Volume. An example of an evidence-based independent nursing intervention is, “The nurse will reposition the client with dependent edema frequently, as appropriate.”[59] The nurse would individualize this evidence-based intervention to the client and include agency policy by stating, “The nurse will reposition the client every two hours.”
Dependent Nursing Interventions
Dependent nursing interventions require a prescription or order before they can be performed. Prescriptions are interventions specifically related to medication as directed by an authorized primary health care provider. An order is an intervention, remedy, or treatment as directed by an authorized primary health care provider.[60] A primary health care provider is a member of the health care team (usually a physician, advanced practice nurse, or physician’s assistant) who is licensed and authorized to formulate prescriptions on behalf of the client. For example, administering medication is a dependent nursing intervention. The nurse incorporates dependent interventions into the client's overall care plan by associating each intervention with the appropriate nursing diagnosis.
Example of a Dependent Nursing Intervention
Refer to Scenario C in the "Assessment" section of this chapter. Ms. J. was diagnosed with Excess Fluid Volume. An example of a dependent nursing intervention is, “The nurse will administer scheduled diuretics as prescribed.”
Collaborative Nursing Interventions
Collaborative nursing interventions are actions that the nurse carries out in collaboration with other health team members, such as physicians, social workers, respiratory therapists, physical therapists, and occupational therapists. These actions are developed in consultation with other health care professionals and incorporate their professional viewpoint.[61]
Example of a Collaborative Nursing Intervention
Refer to Scenario C in the "Assessment" section of this chapter. Ms. J. was diagnosed with Excess Fluid Volume. An example of a collaborative nursing intervention is the nurse consulting with a respiratory therapist when the client has deteriorating oxygen saturation levels. The respiratory therapist plans oxygen therapy and obtains a prescription from the provider. The nurse would document “The nurse will manage oxygen therapy in collaboration with the respiratory therapist" in the care plan.
Individualization of Interventions
It is vital for the planned interventions to be individualized to the client to be successful. For example, adding prune juice to the breakfast meal of a client with constipation will only work if the client likes to drink the prune juice. If the client does not like prune juice, then this intervention should not be included in the care plan. Collaboration with the client, family members, significant others, and the interprofessional team is essential for selecting effective interventions. There is not a set number of interventions required to be included in a nursing care plan, but instead, the number of quality individualized interventions is based on what is required to meet the specific, identified outcomes established for that client.
Creating Nursing Care Plans
Nursing care plans are created by registered nurses (RNs). Documentation of individualized nursing care plans are legally required in long-term care facilities by the Centers for Medicare and Medicaid Services (CMS) and in hospitals by The Joint Commission. CMS guidelines state, “Residents and their representative(s) must be afforded the opportunity to participate in their care planning process and to be included in decisions and changes in care, treatment, and/or interventions. This applies both to initial decisions about care and treatment, as well as the refusal of care or treatment. Facility staff must support and encourage participation in the care planning process. This may include ensuring that residents, families, or representatives understand the comprehensive care planning process, holding care planning meetings at the time of day when a resident is functioning at their best and client representatives can be present, providing sufficient notice in advance of the meeting, scheduling these meetings to accommodate a resident’s representative (such as conducting the meeting in-person, via a conference call, or video conferencing), and planning enough time for information exchange and decision-making. A resident has the right to select or refuse specific treatment options before the care plan is instituted.”[62] The Joint Commission conceptualizes the care planning process as the structuring framework for coordinating communication that will result in safe and effective care.[63]
Many facilities have established standardized nursing care plans with lists of possible interventions that can be customized for each specific client. Other facilities require the nurse to develop each care plan independently. Whatever the format, nursing care plans should be individualized to meet the specific and unique needs of each client. See Figure 4.13[64] for an image of a standardized care plan.

Nursing care plans created in nursing school can also be in various formats such as concept maps or tables. Some are fun and creative, while others are more formal. Appendix B contains a template that can be used for creating nursing care plans.
Planning is the fourth step of the nursing process (and the fourth Standard of Practice by the American Nurses Association). This standard is defined as, "The registered nurse develops a collaborative plan encompassing strategies to achieve expected outcomes." The RN develops an individualized, holistic, evidence-based plan in partnership with the health care consumer, family, significant others, and interprofessional team. Elements of the plan are prioritized for client safety and optimal client outcomes. The plan is modified according to the ongoing assessment of the health care consumer's response and other indicators. The plan is documented using standardized language or terminology.[65]
After expected outcomes are identified, the nurse begins planning nursing interventions to implement. Nursing interventions are evidence-based actions that the nurse performs to achieve client outcomes. Just as a provider makes medical diagnoses and writes prescriptions to improve the client's medical condition, a nurse formulates nursing diagnoses and plans nursing interventions to resolve client problems. Nursing interventions should focus on eliminating or reducing the related factors (etiology) of the nursing diagnoses when possible.[66] Nursing interventions, goals, and expected outcomes are written in the nursing care plan for continuity of care across shifts, nurses, and health professionals. Planning is outside the scope of practice for LPN/VNs, although they may assist in performing planned interventions during the Implementation phase according to their scope of practice. Refer to Figure 4.9a in the "Outcome Identification" section for a illustration of how the Planning phase of the nursing process correlates to NCSBN's Clinical Judgment Measurement Model.
