Open Resources for Nursing (Open RN)
Now that we have discussed the pathophysiology of our immune system and interventions to treat and prevent infection, let’s apply this information to using the nursing process when providing client care.
Assessment
When assessing an individual who is feeling ill but has not yet been diagnosed with an infection, general symptoms associated with the prodromal period of disease may be present due to the activation of the immune system. These symptoms include a feeling of malaise (not feeling well), headache, fever, and lack of appetite. As an infection moves into the acute phase of disease, more specific signs and symptoms related to the specific type of infection will occur.
A fever is a common sign of inflammation and infection. A temperature of 38 degrees Celsius (100.4 degrees F) is generally considered a low-grade fever, and a temperature of 38.3 degrees Celsius (101 degrees F) is considered a fever.[1] As discussed earlier in this chapter, fever is part of the nonspecific innate immune response and can be beneficial in destroying pathogens. However, extremely elevated temperatures can cause cell and organ damage, and prolonged fever can cause dehydration.
Infection raises the metabolic rate, causing an increased heart rate. The respiratory rate may also increase as the body rids itself of carbon dioxide created during increased metabolism. However, be aware that an elevated heart rate above 90 and a respiratory rate above 20 are also criteria for systemic inflammatory response syndrome (SIRS) in clients with an existing infection.
As an infection develops, the lymph nodes that drain that area often become enlarged and tender. The swelling indicates that the lymphocytes and macrophages in the lymph node are fighting the infection. If a skin infection is developing, general signs of inflammation, such as redness, warmth, swelling, and tenderness, will occur at the site. As white blood cells migrate to the site, purulent drainage may occur.
Some viruses, bacteria, and toxins cause gastrointestinal inflammation, resulting in loss of appetite, nausea, vomiting, and diarrhea.
See Table 9.7a for a comparison of expected findings on physical assessment versus unexpected findings indicating a new infectious process that requires notification of the health care provider.
Table 9.7a Expected Versus Unexpected Findings on Assessment Related to Infection
| Assessment | Expected Findings | Unexpected Findings to Report to Health Care Provider |
|---|---|---|
| Vital Signs | Within normal range | New temperature over 100.4 F or 38 C. |
| Neurological | Within baseline level of consciousness | New or worsening confusion and/or worsening level of consciousness. |
| Wound or Incision | Progressive healing of a wound with no signs of infection | New or worsening redness, warmth, tenderness, or purulent drainage from a wound. |
| Respiratory | No cough or production of sputum | New or worsening cough and/or productive cough of purulent sputum. Adventitious breath sounds (crackles, rhonchi, wheezing). New or worsening dyspnea. |
| Genitourinary | Urine clear, light yellow without odor | Malodorous, cloudy, bloody urine, with increased frequency, urgency, or pain with urination. |
| Gastrointestinal | Good appetite and food intake; feces formed and brown | Loss of appetite. Nausea and vomiting. Diarrhea. Discolored or unusually malodorous feces. |
| *CRITICAL CONDITIONS requiring immediate notification of the provider and/or implementation of a sepsis protocol:
Two or more of the following criteria in a client with an existing infection indicate SIRS:
|
Life Span Considerations
Infants do not have well-developed immune systems, placing this group at higher risk of infection. Breastfeeding helps protect infants from some infectious diseases by providing passive immunity until their immune system matures. New mothers should be encouraged to breastfeed their newborns.[2]
On the other end of the continuum, the immune system gradually decreases in effectiveness with age, making older adults also more vulnerable to infection. Early detection of infection can be challenging in older adults because they may not have a fever or increased white blood cell count (WBC), but instead develop subtle changes like new mental status changes.[3] For example, new, acute confusion is a classic sign of urinary tract infection on older adults. The most common infections in older adults are urinary tract infections (UTI), bacterial pneumonia, influenza, and skin infections.
Diagnostic Tests
Several types of diagnostic tests may be ordered by a health care provider when a client is suspected of having an infection, such as complete blood count with differential, Erythrocyte Sedimentation Rate (ESR), C-Reactive Protein (CRP), serum lactate levels, and blood cultures (if sepsis is suspected). Other cultures may be obtained based on the site of the suspected infection.
CBC With Differential
When an infection is suspected, a complete blood count with differential is usually obtained.
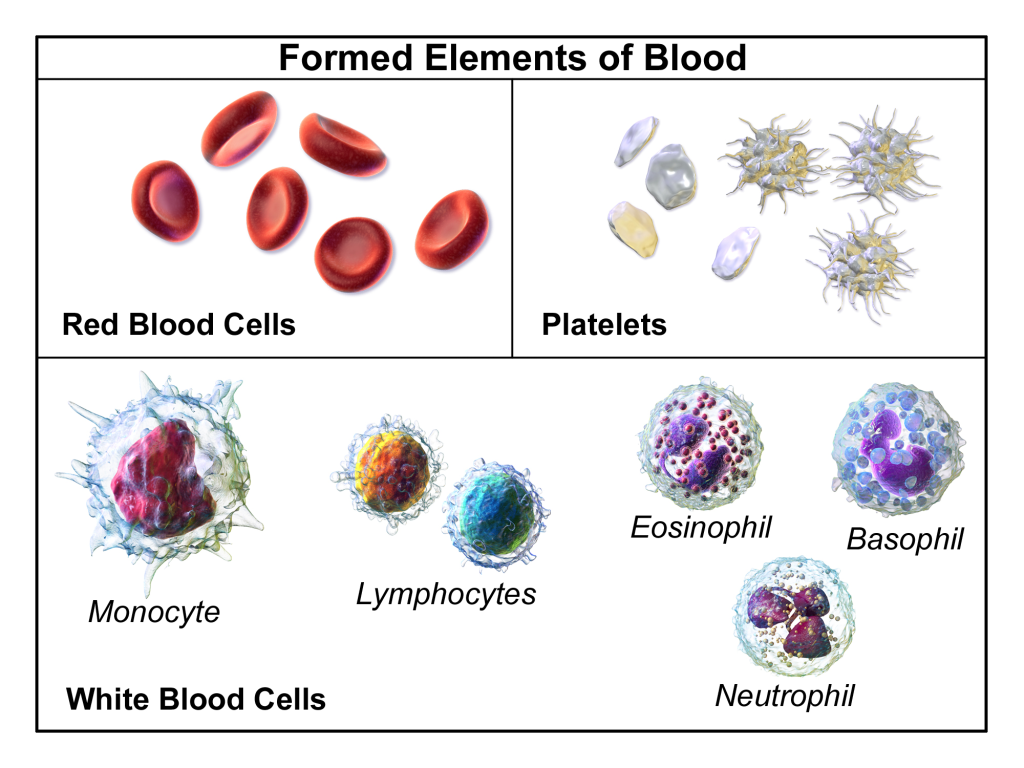
A complete blood count (CBC) includes the red blood cell count (RBC), white blood cell count (WBC), platelets, hemoglobin, and hematocrit values. A differential provides additional information, including the relative percentages of each type of white blood cell. See Figure 9.22[4] for an illustration of a complete blood count with differential.