Planning Nursing Interventions
You might be asking yourself, “How do I know what evidence-based nursing interventions to include in the nursing care plan?” There are several sources that nurses and nursing students can use to select nursing interventions. Many agencies have care planning tools and references included in the electronic health record that are easily documented in the client chart. Nurses can also refer to other care planning books or sources such as the Nursing Interventions Classification (NIC) system. Based on research and input from the nursing profession, NIC categorizes and describes nursing interventions that are regularly evaluated and updated. Interventions included in NIC are considered evidence-based nursing practices. The RN is responsible for using clinical judgment to make decisions about which interventions are best suited to meet an individualized client’s needs.[67]
Direct and Indirect Care
Nursing interventions are considered direct care or indirect care. Direct care refers to interventions that are carried out by having personal contact with clients. Examples of direct care interventions are wound care, repositioning, and ambulation. Indirect care interventions are performed when the nurse provides assistance in a setting other than with the client. Examples of indirect care interventions are attending care conferences, documenting, and communicating about client care with other providers.
Classification of Nursing Interventions
There are three types of nursing interventions: independent, dependent, and collaborative. (See Figure 4.12[68] for an image of a nurse collaborating with the health care team when planning interventions.)

Independent Nursing Interventions
Any intervention that the nurse can independently provide without obtaining a prescription or consulting another member of the health care team is considered an independent nursing intervention. An example of an independent nursing intervention is when the nurse monitors the client’s 24-hour intake/output record for trends because of a risk for imbalanced fluid volume. Another example of independent nursing interventions is the therapeutic communication that a nurse uses to assist clients to cope with a new medical diagnosis.
Example of an Independent Nursing Intervention
Refer to Scenario C in the "Assessment" section of this chapter. Ms. J. was diagnosed with Excess Fluid Volume. An example of an evidence-based independent nursing intervention is, “The nurse will reposition the client with dependent edema frequently, as appropriate.”[69] The nurse would individualize this evidence-based intervention to the client and include agency policy by stating, “The nurse will reposition the client every two hours.”
Dependent Nursing Interventions
Dependent nursing interventions require a prescription or order before they can be performed. Prescriptions are interventions specifically related to medication as directed by an authorized primary health care provider. An order is an intervention, remedy, or treatment as directed by an authorized primary health care provider.[70] A primary health care provider is a member of the health care team (usually a physician, advanced practice nurse, or physician’s assistant) who is licensed and authorized to formulate prescriptions on behalf of the client. For example, administering medication is a dependent nursing intervention. The nurse incorporates dependent interventions into the client's overall care plan by associating each intervention with the appropriate nursing diagnosis.
Example of a Dependent Nursing Intervention
Refer to Scenario C in the "Assessment" section of this chapter. Ms. J. was diagnosed with Excess Fluid Volume. An example of a dependent nursing intervention is, “The nurse will administer scheduled diuretics as prescribed.”
Collaborative Nursing Interventions
Collaborative nursing interventions are actions that the nurse carries out in collaboration with other health team members, such as physicians, social workers, respiratory therapists, physical therapists, and occupational therapists. These actions are developed in consultation with other health care professionals and incorporate their professional viewpoint.[71]
Example of a Collaborative Nursing Intervention
Refer to Scenario C in the "Assessment" section of this chapter. Ms. J. was diagnosed with Excess Fluid Volume. An example of a collaborative nursing intervention is the nurse consulting with a respiratory therapist when the client has deteriorating oxygen saturation levels. The respiratory therapist plans oxygen therapy and obtains a prescription from the provider. The nurse would document “The nurse will manage oxygen therapy in collaboration with the respiratory therapist" in the care plan.
Individualization of Interventions
It is vital for the planned interventions to be individualized to the client to be successful. For example, adding prune juice to the breakfast meal of a client with constipation will only work if the client likes to drink the prune juice. If the client does not like prune juice, then this intervention should not be included in the care plan. Collaboration with the client, family members, significant others, and the interprofessional team is essential for selecting effective interventions. There is not a set number of interventions required to be included in a nursing care plan, but instead, the number of quality individualized interventions is based on what is required to meet the specific, identified outcomes established for that client.
Creating Nursing Care Plans
Nursing care plans are created by registered nurses (RNs). Documentation of individualized nursing care plans are legally required in long-term care facilities by the Centers for Medicare and Medicaid Services (CMS) and in hospitals by The Joint Commission. CMS guidelines state, “Residents and their representative(s) must be afforded the opportunity to participate in their care planning process and to be included in decisions and changes in care, treatment, and/or interventions. This applies both to initial decisions about care and treatment, as well as the refusal of care or treatment. Facility staff must support and encourage participation in the care planning process. This may include ensuring that residents, families, or representatives understand the comprehensive care planning process, holding care planning meetings at the time of day when a resident is functioning at their best and client representatives can be present, providing sufficient notice in advance of the meeting, scheduling these meetings to accommodate a resident’s representative (such as conducting the meeting in-person, via a conference call, or video conferencing), and planning enough time for information exchange and decision-making. A resident has the right to select or refuse specific treatment options before the care plan is instituted.”[72] The Joint Commission conceptualizes the care planning process as the structuring framework for coordinating communication that will result in safe and effective care.[73]
Many facilities have established standardized nursing care plans with lists of possible interventions that can be customized for each specific client. Other facilities require the nurse to develop each care plan independently. Whatever the format, nursing care plans should be individualized to meet the specific and unique needs of each client. See Figure 4.13[74] for an image of a standardized care plan.

Nursing care plans created in nursing school can also be in various formats such as concept maps or tables. Some are fun and creative, while others are more formal. Appendix B contains a template that can be used for creating nursing care plans.
Learning Activities
(Answers to "Learning Activities" can be found in the "Answer Key" at the end of the book. Answers to interactive activity elements will be provided within the element as immediate feedback.)
Instructions: Apply what you’ve learned in this chapter by creating a nursing care plan using the following scenario. Use the template in Appendix B as a guide.
The client, Mark S., is a 57-year-old male who was admitted to the hospital with “severe” abdominal pain that was unable to be managed in the Emergency Department. The physician has informed Mark that he will need to undergo some diagnostic tests. The tests are scheduled for the morning.
After receiving the news about his condition and the need for diagnostic tests, Mark begins to pace the floor. He continues to pace constantly. He keeps asking the nurse the same question (“How long will the tests take?”) about his tests over and over again. The client also remarked, “I’m so uptight I will never be able to sleep tonight.” The nurse observes that the client avoids eye contact during their interactions and that he continually fidgets with the call light. His eyes keep darting around the room. He appears tense and has a strained expression on his face. He states, “My mouth is so dry.” The nurse observes his vital signs to be: T 98, P 104, R 30, BP 180/96. The nurse notes that his skin feels sweaty (diaphoretic) and cool to the touch.
Critical Thinking Activity:
-
- Group (cluster) the cues (subjective and objective data).
- Create a problem-focused nursing diagnosis (hypothesis).
- Develop a broad goal and then identify an expected outcome in “SMART” format.
- Outline three interventions for the nursing diagnosis to meet the goal and their rationale. Cite an evidence-based source for the interventions and rationale
- Imagine that you implemented the interventions that you identified. Evaluate the degree to which the expected outcome was achieved: Met - Partially Met - Not Met.

Test your knowledge using this NCLEX Next Generation-style question. You may reset and resubmit your answers to this question an unlimited number of times.[75]
Implementation is the fifth step of the nursing process (and the fifth Standard of Practice by the American Nurses Association). This standard is defined as, "The registered nurse implements the identified plan." The RN may delegate planned interventions after considering the circumstance, person, task, communication, supervision, and evaluation, as well as the state Nurse Practice Act, federal regulation, and agency policy.[76]
Implementation of interventions requires the RN to use critical thinking and clinical judgment. After the initial plan of care is developed, continual reassessment of the client is necessary to detect any changes in the client’s condition requiring modification of the plan. The need for continual client reassessment underscores the dynamic nature of the nursing process and is crucial to providing safe care.
During the implementation phase of the nursing process, the nurse prioritizes planned interventions, assesses client safety while implementing interventions, delegates interventions as appropriate, and documents interventions performed. LPN/VNs have an active role in the Implementation phase, provided the interventions falls within the LPN/VN scope of practice. See Figure 4.14 for an illustration of how the Implementation phase of the nursing process correlates to NCSBN's Clinical Judgment Measurement Model.[77]
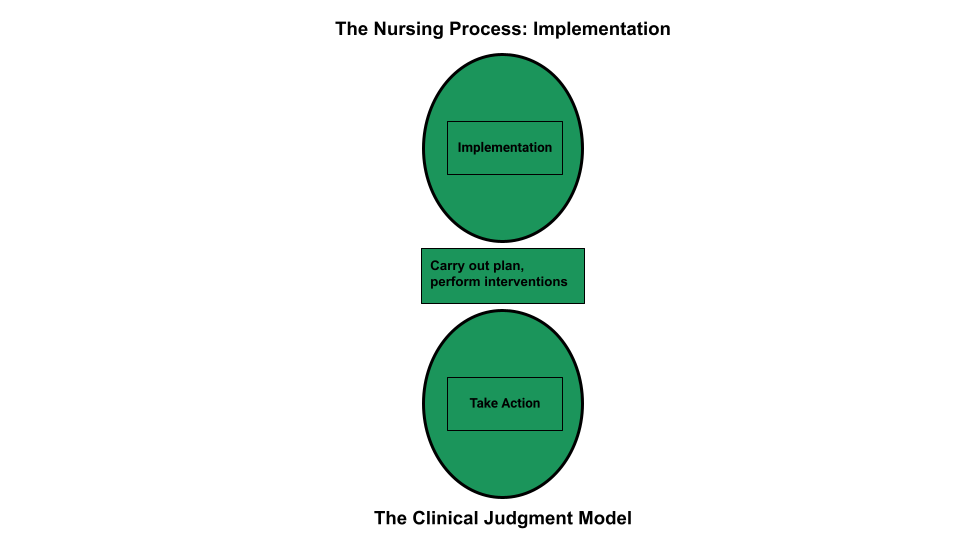
Prioritizing Implementation of Interventions
Prioritizing implementation of interventions follows a similar method as to prioritizing nursing diagnoses. Maslow’s Hierarchy of Needs and the ABCs of airway, breathing, and circulation are used to establish top priority interventions. When possible, least invasive actions are usually preferred due to the risk of injury from invasive options. Read more about methods for prioritization under the “Diagnosis” section of this chapter.