When there is an infection or an inflammatory process somewhere in the body, the bone marrow produces more WBCs (also called leukocytes), releasing them into the blood where they move to the site of infection or inflammation. An increase in white blood cells is known as leukocytosis and is a sign of the inflammatory response. The normal range of WBC varies slightly from lab to lab but is generally 4,500-11,000 for adults, reported as 4.5-11.0 x 109 per liter (L).[5]
There are five types of white blood cells, each with different functions. The differential blood count gives the relative percentage of each type of white blood cell and also reveals abnormal white blood cells. The five types of white blood cells are as follows:
- Neutrophils
- Eosinophils
- Basophils
- Lymphocytes
- Monocytes
Neutrophils make up the largest number of circulating WBCs. They move into an area of damaged or infected tissue where they engulf and destroy bacteria or sometimes fungi.[6] An elevated neutrophil count is called neutrophilia, and decreased neutrophil count is called neutropenia.[7]
Eosinophils respond to infections caused by parasites, play a role in allergic reactions (hypersensitivities), and control the extent of immune responses and inflammation. Elevated levels of eosinophils are referred to as eosinophilia.[8]
Basophils make up the fewest number of circulating WBCs and are thought to be involved in allergic reactions.[9]
Lymphocytes include three types of cells, although the differential count does not distinguish among them:
- B lymphocytes (B cells) produce antibodies that target and destroy bacteria, viruses, and other “non-self” foreign antigens.
- T lymphocytes (T cells) mature in the thymus and consist of a few different types. Some T cells help the body distinguish between “self” and “non-self” antigens; some initiate and control the extent of an immune response, boosting it as needed and then slowing it as the condition resolves; and other types of T cells directly attack and neutralize virus-infected or cancerous cells.
- Natural killer cells (NK cells) directly attack and kill abnormal cells such as cancer cells or those infected with a virus.[10]
Monocytes, similar to neutrophils, move to an area of infection and engulf and destroy bacteria. They are associated with chronic rather than acute infections. They are also involved in tissue repair and other functions involving the immune system.[11]
Care must be taken when interpreting the results of a differential. A health care provider will consider an individual’s signs and symptoms and medical history, as well as the degree to which each type of cell is increased or decreased. A number of factors can cause a transient rise or drop in the number of any type of cell. For example, bacterial infections usually produce an increase in neutrophils, but a severe infection, like sepsis, can use up the available neutrophils, causing a low number to be found in the blood. Eosinophils are often elevated in parasitic and allergic responses. Acute viral infections often cause an increased level of lymphocytes (referred to as lymphocytosis).[12]
Erythrocyte Sedimentation Rate (ESR)
An Erythrocyte Sedimentation Rate (ESR) is a test that indirectly measures inflammation. This test measures how quickly erythrocytes or red blood cells (RBCs) settle at the bottom of a test tube that contains a blood sample. When a sample of blood is placed in a tube, the red blood cells normally settle out relatively slowly, leaving a small amount of clear plasma. The red cells settle at a faster rate when there is an increased level of proteins, such as C-reactive protein (CRP), that increases in the blood in response to inflammation. The ESR test is not diagnostic; it is a nonspecific test indicating the presence or absence of an inflammatory condition.[13]
C-Reactive Protein (CRP)
C-Reactive Protein (CRP) levels in the blood increase when there is a condition causing inflammation somewhere in the body. CRP is a nonspecific indicator of inflammation and one of the most sensitive acute phase reactants, meaning it is released into the blood within a few hours after the start of an infection or other causes of inflammation. The level of CRP can jump as much as a thousand-fold in response to a severe bacterial infection, and its rise in the blood can precede symptoms of fever or pain.[14]
Lactate
Serum lactate levels are measured when sepsis is suspected in a client with an existing infection. Sepsis can quickly lead to septic shock and death due to multi-organ failure so early recognition is crucial.
Lactate is one of the substances produced by cells as the body turns food into energy (i.e., cellular metabolism), with the highest level of production occurring in the muscles. Normally, the level of lactate in blood is low. Lactate is produced in excess by muscle cells and other tissues when there is insufficient oxygen at the cellular level, causing metabolism to change from aerobic (with oxygen) to anaerobic (without oxygen).