The potential impact on future events, especially if a task is not completed at a certain time, is also included when prioritizing nursing interventions. For example, if a client is scheduled to undergo a surgical procedure later in the day, the nurse prioritizes initiating a NPO (nothing by mouth) prescription prior to completing pre-op client education about the procedure. The rationale for this decision is that if the client eats food or drinks water, the surgery time will be delayed. Knowing and understanding the client's purpose for care, current situation, and expected outcomes are necessary to accurately prioritize interventions.
Client Safety
It is essential to consider client safety when implementing interventions. At times, clients may experience a change in condition that makes a planned nursing intervention or provider prescription no longer safe to implement. For example, an established nursing care plan for a client states, “The nurse will ambulate the client 100 feet three times daily.” However, during assessment this morning, the client reports feeling dizzy today, and their blood pressure is 90/60. Using critical thinking and clinical judgment, the nurse decides to not implement the planned intervention of ambulating the client. This decision and supporting assessment findings should be documented in the client’s chart and also communicated during the shift handoff report, along with appropriate notification of the provider of the client’s change in condition.
Implementing interventions goes far beyond implementing provider prescriptions and completing tasks identified on the nursing care plan and must focus on client safety. As frontline providers, nurses are in the position to stop errors before they reach the client.
In 2000 the Institute of Medicine (IOM) issued the historic, groundbreaking report titled To Err Is Human: Building a Safer Health System. The report stated that as many as 98,000 people die in U.S. hospitals each year as a result of preventable medical errors. To Err Is Human broke the silence that previously surrounded the consequences of medical errors and set a national agenda for reducing medical errors and improving client safety through the design of a safer health system.[78] In 2007 the IOM published a follow-up report titled Preventing Medication Errors and reported that more than 1.5 million Americans are injured every year in American hospitals, and the average hospitalized client experiences at least one medication error each day. This report emphasized actions that health care systems could take to improve medication safety.[79]
The Quality and Safety Education for Nurses (QSEN) project began in 2005 to assist in preparing future nurses to continuously improve the quality and safety of the health care systems in which they work. The vision of the QSEN project is to “inspire health care professionals to put quality and safety as core values to guide their work.”[80] Nurses and nursing students are expected to participate in quality improvement (QI) initiatives by identifying gaps where change is needed and assisting in implementing initiatives to resolve these gaps. Quality improvement is defined as, “The combined and unceasing efforts of everyone – health care professionals, clients and their families, researchers, payers, planners and educators – to make the changes that will lead to better client outcomes (health), better system performance (care), and better professional development (learning).”[81]
Delegation of Interventions
While implementing interventions, RNs may elect to delegate nursing tasks. Delegation is defined by the American Nurses Association as, “The assignment of the performance of activities or tasks related to client care to unlicensed assistive personnel or licensed practical nurses (LPNs) while retaining accountability for the outcome.”[82] RNs are accountable for determining the appropriateness of the delegated task according to the condition of the client and the circumstance; the communication provided to an appropriately trained LPN or UAP; the level of supervision provided; and the evaluation and documentation of the task completed. The RN must also be aware of the state Nurse Practice Act, federal regulations, and agency policy before delegating. The RN cannot delegate responsibilities requiring clinical judgment.[83] See the following box for information regarding legal requirements associated with delegation according to the Nurse Practice Act.
Delegation According to the Wisconsin Nurse Practice Act[84]
"During the supervision and direction of delegated acts a Registered Nurse shall do all of the following:
(a) Delegate tasks commensurate with educational preparation and demonstrated abilities of the person supervised.
(b) Provide direction and assistance to those supervised.
(c) Observe and monitor the activities of those supervised.
(d) Evaluate the effectiveness of acts performed under supervision.
The standard of practice for Licensed Practical Nurses in Wisconsin states, “In the performance of acts in basic patient situations, the LPN shall, under the general supervision of an RN or the direction of a provider:
(a) Accept only patient care assignments which the LPN is competent to perform.
(b) Provide basic nursing care. Basic nursing care is defined as care that can be performed following a defined nursing procedure with minimal modification in which the responses of the patient to the nursing care are predictable.
(c) Record nursing care given and report to the appropriate person changes in the condition of a patient.
(d) Consult with a provider in cases where an LPN knows or should know a delegated act may harm a patient.
(e) Perform the following other acts when applicable:
- Assist with the collection of data.
- Assist with the development and revision of a nursing care plan.
- Reinforce the teaching provided by an RN provider and provide basic health care instruction.
- Participate with other health team members in meeting basic patient needs.”
Read additional details about the scope of practice of registered nurses (RNs) and licensed practical nurses (LPNs) in Wisconsin's Nurse Practice Act in Chapter N 6 Standards of Practice.
Read more about the American Nurses Association's Principles for Delegation.
Table 4.7 outlines general guidelines for delegating nursing tasks in the state of Wisconsin according to the role of the health care team member.
Table 4.7 General Guidelines for Delegating Nursing Tasks
| RN | LPN | CNA | |
|---|---|---|---|
| Assessment | Complete client assessment | Assist with the collection of data for stable clients | Collect measurements such as weight, input/output, and vital signs in stable clients |
| Diagnosis | Analyze assessment data and create nursing diagnoses | Not applicable | Not applicable |
| Outcome Identification | Identify SMART client outcomes | Not applicable | Not applicable |
| Planning | Plan nursing interventions | Assist with the development of a nursing care plan | Not applicable |
| Implementation of Interventions | Implement independent, dependent, and collaborative nursing interventions; delegate interventions as appropriate, with supervision; document interventions performed | Participate with other health team members in meeting basic client needs and document interventions provided
Reinforce the teaching provided by an RN provider and provide basic health care instruction |
Implement and document delegated interventions associated with basic nursing care such as providing assistance in ambulating or tasks within their scope of practice |
| Evaluation | Evaluate the attainment of outcomes and revise the nursing care plan as needed | Contribute data regarding the achievement of client outcomes; assist in the revision of a nursing care plan | Not applicable |
Documentation of Interventions
As interventions are performed, they must be documented in the client’s record in a timely manner. As previously discussed in the “Ethical and Legal Issues” subsection of the “Basic Concepts” section, lack of documentation is considered a failure to communicate and a basis for legal action. A basic rule of thumb is if an intervention is not documented, it is considered not done in a court of law. It is also important to document administration of medication and other interventions in a timely manner to prevent errors that can occur due to delayed documentation time.
Coordination of Care and Health Teaching/Health Promotion
ANA's Standard of Professional Practice for Implementation also includes the standards 5A Coordination of Care and 5B Health Teaching and Health Promotion.[85] Coordination of Care includes competencies such as organizing the components of the plan, engaging the client in self-care to achieve goals, and advocating for the delivery of dignified and holistic care by the interprofessional team. Health Teaching and Health Promotion is defined as, “Employing strategies to teach and promote health and wellness.”[86] Client education is an important component of nursing care and should be included during every client encounter. For example, client education may include teaching about side effects while administering medications or teaching clients how to self-manage their conditions at home.
Putting It Together
See an example of implementation in the following box.
Example of Implementation
Refer to Scenario C in the "Assessment" section of this chapter. The nurse implemented the nursing care plan documented in Appendix C. Interventions related to breathing were prioritized. Administration of the diuretic medication was completed first, and lung sounds were monitored frequently for the remainder of the shift. Weighing the client before breakfast was delegated to the CNA. The client was educated about her medications and methods to use to reduce peripheral edema at home. All interventions were documented in the electronic medical record (EMR).
Implementation is the fifth step of the nursing process (and the fifth Standard of Practice by the American Nurses Association). This standard is defined as, "The registered nurse implements the identified plan." The RN may delegate planned interventions after considering the circumstance, person, task, communication, supervision, and evaluation, as well as the state Nurse Practice Act, federal regulation, and agency policy.[87]
Implementation of interventions requires the RN to use critical thinking and clinical judgment. After the initial plan of care is developed, continual reassessment of the client is necessary to detect any changes in the client’s condition requiring modification of the plan. The need for continual client reassessment underscores the dynamic nature of the nursing process and is crucial to providing safe care.
During the implementation phase of the nursing process, the nurse prioritizes planned interventions, assesses client safety while implementing interventions, delegates interventions as appropriate, and documents interventions performed. LPN/VNs have an active role in the Implementation phase, provided the interventions falls within the LPN/VN scope of practice. See Figure 4.14 for an illustration of how the Implementation phase of the nursing process correlates to NCSBN's Clinical Judgment Measurement Model.[88]
Prioritizing Implementation of Interventions
Prioritizing implementation of interventions follows a similar method as to prioritizing nursing diagnoses. Maslow’s Hierarchy of Needs and the ABCs of airway, breathing, and circulation are used to establish top priority interventions. When possible, least invasive actions are usually preferred due to the risk of injury from invasive options. Read more about methods for prioritization under the “Diagnosis” section of this chapter.