Lactic acid can accumulate in the body and blood when it is produced faster than the liver can break it down, which can lead to lactic acidosis. Excess lactate may be produced due to several medical conditions that cause decreased transport of oxygen to the tissues, such as sepsis, hypovolemic shock, necrotic bowel, heart attack, heart failure, or respiratory distress.[15]
Blood Culture
Blood cultures are ordered when sepsis is suspected. In many facilities, lab personnel draw the blood samples for blood cultures to avoid contamination of the sample. With some infections, pathogens are only found in the blood intermittently, so a series of three or more blood cultures, as well as blood draws from different veins, may be performed to increase the chance of finding the infection and to minimize false-positive cultures resulting from bacterial contamination of the site.
Blood cultures are incubated for several days before being reported as negative. Some types of bacteria and fungi grow more slowly than others and/or may take longer to detect if initially present in low numbers.
A positive result indicates bacteria have been found in the blood (bacteremia). Other types of pathogens, such as a fungus or a virus, may also be found in a blood culture. When a blood culture is positive, the specific microbe causing the infection is identified and susceptibility testing is performed to inform the health care provider which antibiotics or other medications are most likely to be effective for treatment.
It is important for nurses to remember that when new orders for both antibiotics and a blood culture are received, antibiotics should not be administered until after the blood culture is drawn. Administering antibiotics before the blood culture is drawn will impact the results and adversely affect the treatment plan.
Cultures and Other Diagnostic Tests
Several types of swabs and cultures may be ordered based on the site of a suspected infection, such as a nasal swab, nasopharyngeal swab, sputum culture, urine culture, and wound culture. If a lower respiratory tract infection is suspected, a chest X-ray may be ordered.
Read additional information about the following topics in Open RN Nursing Skills, 2e:
- “Specimen Collection”
- Collecting urine cultures in “Facilitation of Elimination“
- Collecting wound cultures in “Wound Care“
Therapeutic Drug Monitoring
When antibiotics are prescribed to treat an infection, some types of antibiotics require blood tests to ensure the dosage of the medication reaches and stays within therapeutic ranges in the blood. These tests are often referred to as peak and/or trough levels. A peak level refers to when the medication is at its highest concentration in the bloodstream. A trough level is when the medication is a the lowest concentration in the bloodstream, just prior to the next dose to be administered. The nurse must be aware of these orders because they impact the timing of administration of antibiotics.
Diagnoses
There are many NANDA-I nursing diagnoses applicable to infection. Nursing diagnoses associated with actual infections are customized based on the signs and symptoms of the specific infection (e.g., a client with pneumonia may have an actual nursing diagnosis of Ineffective Airway Clearance). Review a nursing care planning source for a list of current NANDA-I approved nursing diagnoses based on the type of infection occurring.[16]
Two common risk diagnoses are Risk for Infection for clients at risk for developing an infection and Risk for Shock for clients with an existing infection who are at risk for developing sepsis and septic shock. See Table 9.7b for the risk diagnoses of Risk for Infection and Risk for Shock.
Table 9.7b NANDA-I Diagnoses Associated with Infection
| NANDA-I Diagnosis | Definition | Other |
|---|---|---|
| Risk for Infection | Susceptible to invasion and multiplication of pathogenic organisms, which may compromise health
|
Risk Factors
|
| Risk of Shock | Susceptible to inadequate blood flow to the body’s tissues that may lead to life-threatening cellular dysfunction, which may compromise health
|
Associated Conditions
|
Examples
For example, a nurse caring for a client with an open wound assesses the wound regularly because clients with nonintact skin are always at increased risk for developing infection. A sample PES statement would be the following: “Risk for Infection as evidenced by alteration in skin integrity and insufficient knowledge to avoid exposure to pathogens.” The nurse plans to provide client education regarding care of the wound to prevent bacterial contamination during dressing changes.
Whenever caring for a client with an existing infection, nurses know it is important to closely monitor for signs of developing SIRS and sepsis. A sample PES statement for a client with an existing infection is as follows: “Risk for Shock as evidenced by the associated condition of infection.”
Note: Recall that in NANDA-I risk diagnoses, there are no etiological factors because a vulnerability reflects the potential for developing a problem. Read more about creating PES statements for risk diagnoses in the “Nursing Process” chapter.
Outcomes
An example of a broad goal for all clients is the following: “The client will remain free from infection during their health care stay.”[17]
An example of a SMART expected outcome to prevent infection is: “The client will demonstrate how to perform dressing changes using aseptic technique prior to discharge from the hospital.”[18]
Read more about creating SMART outcomes in the “Nursing Process” chapter.
Planning Interventions
When planning interventions for a client who is at risk for developing an infection, the nurse selects interventions such as those listed in the following box.
Interventions for Infection Prevention[19],[20]
- Monitor vital signs for signs of infection
- Monitor for early signs of localized and systemic infection for clients at risk
- Screen all visitors for communicable disease
- Encourage respiratory hygiene for clients, visitors, and staff members
- Maintain aseptic technique during nursing procedures
- Use sterile technique for invasive procedures or care of open wounds
- Use standard precautions with all clients to prevent the spread of infection
- Initiate transmission-based precautions for clients suspected of communicable infection, as appropriate
- Promote sufficient nutritional intake
- Encourage fluid intake, as appropriate
- Encourage rest
- Encourage frequent ambulation or turn immobilized clients frequently
- Ensure appropriate hygienic care, including proper hand hygiene, daily bathing, oral care, and perineal care performed by either the nurse or the client, as appropriate
- Moisturize dry skin to keep it intact
- Use strategies to prevent healthcare-acquired respiratory infection, such as incentive spirometry, coughing and deep breathing, positional changes, and early ambulation as appropriate
- Use strategies to prevent wound infection such as changing saturated dressings to reduce the potential reservoir of bacteria
- Teach the client and family members the importance of a nutritious diet, exercise, and adequate rest to promote healing and health at home
- Teach the client and family about signs and symptoms of infection and when to report them to the health care provider
- Encourage the annual influenza vaccine and keeping other recommended vaccinations up-to-date
- If a client smokes, encourage smoking cessation because smoking damages the mucociliary escalator and places the client at increased risk for infection
- Report signs and symptoms of suspected infection or sepsis to the health care provider
- Suspect an infection if an older adult client has new signs of lethargy or confusion
If a client has an infection with a fever, the nursing diagnosis Hyperthermia may be applicable. See the following box for interventions for clients with fever/hyperthermia.
Interventions for Hyperthermia
- Assess for associated symptoms such as diaphoresis, shaking chills (rigors)
- Monitor level of consciousness
- Adjust room temperature to the client’s comfort without inducing chilling
- Administer antipyretics, as appropriate (e.g., acetaminophen, ibuprofen)
- Apply external cooling methods as needed (cold packs or cool sponge bath)
- Encourage fluid intake
- Monitor for signs of dehydration
Implementing Interventions
When caring for a client with an active infection, transmission-based precautions may be required based on the specific type of pathogen. Antibiotics and/or other antimicrobials are administered as prescribed, and the client and family are instructed how to take prescribed antibiotics with measures to prevent antibiotic resistance (i.e., complete prescribed length of therapy even if they feel better in a few days).
If cultures have been obtained, it is important to monitor and report new results to the provider to ensure the prescribed antibiotic therapy is appropriate based on susceptibility results.
It is important to continually monitor clients with an existing infection for signs of SIRS/sepsis:
- Carefully monitor vital signs. Immediately notify the provider for two or more of the following indicators that suggest SIRS: heart rate greater than 90 beats per minute, temperature greater than 38 degrees C or less than 36 degrees C, systolic blood pressure less than 90 mm Hg, respiratory rate greater than 20, or a white blood cell count greater than 12,000 or less than 4,000.[21] Anticipate new orders for a lactate level and blood cultures for early diagnosis of sepsis.
- Monitor for signs of new decreased mental status, especially in older adults, that can indicate decreased oxygenation or tissue perfusion associated with sepsis and septic shock.
- For clients presenting with early signs of shock, administer oxygen immediately to maintain oxygen saturation greater than 90%. Administer prescribed antibiotics within an hour after diagnosis for improved survival. Be aware that IV fluids and vasopressor medications may be required to treat shock.[22]
Evaluation
It is always important to evaluate the effectiveness of interventions used to prevent and treat infection. Evaluation helps the nurse determine whether the established outcomes have been met and if the planned interventions are still appropriate for the client at the time of implementation. If outcomes are not met, interventions may need to be added or revised to help the client meet their goals.
- Abad, C., Fearday, A., & Safdar, N. (2010). Adverse effects of isolation in hospitalised patients: A systematic review. The Journal of Hospital Infection, 76(2), 97-102. https://doi.org/10.1016/j.jhin.2010.04.027 ↵
- Centers for Disease Control and Prevention. (2020, May 28). Breastfeeding, Frequently asked questions (FAQs). https://www.cdc.gov/breastfeeding/faq/index.htm ↵
- Centers for Disease Control and Prevention. (2020, May 28). Breastfeeding, Frequently asked questions (FAQs). https://www.cdc.gov/breastfeeding/faq/index.htm ↵
- “Blausen_0425_Formed_Elements.png” by BruceBlaus.com staff is licensed under CC BY 3.0 ↵
- Centers for Disease Control and Prevention. (2021, January 19). Candida auris. https://www.cdc.gov/fungal/candida-auris/index.html ↵
- Centers for Disease Control and Prevention. (2021, January 19). Candida auris. https://www.cdc.gov/fungal/candida-auris/index.html ↵
- LabTestsOnline.org. (2021, January 27). White blood cell count (WBC). https://labtestsonline.org/tests/white-blood-cell-count-wbc ↵
- LabTestsOnline.org. (2021, January 27). White blood cell count (WBC). https://labtestsonline.org/tests/white-blood-cell-count-wbc ↵
- LabTestsOnline.org. (2021, January 27). White blood cell count (WBC). https://labtestsonline.org/tests/white-blood-cell-count-wbc ↵
- LabTestsOnline.org. (2021, January 27). White blood cell count (WBC). https://labtestsonline.org/tests/white-blood-cell-count-wbc ↵
- LabTestsOnline.org. (2021, January 27). White blood cell count (WBC). https://labtestsonline.org/tests/white-blood-cell-count-wbc ↵
- LabTestsOnline.org. (2021, January 27). White blood cell count (WBC). https://labtestsonline.org/tests/white-blood-cell-count-wbc ↵
- LabTestsOnline.org. (2020, July 29). Erythrocyte sedimentation rate (ESR). https://labtestsonline.org/tests/erythrocyte-sedimentation-rate-esr ↵
- LabTestsOnline.org. (2020, August 12). C-Reactive protein (CRP). https://labtestsonline.org/tests/c-reactive-protein-crp ↵
- LabTestsOnline.org. (2020, August 12). Lactate. https://labtestsonline.org/tests/lactate ↵
- Herdman, T., & Kamitsuru, S. (2017). NANDA international nursing diagnoses: Definitions & classification 2018-2020 (11th ed.). Thieme Publishers. pp. 382, 405. ↵
- Centers for Disease Control and Prevention. (2016, January 26). Standard precautions for all patient care. https://www.cdc.gov/infectioncontrol/basics/standard-precautions.html ↵
- Johnson, M., Moorhead, S., Bulechek, G., Butcher, H., Maas, M., & Swanson, E. (2012). NOC and NIC linkages to NANDA-I and clinical conditions: Supporting critical reasoning and quality care. Elsevier. p. 268. ↵
- Butcher, H., Bulechek, G., Dochterman, J., & Wagner, C. (2018). Nursing interventions classification (NIC). Elsevier. pp. 214, 226-227, 346. ↵
- Wilson, J., Bak, A., & Loveday, H. P. (2017, March 29). Applying human factors and ergonomics to the misuse of nonsterile clinical gloves in acute care. American Journal of Infection Control, 45(7), 779-786. https://doi.org/10.1016/j.ajic.2017.02.019. ↵
- Herdman, T., & Kamitsuru, S. (2017). NANDA international nursing diagnoses: Definitions & classification 2018-2020 (11th ed.). Thieme Publishers. pp. 382, 405. ↵
- This work is a derivative of StatPearls by Chakraborty & Burns and is licensed under CC BY 4.0 ↵
In addition to recognizing signs of infection and educating clients about the treatment of their infection, nurses also play an important role in preventing the spread of infection. A cyclic process known as the chain of infection describes the transmission of an infection. By implementing interventions to break one or more links in the chain of infection, the spread of infection can be stopped. See Figure 9.16[1] for an illustration of the links within the chain of infection. These links are described as the following[2]:
- Infectious Agent: A causative organism, such as bacteria, virus, fungi, parasite.