The potential impact on future events, especially if a task is not completed at a certain time, is also included when prioritizing nursing interventions. For example, if a client is scheduled to undergo a surgical procedure later in the day, the nurse prioritizes initiating a NPO (nothing by mouth) prescription prior to completing pre-op client education about the procedure. The rationale for this decision is that if the client eats food or drinks water, the surgery time will be delayed. Knowing and understanding the client's purpose for care, current situation, and expected outcomes are necessary to accurately prioritize interventions.
Client Safety
It is essential to consider client safety when implementing interventions. At times, clients may experience a change in condition that makes a planned nursing intervention or provider prescription no longer safe to implement. For example, an established nursing care plan for a client states, “The nurse will ambulate the client 100 feet three times daily.” However, during assessment this morning, the client reports feeling dizzy today, and their blood pressure is 90/60. Using critical thinking and clinical judgment, the nurse decides to not implement the planned intervention of ambulating the client. This decision and supporting assessment findings should be documented in the client’s chart and also communicated during the shift handoff report, along with appropriate notification of the provider of the client’s change in condition.
Implementing interventions goes far beyond implementing provider prescriptions and completing tasks identified on the nursing care plan and must focus on client safety. As frontline providers, nurses are in the position to stop errors before they reach the client.
In 2000 the Institute of Medicine (IOM) issued the historic, groundbreaking report titled To Err Is Human: Building a Safer Health System. The report stated that as many as 98,000 people die in U.S. hospitals each year as a result of preventable medical errors. To Err Is Human broke the silence that previously surrounded the consequences of medical errors and set a national agenda for reducing medical errors and improving client safety through the design of a safer health system.[89] In 2007 the IOM published a follow-up report titled Preventing Medication Errors and reported that more than 1.5 million Americans are injured every year in American hospitals, and the average hospitalized client experiences at least one medication error each day. This report emphasized actions that health care systems could take to improve medication safety.[90]
The Quality and Safety Education for Nurses (QSEN) project began in 2005 to assist in preparing future nurses to continuously improve the quality and safety of the health care systems in which they work. The vision of the QSEN project is to “inspire health care professionals to put quality and safety as core values to guide their work.”[91] Nurses and nursing students are expected to participate in quality improvement (QI) initiatives by identifying gaps where change is needed and assisting in implementing initiatives to resolve these gaps. Quality improvement is defined as, “The combined and unceasing efforts of everyone – health care professionals, clients and their families, researchers, payers, planners and educators – to make the changes that will lead to better client outcomes (health), better system performance (care), and better professional development (learning).”[92]
Delegation of Interventions
While implementing interventions, RNs may elect to delegate nursing tasks. Delegation is defined by the American Nurses Association as, “The assignment of the performance of activities or tasks related to client care to unlicensed assistive personnel or licensed practical nurses (LPNs) while retaining accountability for the outcome.”[93] RNs are accountable for determining the appropriateness of the delegated task according to the condition of the client and the circumstance; the communication provided to an appropriately trained LPN or UAP; the level of supervision provided; and the evaluation and documentation of the task completed. The RN must also be aware of the state Nurse Practice Act, federal regulations, and agency policy before delegating. The RN cannot delegate responsibilities requiring clinical judgment.[94] See the following box for information regarding legal requirements associated with delegation according to the Nurse Practice Act.
Delegation According to the Wisconsin Nurse Practice Act[95]
"During the supervision and direction of delegated acts a Registered Nurse shall do all of the following:
(a) Delegate tasks commensurate with educational preparation and demonstrated abilities of the person supervised.
(b) Provide direction and assistance to those supervised.
(c) Observe and monitor the activities of those supervised.
(d) Evaluate the effectiveness of acts performed under supervision.
The standard of practice for Licensed Practical Nurses in Wisconsin states, “In the performance of acts in basic patient situations, the LPN shall, under the general supervision of an RN or the direction of a provider:
(a) Accept only patient care assignments which the LPN is competent to perform.
(b) Provide basic nursing care. Basic nursing care is defined as care that can be performed following a defined nursing procedure with minimal modification in which the responses of the patient to the nursing care are predictable.
(c) Record nursing care given and report to the appropriate person changes in the condition of a patient.
(d) Consult with a provider in cases where an LPN knows or should know a delegated act may harm a patient.
(e) Perform the following other acts when applicable:
- Assist with the collection of data.
- Assist with the development and revision of a nursing care plan.
- Reinforce the teaching provided by an RN provider and provide basic health care instruction.
- Participate with other health team members in meeting basic patient needs.”
Read additional details about the scope of practice of registered nurses (RNs) and licensed practical nurses (LPNs) in Wisconsin's Nurse Practice Act in Chapter N 6 Standards of Practice.
Read more about the American Nurses Association's Principles for Delegation.
Table 4.7 outlines general guidelines for delegating nursing tasks in the state of Wisconsin according to the role of the health care team member.