- Reservoir: A place where the organism grows, such as in blood, food, or a wound.
- Portal of Exit: The method by which the organism leaves the reservoir, such as through respiratory secretions, blood, urine, breast milk, or feces.
- Mode of Transmission: The vehicle by which the organism is transferred such as physical contact, inhalation, or injection. The most common vehicles are respiratory secretions spread by a cough, sneeze, or on the hands. A single sneeze can send thousands of virus particles into the air.
- Portal of Entry: The method by which the organism enters a new host, such as through mucous membranes or nonintact skin.
- Susceptible Host: The susceptible individual the organism has invaded.
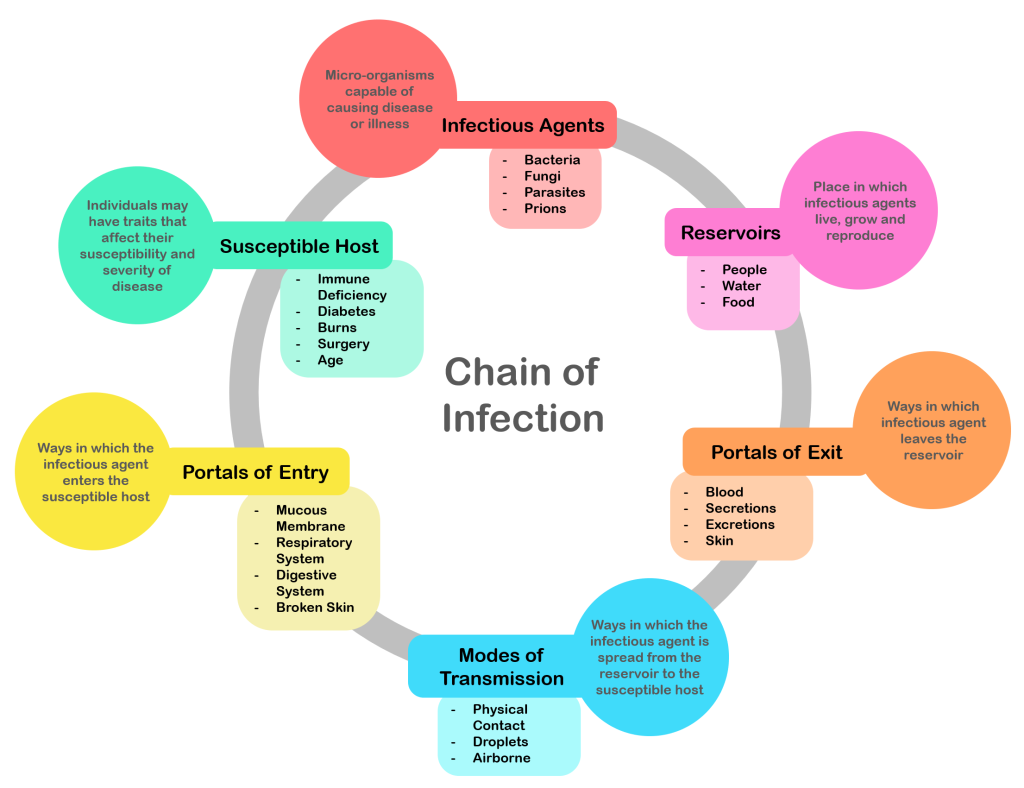
For a pathogen to continue to exist, it must put itself in a position to be transmitted to a new host, leaving the infected host through a portal of exit. Similar to portals of entry, the most common portals of exit include the skin and the respiratory, urogenital, and gastrointestinal tracts. Coughing and sneezing can expel thousands of pathogens from the respiratory tract into the environment. Other pathogens are expelled through feces, urine, semen, and vaginal secretions. Pathogens that rely on insects for transmission exit the body in the blood extracted by a biting insect.[3]
The pathogen enters a new individual via a portal of entry, such as mucous membranes or nonintact skin. If the individual has a weakened immune system or their natural defenses cannot fend off the pathogen, they become infected.
Interventions to Break the Chain of Infection
Infections can be stopped from spreading by interrupting this chain at any link. Chain links can be broken by disinfecting the environment, sterilizing medical instruments and equipment, covering coughs and sneezes, using good hand hygiene, implementing standard and transmission-based precautions, appropriately using personal protective equipment, encouraging clients to stay up-to-date on vaccines (including the flu shot), following safe injection practices, and promoting the optimal functioning of the natural immune system with good nutrition, rest, exercise, and stress management.
Disinfection and Sterilization
Disinfection and sterilization are used to kill microorganisms and remove harmful pathogens from the environment and equipment to decrease the chance of spreading infection. Disinfection is the removal of microorganisms. However, disinfection does not destroy all spores and viruses. Sterilization is a process used on equipment and the environment to destroy all pathogens, including spores and viruses. Sterilization methods include steam, boiling water, dry heat, radiation, and chemicals. Because of the harshness of these sterilization methods, skin can only be disinfected and not sterilized.[4]
Standard and Transmission-Based Precautions
To protect clients and health care workers from the spread of pathogens, the CDC has developed precautions to use during client care that address portals of exit, methods of transmission, and portals of entry. These precautions include standard precautions and transmission-based precautions.
Standard Precautions
Standard precautions are used when caring for all clients to prevent healthcare-associated infections. According to the Centers for Disease Control and Prevention (CDC), standard precautions are the minimum infection prevention practices that apply to all client care, regardless of suspected or confirmed infection status of the client, in any setting where health care is delivered. These precautions are based on the principle that all blood, body fluids (except sweat), nonintact skin, and mucous membranes may contain transmissible infectious agents. These standards reduce the risk of exposure for the health care worker and protect the client from potential transmission of infectious organisms.[5] See Figure 9.17[6] for an image of some of the components of standard precautions.
Current standard precautions according to the CDC include the following:
- Appropriate hand hygiene
- Use of personal protective equipment (e.g., gloves, gowns, masks, eyewear) whenever infectious material exposure may occur
- Appropriate client placement and care using transmission-based precautions when indicated
- Respiratory hygiene/cough etiquette
- Proper handling and cleaning of environment, equipment, and devices
- Safe handling of laundry
- Sharps safety (i.e., engineering and work practice controls)
- Aseptic technique for invasive nursing procedures such as parenteral medication administration[7]
![]“hand-disinfection-4954840_960_720.jpg” by KlausHausmann is licensed under CC0 Image showing hand sanitizer, gloves, and a surgical mask](https://open.maricopa.edu/app/uploads/sites/683/2024/09/hand-sanitizer-300x201.png)
Hand Hygiene
Hand hygiene, although simple, is still the best and most effective way to prevent the spread of infection. The 2021 National Patient Safety Goals from The Joint Commission encourages infection prevention strategy practices such as implementing the hand hygiene guidelines from the Centers for Disease Control.[8] Accepted methods for hand hygiene include using either soap and water or alcohol-based hand sanitizer. It is essential for all health care workers to use proper hand hygiene at the appropriate times, such as the following:
- Immediately before touching a client
- Before performing an aseptic task or handling invasive devices
- Before moving from a soiled body site to a clean body site on a client
- After touching a client or their immediate environment
- After contact with blood, body fluids, or contaminated surfaces (with or without glove use)
- Immediately after glove removal[9]
Hand hygiene also includes health care workers keeping their nails short with tips less than 0.5 inches and no nail polish. Nails should be natural, and artificial nails or tips should not be worn. Artificial nails and chipped nail polish have been associated with a higher level of pathogens carried on the hands of the nurse despite hand hygiene.[10]
Respiratory Hygiene/Cough Etiquette
Respiratory hygiene is targeted at clients, accompanying family members and friends, and staff members with undiagnosed transmissible respiratory infections. It applies to any person with signs of illness, including cough, congestion, or increased production of respiratory secretions when entering a health care facility. The elements of respiratory hygiene include the following:
- Education of health care facility staff, clients, and visitors
- Posted signs, in language(s) appropriate to the population served, with instructions to clients and accompanying family members or friends
- Source control measures for a coughing person (e.g., covering the mouth/nose with a tissue when coughing and prompt disposal of used tissues, or applying surgical masks on the coughing person to contain secretions)
- Hand hygiene after contact with one’s respiratory secretions
- Spatial separation, ideally greater than three feet, of persons with respiratory infections in common waiting areas when possible[11]
Health care personnel are advised to wear a mask and use frequent hand hygiene when examining and caring for clients with signs and symptoms of a respiratory infection. Health care personnel who have a respiratory infection are advised to stay home or avoid direct client contact, especially with high-risk clients. If this is not possible, then a mask should be worn while providing client care.[12]
Personal Protective Equipment
Personal Protective Equipment (PPE) includes gloves, gowns, face shields, goggles, and masks used to prevent the spread of infection to and from clients and health care providers. See Figure 9.18[13] for an image of a nurse wearing PPE. Depending upon the anticipated exposure and type of pathogen, PPE may include the use of gloves, a fluid-resistant gown, goggles or a face shield, and a mask or respirator. When used while caring for a client with transmission-based precautions, PPE supplies are typically stored in an isolation cart next to the client’s room.