Table 4.7 General Guidelines for Delegating Nursing Tasks
| RN | LPN | CNA | |
|---|---|---|---|
| Assessment | Complete client assessment | Assist with the collection of data for stable clients | Collect measurements such as weight, input/output, and vital signs in stable clients |
| Diagnosis | Analyze assessment data and create nursing diagnoses | Not applicable | Not applicable |
| Outcome Identification | Identify SMART client outcomes | Not applicable | Not applicable |
| Planning | Plan nursing interventions | Assist with the development of a nursing care plan | Not applicable |
| Implementation of Interventions | Implement independent, dependent, and collaborative nursing interventions; delegate interventions as appropriate, with supervision; document interventions performed | Participate with other health team members in meeting basic client needs and document interventions provided
Reinforce the teaching provided by an RN provider and provide basic health care instruction |
Implement and document delegated interventions associated with basic nursing care such as providing assistance in ambulating or tasks within their scope of practice |
| Evaluation | Evaluate the attainment of outcomes and revise the nursing care plan as needed | Contribute data regarding the achievement of client outcomes; assist in the revision of a nursing care plan | Not applicable |
Documentation of Interventions
As interventions are performed, they must be documented in the client’s record in a timely manner. As previously discussed in the “Ethical and Legal Issues” subsection of the “Basic Concepts” section, lack of documentation is considered a failure to communicate and a basis for legal action. A basic rule of thumb is if an intervention is not documented, it is considered not done in a court of law. It is also important to document administration of medication and other interventions in a timely manner to prevent errors that can occur due to delayed documentation time.
Coordination of Care and Health Teaching/Health Promotion
ANA's Standard of Professional Practice for Implementation also includes the standards 5A Coordination of Care and 5B Health Teaching and Health Promotion.[96] Coordination of Care includes competencies such as organizing the components of the plan, engaging the client in self-care to achieve goals, and advocating for the delivery of dignified and holistic care by the interprofessional team. Health Teaching and Health Promotion is defined as, “Employing strategies to teach and promote health and wellness.”[97] Client education is an important component of nursing care and should be included during every client encounter. For example, client education may include teaching about side effects while administering medications or teaching clients how to self-manage their conditions at home.
Putting It Together
See an example of implementation in the following box.
Example of Implementation
Refer to Scenario C in the "Assessment" section of this chapter. The nurse implemented the nursing care plan documented in Appendix C. Interventions related to breathing were prioritized. Administration of the diuretic medication was completed first, and lung sounds were monitored frequently for the remainder of the shift. Weighing the client before breakfast was delegated to the CNA. The client was educated about her medications and methods to use to reduce peripheral edema at home. All interventions were documented in the electronic medical record (EMR).
Evaluation is the sixth step of the nursing process (and the sixth Standard of Practice by the American Nurses Association). This standard is defined as, “The registered nurse evaluates progress toward attainment of goals and outcomes.”[98] Both the client status and the effectiveness of the nursing care must be continuously evaluated, and the care plan modified as needed.[99]
Evaluation focuses on the effectiveness of the nursing interventions by reviewing the expected outcomes to determine if they were met by the time frames indicated. During the evaluation phase, nurses use critical thinking to analyze reassessment data and determine if a client’s expected outcomes have been met, partially met, or not met by the time frames established. If outcomes are not met or only partially met by the time frame indicated, the care plan should be revised. Reassessment should occur every time the nurse interacts with a client, discusses the care plan with others on the interprofessional team, or reviews updated laboratory or diagnostic test results. Nursing care plans should be updated as higher priority goals emerge. The results of the evaluation must be documented in the client’s medical record. Evaluation is outside the scope of practice for LPN/VNs, but they may assist in collecting reassessment data for the RN to evaluate.
Ideally, when the planned interventions are implemented, the client will respond positively, and the expected outcomes are achieved. However, when interventions do not assist in progressing the client toward the expected outcomes, the nursing care plan must be revised to more effectively address the needs of the client These questions can be used as a guide when revising the nursing care plan:
- Did anything unanticipated occur?
- Has the client’s condition changed?
- Were the expected outcomes and their time frames realistic?
- Are the nursing diagnoses accurate for this client at this time?
- Are the planned interventions appropriately focused on supporting outcome attainment?
- What barriers were experienced as interventions were implemented?
- Does ongoing assessment data indicate the need to revise diagnoses, outcome criteria, planned interventions, or implementation strategies?
- Are different interventions required?
See Figure 4.15 for a comparison of the Evaluation phase of the nursing process to the NCSBN Clinical Judgment Model.[100]
Putting It Together
See an example of the Evaluation phase in the following box.
Example of Evaluation
Refer to Scenario C in the "Assessment" section of this chapter and Appendix C. The nurse evaluates the client’s progress toward achieving the expected outcomes.
For the nursing diagnosis Excess Fluid Volume, the nurse evaluated four expected outcomes to determine if they were met during the time frames indicated:
- The client will report decreased dyspnea within the next 8 hours.
- The client will have clear lung sounds within the next 24 hours.
- The client will have decreased edema within the next 24 hours.
- The client’s weight will return to baseline by discharge.
Evaluation of the client condition on Day 1 included the following data: “The client reported decreased shortness of breath, and there were no longer crackles in the lower bases of the lungs. Weight decreased by 1 kg, but 2+ edema continued in ankles and calves.” Based on this data, the nurse evaluated the expected outcomes as "Partially Met" and revised the care plan with two new interventions:
- Request prescription for TED hose from provider.
- Elevate client's legs when sitting in chair.
For the second nursing diagnosis, Risk for Falls, the nurse evaluated the outcome criteria as "Met" based on the evaluation, “The client verbalizes understanding and is appropriately calling for assistance when getting out of bed. No falls have occurred.”
The nurse will continue to reassess the client’s progress according to the care plan during hospitalization and make revisions to the care plan as needed. Evaluation of the care plan is documented in the client’s medical record.
Evaluation is the sixth step of the nursing process (and the sixth Standard of Practice by the American Nurses Association). This standard is defined as, “The registered nurse evaluates progress toward attainment of goals and outcomes.”[101] Both the client status and the effectiveness of the nursing care must be continuously evaluated, and the care plan modified as needed.[102]
Evaluation focuses on the effectiveness of the nursing interventions by reviewing the expected outcomes to determine if they were met by the time frames indicated. During the evaluation phase, nurses use critical thinking to analyze reassessment data and determine if a client’s expected outcomes have been met, partially met, or not met by the time frames established. If outcomes are not met or only partially met by the time frame indicated, the care plan should be revised. Reassessment should occur every time the nurse interacts with a client, discusses the care plan with others on the interprofessional team, or reviews updated laboratory or diagnostic test results. Nursing care plans should be updated as higher priority goals emerge. The results of the evaluation must be documented in the client’s medical record. Evaluation is outside the scope of practice for LPN/VNs, but they may assist in collecting reassessment data for the RN to evaluate.
Ideally, when the planned interventions are implemented, the client will respond positively, and the expected outcomes are achieved. However, when interventions do not assist in progressing the client toward the expected outcomes, the nursing care plan must be revised to more effectively address the needs of the client These questions can be used as a guide when revising the nursing care plan:
- Did anything unanticipated occur?
- Has the client’s condition changed?
- Were the expected outcomes and their time frames realistic?
- Are the nursing diagnoses accurate for this client at this time?
- Are the planned interventions appropriately focused on supporting outcome attainment?
- What barriers were experienced as interventions were implemented?
- Does ongoing assessment data indicate the need to revise diagnoses, outcome criteria, planned interventions, or implementation strategies?
- Are different interventions required?
See Figure 4.15 for a comparison of the Evaluation phase of the nursing process to the NCSBN Clinical Judgment Model.[103]
Putting It Together
See an example of the Evaluation phase in the following box.
Example of Evaluation
Refer to Scenario C in the "Assessment" section of this chapter and Appendix C. The nurse evaluates the client’s progress toward achieving the expected outcomes.
For the nursing diagnosis Excess Fluid Volume, the nurse evaluated four expected outcomes to determine if they were met during the time frames indicated:
- The client will report decreased dyspnea within the next 8 hours.
- The client will have clear lung sounds within the next 24 hours.
- The client will have decreased edema within the next 24 hours.
- The client’s weight will return to baseline by discharge.
Evaluation of the client condition on Day 1 included the following data: “The client reported decreased shortness of breath, and there were no longer crackles in the lower bases of the lungs. Weight decreased by 1 kg, but 2+ edema continued in ankles and calves.” Based on this data, the nurse evaluated the expected outcomes as "Partially Met" and revised the care plan with two new interventions:
- Request prescription for TED hose from provider.
- Elevate client's legs when sitting in chair.
For the second nursing diagnosis, Risk for Falls, the nurse evaluated the outcome criteria as "Met" based on the evaluation, “The client verbalizes understanding and is appropriately calling for assistance when getting out of bed. No falls have occurred.”
The nurse will continue to reassess the client’s progress according to the care plan during hospitalization and make revisions to the care plan as needed. Evaluation of the care plan is documented in the client’s medical record.
You have now learned how to perform each step of the nursing process according to the ANA Standards of Professional Nursing Practice. Critical thinking, clinical reasoning, and clinical judgment are used when assessing the client, creating a nursing care plan, and implementing interventions. Frequent reassessment, with revisions to the care plan as needed, is important to help the client achieve expected outcomes. Throughout the entire nursing process, the client always remains the cornerstone of nursing care. Providing individualized, client-centered care and evaluating whether that care has been successful in achieving client outcomes are essential for providing safe, professional nursing practice.
Video Review of Creating a Sample Care Plan[104]
You have now learned how to perform each step of the nursing process according to the ANA Standards of Professional Nursing Practice. Critical thinking, clinical reasoning, and clinical judgment are used when assessing the client, creating a nursing care plan, and implementing interventions. Frequent reassessment, with revisions to the care plan as needed, is important to help the client achieve expected outcomes. Throughout the entire nursing process, the client always remains the cornerstone of nursing care. Providing individualized, client-centered care and evaluating whether that care has been successful in achieving client outcomes are essential for providing safe, professional nursing practice.