Transmission-Based Precautions
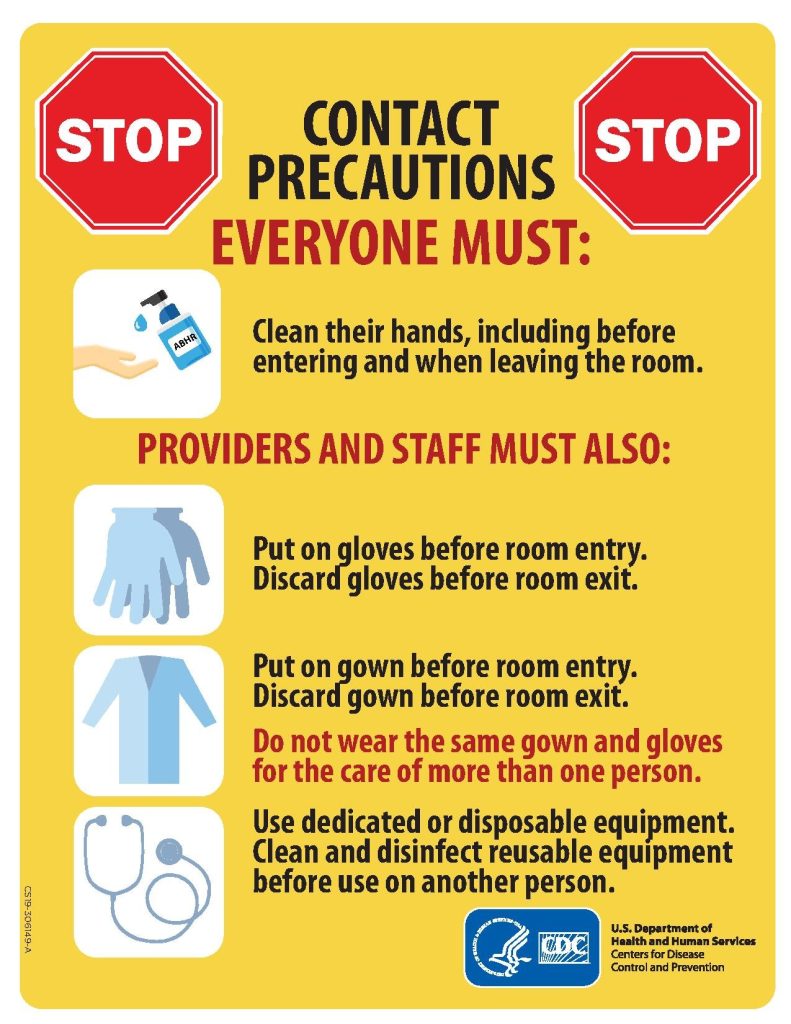
In addition to standard precautions, transmission-based precautions are used for clients with documented or suspected infection of highly transmissible pathogens, such as C. difficile (C-diff), Methicillin-resistant Staphylococcus aureus (MRSA), Vancomycin-resistant enterococci (VRE), Respiratory Syncytial Virus (RSV), measles, and tuberculosis (TB). For clients with these types of pathogens, standard precautions are used along with specific transmission-based precautions.[14]
There are three categories of transmission-based precautions: contact precautions, droplet precautions, and airborne precautions. Transmission-based precautions are used when the route(s) of transmission of a specific disease are not completely interrupted using standard precautions alone.
Some diseases, such as tuberculosis, have multiple routes of transmission so more than one transmission-based precaution category must be implemented. See Table 9.6 outlining the categories of transmission precautions with associated PPE and other precautions. When possible, clients with transmission-based precautions should be placed in a single occupancy room with dedicated client care equipment (e.g., blood pressure cuffs, stethoscope, and thermometer stay in the client’s room). A card is posted outside the door alerting staff and visitors to required precautions before entering the room. See Figure 9.19[15] for an example of signage used for a client with contact precautions. Transport of the clientand unnecessary movement outside the client room should be limited. When transmission-based precautions are implemented, it is also important for the nurse to make efforts to counteract possible adverse effects of these precautions on clients, such as anxiety, depression, perceptions of stigma, and reduced contact with clinical staff.[16]
Table 9.6 Transmission-Based Precautions[17]
| Precaution | Implementation | PPE and Other Precautions |
|---|---|---|
| Contact | Known or suspected infections with increased risk for contact transmission (e.g., draining wounds, fecal incontinence) or with epidemiologically important organisms, such as C-diff, MRSA, VRE, or RSV | Gloves
Gown Dedicated equipment Limit client transport out of room Prioritized disinfection of the room Note: Use only soap and water for hand hygiene in clients with C. difficile infection. |
| Droplet | Known or suspected infection with pathogens transmitted by large respiratory droplets generated by coughing, sneezing, or talking, such as influenza or pertussis | Mask
Goggles or face shield Dedicated equipment |
| Airborne | Known or suspected infection with pathogens transmitted by small respiratory droplets that travel through the air, such as measles and coronavirus | Fit-tested N-95 respirator
Airborne infection isolation room Single-client room Client door closed Restricted susceptible personnel room entry Dedicated equipment |
Client Transport
Several principles are used to guide transport of clients requiring transmission-based precautions. During inpatient and residential settings, these principles include the following:
- Limit transport for essential purposes only, such as diagnostic and therapeutic procedures that cannot be performed in the client’s room
- When transporting, use appropriate barriers on the client consistent with the route and risk of transmission (e.g., mask, gown, covering the affected areas when infectious skin lesions or drainage is present)
- Notify health care personnel in the receiving area of the impending arrival of the client and of the precautions necessary to prevent transmission[18]
Enteric Precautions
Enteric precautions are used when there is the presence, or suspected presence, of gastrointestinal pathogens such as Clostridium difficile (C-diff) or norovirus. These pathogens are present in feces, so health care workers should always wear a gown in the client room to prevent inadvertent fecal contamination of their clothing from contact with contaminated surfaces.
In addition to contact precautions, enteric precautions include the following:
- Using only soap and water for hand hygiene. Do not use hand sanitizer because it is not effective against C-diff spores.
- Using a special disinfecting process. Special disinfecting should be used after client discharge and includes disinfection of the mattress.
Reverse Isolation
Reverse isolation, also called neutropenic precautions, is used for clients who have compromised immune systems and low neutrophil levels. This type of isolation protects the client from pathogens in their environment. In addition to using contact precautions to protect the client, reverse isolation precautions include the following:
- Meticulous hand hygiene by all visitors, staff, and the client
- Frequently monitoring for signs and symptoms of infection and sepsis
- Not allowing live plants, fresh flowers, fresh raw fruits or vegetables, sushi, deli foods, or cheese into the room due to bacteria and fungi
- Placement in a private room or a positive pressure room
- Limited transport and movement of the client outside of the room
- Masking of the client for transport with a surgical mask[19]
Psychological Effects of Isolation
Although the use of transmission-based precautions is needed to prevent the spread of infection, it is important for nurses to be aware of the potential psychological impact on the client. Research has shown that isolation can cause negative impact on client mental well-being and behavior, including higher scores for depression, anxiety, and anger among isolated clients. It has also been found that health care workers spend less time with clients in isolation, resulting in a negative impact on client safety.[20]
Client and family education at the time of instituting transmission-based precautions is a critical component of the process to reduce anxiety and distress. Clients often feel stigmatized when placed in isolation, so it is important for them to understand the rationale of the precautions to keep themselves and others free from the spread of disease. Preparing clients emotionally will also help decrease their anxiety and help them cope with isolation.[21] It is also important to provide distractions from boredom, such as music, television, video games, magazines, or books, as appropriate. Simple actions, such as charting while in the client's room, can also increase nurse-client interaction time.
Aseptic and Sterile Techniques
In addition to using standard precautions and transmission-based precautions, aseptic technique (also called medical asepsis) is used to prevent the transfer of microorganisms from one person or object to another during a medical procedure. For example, a nurse administering parenteral medication or performing urinary catheterization uses aseptic technique. When performed properly, aseptic technique prevents contamination and transfer of pathogens to the client from caregiver hands, surfaces, and equipment during routine care or procedures. It is important to remember that potentially infectious microorganisms can be present in the environment, on instruments, in liquids, on skin surfaces, or within a wound.[22]
There is often misunderstanding between the terms aseptic technique and sterile technique in the health care setting. Both asepsis and sterility are closely related with the shared concept being the removal of harmful microorganisms that can cause infection. In the most simplistic terms, aseptic technique involves creating a protective barrier to prevent the spread of pathogens, whereas sterile technique is a purposeful attack on microorganisms. Sterile technique (also called surgical asepsis) seeks to eliminate every potential microorganism in and around a sterile field while also maintaining objects as free from microorganisms as possible. Sterile fields are implemented during surgery, as well as during nursing procedures such as the insertion of a urinary catheter, changing dressings on open wounds, and performing central line care. See Figure 9.20[23] for an image of a sterile field during surgery. Sterile technique requires a combination of meticulous handwashing, creating and maintaining a sterile field, using long-lasting antimicrobial cleansing agents such as Betadine, donning sterile gloves, and using sterile devices and instruments.[24]

Read additional information about aseptic and sterile technique in the "Aseptic Technique" in Open RN Nursing Skills, 2e.
Read a continuing education article about Sterile Technique and surgical scrubbing.
Other Hygienic Client Care Interventions
In addition to implementing standard and transmission-based precautions and utilizing aseptic and sterile technique when performing procedures, nurses implement many interventions to place a client in the best health possible to prevent an infection or treat infection. These interventions include actions like encouraging rest and good nutrition, teaching stress management, providing good oral care, encouraging daily bathing, and changing linens. It is also important to consider how gripper socks, mobile devices, and improper glove usage can contribute to the transmission of pathogens.
Oral Care
Client hygiene is important in the prevention and spread of infection. Although oral care may be given a low priority, research has found that poor oral care is associated with the spread of infection, poor health outcomes, and poor nutrition. Oral care should be performed in the morning, after meals, and before bed.[25]
Daily Bathing
Daily bathing is another intervention that may be viewed as time-consuming and receive low priority, but it can have a powerful impact on decreasing the spread of infection. Studies have shown a significant decrease in healthcare-associated infections with daily bathing using chlorhexidine gluconate (CHG) wipes or solution. The use of traditional soap and water baths do not reduce infection rates as significantly as CHG products, and wash basins have also been shown to be a reservoir for pathogens.[26]
Linens
Changing bed linens, towels, and a gown regularly eliminates potential reservoirs of bacteria. Fresh linens also promote client comfort.
Gripper Socks
Have you ever thought about what happens to the bed linens when a client returns from a walk in the hallway with gripper socks and gets back into bed with these socks? Research demonstrates that pathogens from the floor are transferred to the client's bed linens from the gripper socks. Nurses should remove gripper socks that were used for walking before clients climb into bed. They should also throw the socks away when the client is discharged instead of sending them home.[27]
Cellular Phones and Mobile Devices
Research has shown that cell phones and mobile devices carry many pathogens and are dirtier than a toilet seat or the bottom of a shoe. Clients, staff, and visitors routinely bring these mobile devices into health care facilities, which can cause the spread of disease. Nurses should frequently wipe mobile devices with disinfectant. They should encourage clients and visitors to disinfect phones frequently and avoid touching the face after having touched a mobile device.[28]
Gloves
Although gloves are used to prevent the spread of infection, they can also contribute to the spread of infection if used improperly. For example, research has shown that hand hygiene opportunities are being missed because of the overuse of gloves. For example, a nurse may don gloves to suction a client but neglect to remove them and perform hand hygiene before performing the next procedure on the same client. This can potentially cause the spread of secondary infection. The World Health Organization (WHO) states that gloves should be worn when there is an expected risk of exposure to blood or body fluids or to protect the hands from chemicals and hazardous drugs, but hand hygiene is the best method of disease prevention and is preferred over wearing gloves when the exposure risk is minimal. Nurses have the perception that wearing gloves provides extra protection and cleanliness. However, the opposite is true. Nonsterile gloves have a high incidence of contamination with a range of bacteria, which means that a gloved hand is dirtier than a washed hand. Research has shown that nearly 40% of the times that gloves are used in client care, there is cross contamination. The most striking example of cross contamination includes situations when gloves are used for toileting a client and not being removed before touching other surfaces or the client.[29],[30],[31]
Glove-related contact dermatitis has also become an important issue in recent years as more and more nurses are experiencing damage to the hands. Contact dermatitis can develop from repeated use of gloves and develops as dry, itchy, irritated areas on the skin of the hands. See Figure 9.21[32] for an image of contact dermatitis from gloves. Because the skin is the first line of defense in preventing pathogens from entering the body, maintaining intact skin is very important to prevent nurses from exposure to pathogens.


